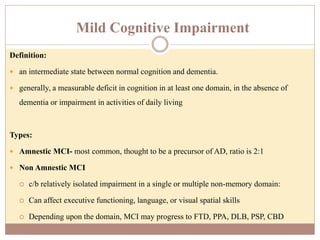
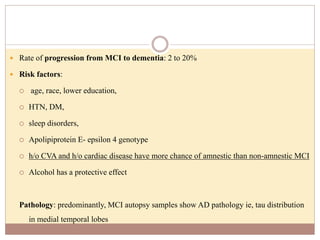
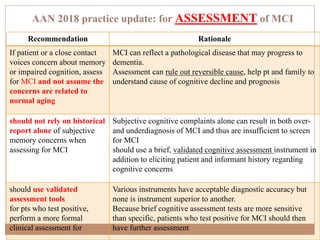
This document provides guidelines for assessing and managing mild cognitive impairment (MCI). It defines MCI as a state between normal cognition and dementia, involving measurable deficits in at least one cognitive domain with no impairment in daily living. There are two main types: amnestic MCI, which is often a precursor to Alzheimer's disease, and non-amnestic MCI affecting other domains. The guidelines recommend using validated cognitive assessment tools in addition to patient/informant reports to diagnose MCI, and assessing for functional impairment before diagnosing dementia. They also suggest monitoring patients over time, treating modifiable risk factors, and discussing uncertainties around prognosis and long-term planning with patients and families.