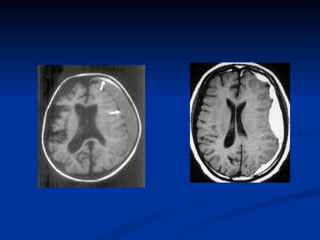
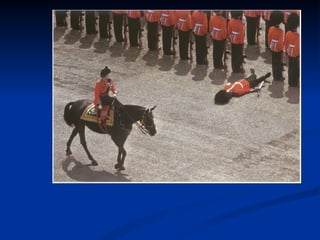
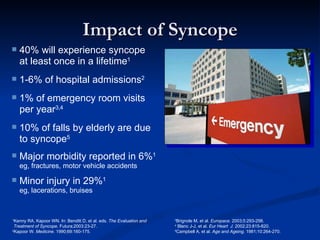
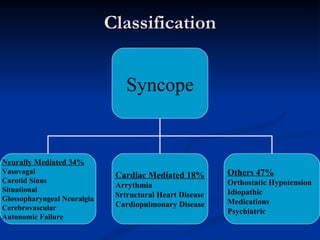
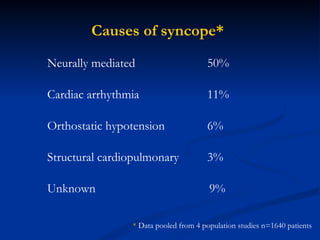
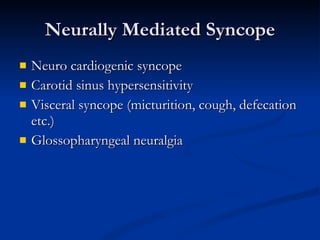
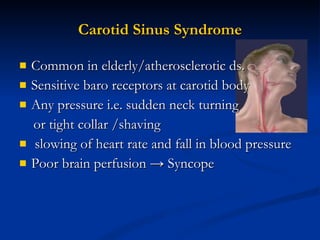
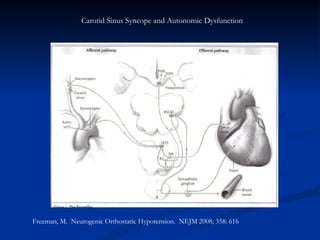
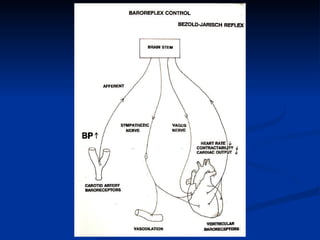
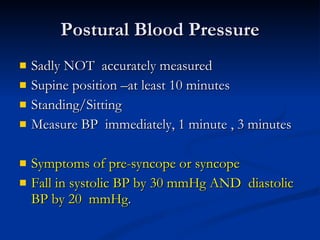
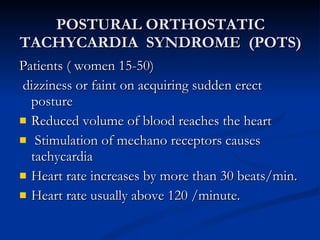
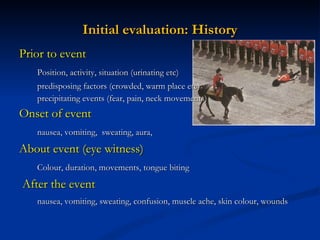
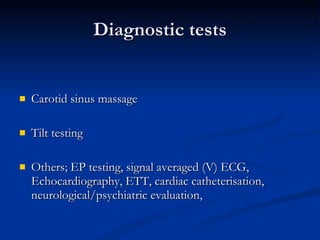
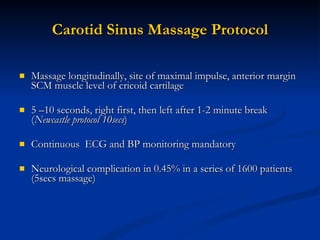
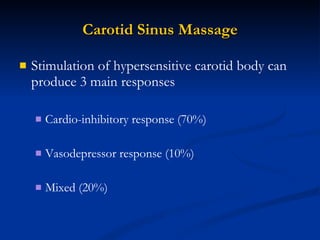
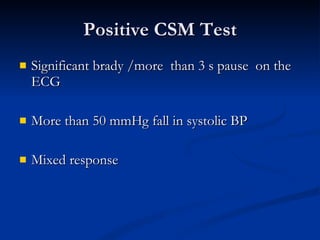
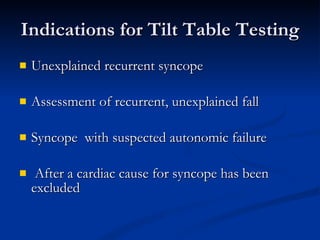
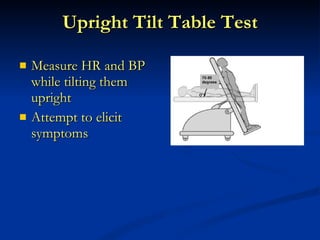
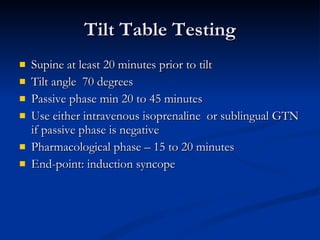
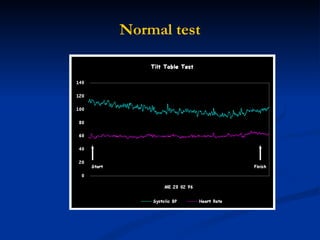
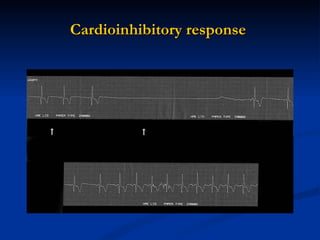
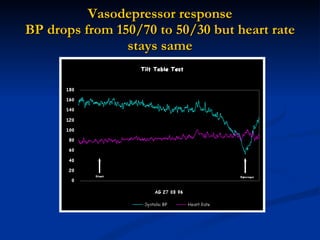
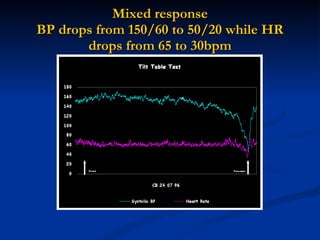
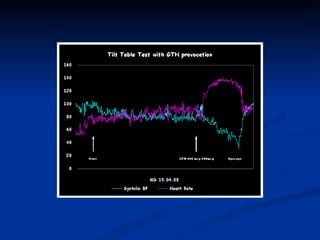
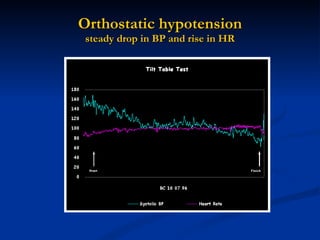
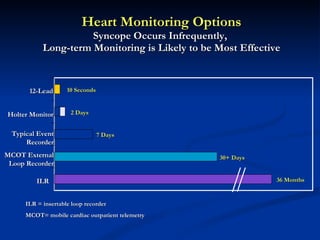
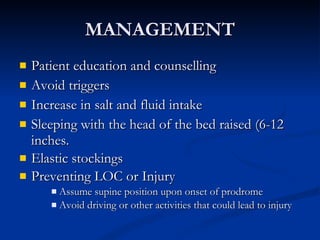
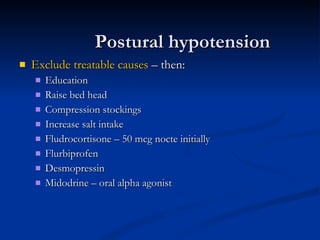
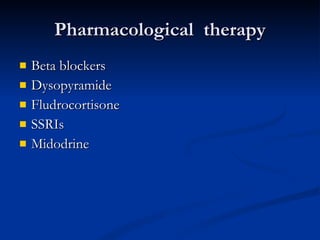
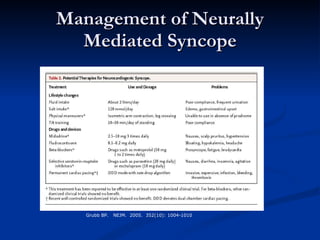
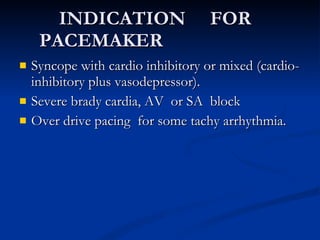
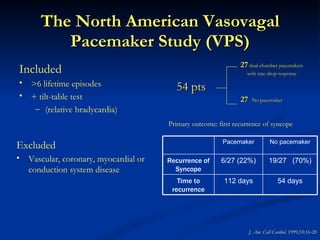
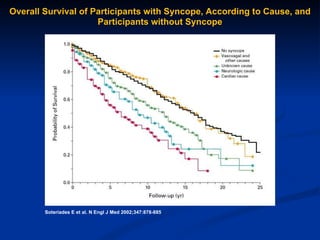
Syncope, or fainting, is a relatively common problem that is often misdiagnosed. It is caused by a temporary drop in blood pressure and loss of consciousness. The most common causes are neurally-mediated syncope, cardiac arrhythmias, and orthostatic hypotension. A thorough history, physical exam, and diagnostic tests like carotid sinus massage and tilt table testing can help identify the underlying cause. Treatment depends on the cause but may include lifestyle changes, medications, or pacemaker implantation in severe cases. Proper diagnosis and management of syncope is important as it can occasionally lead to injuries or accidents.