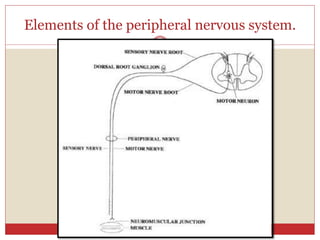
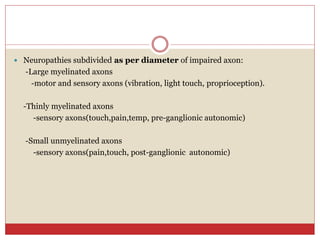
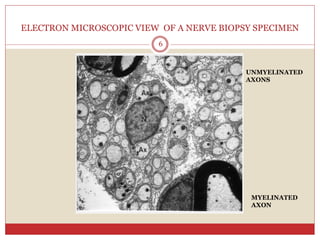
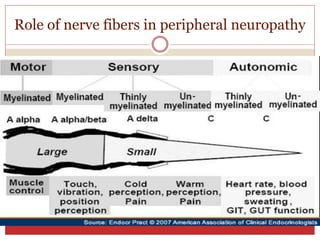
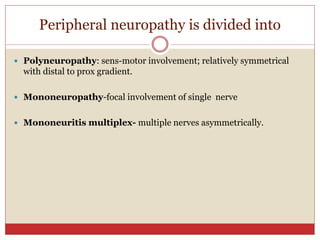
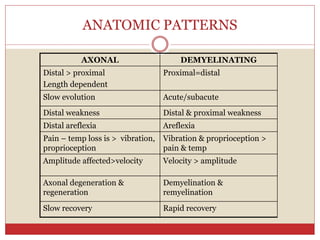
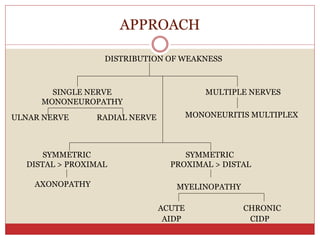
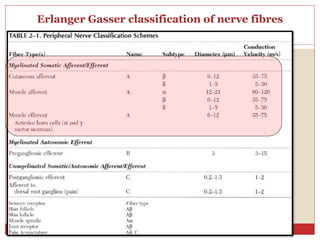
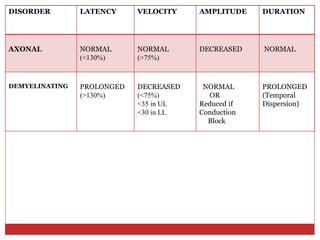
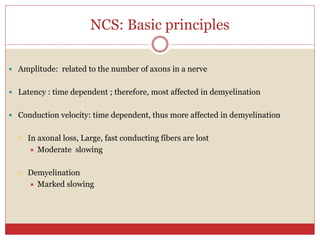
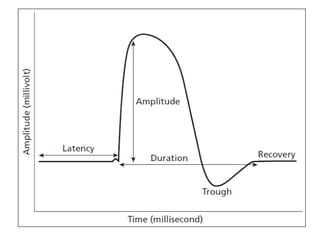
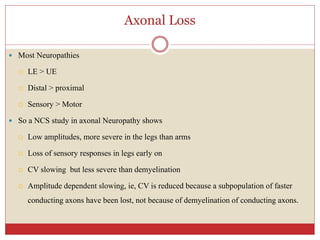
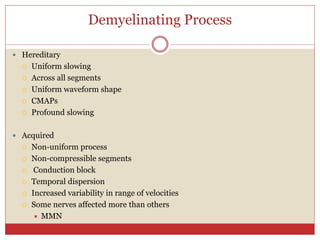
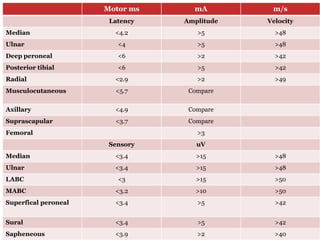
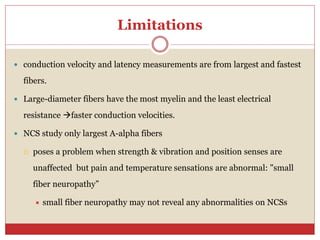
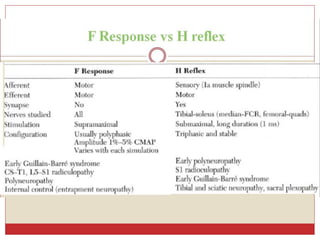
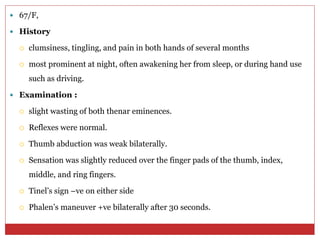
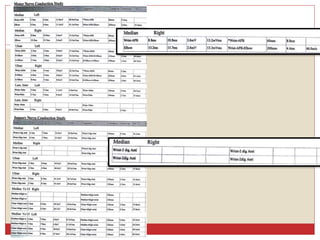
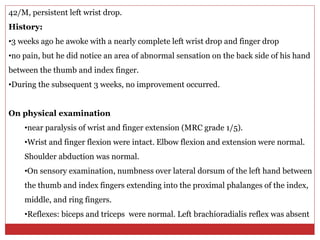
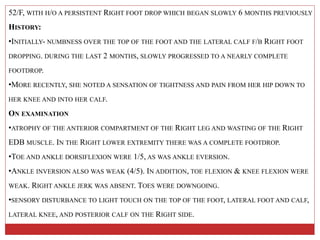
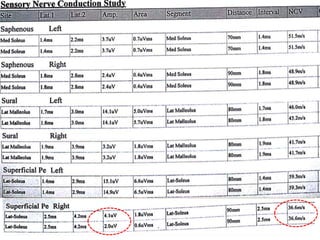
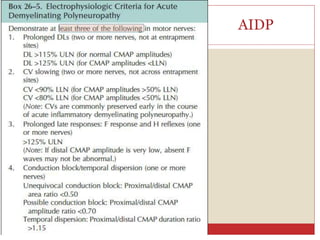
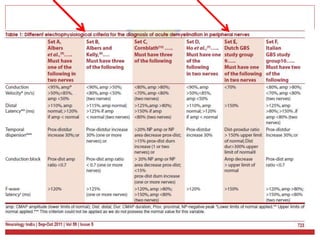
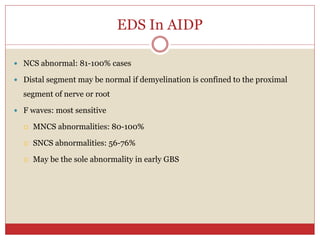
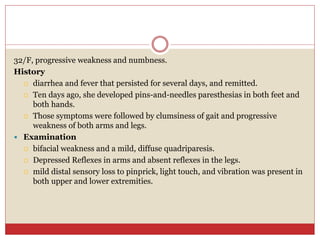
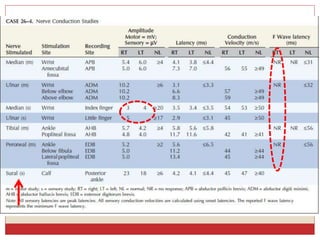
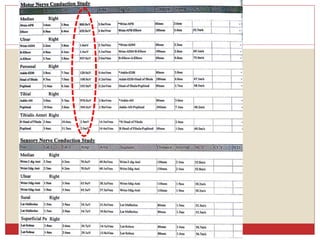
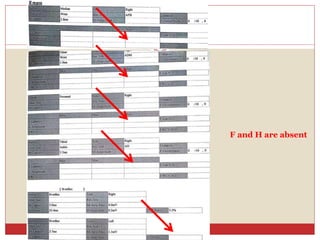
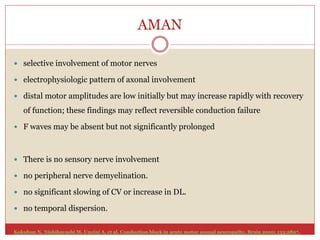
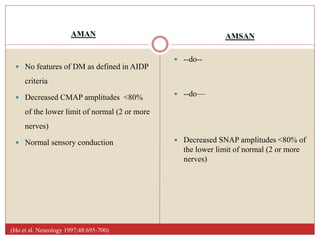
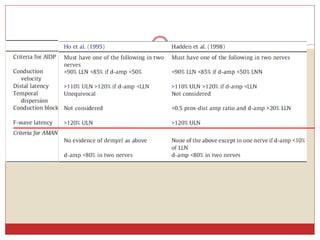
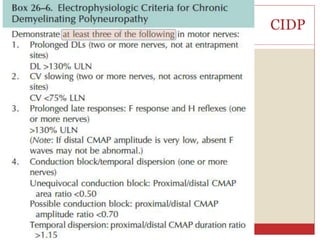
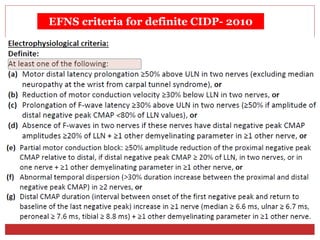
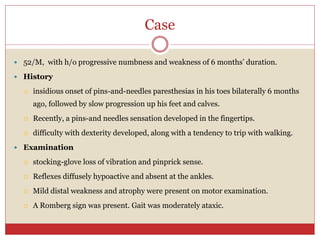
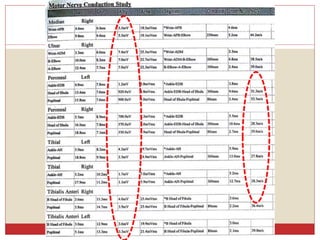
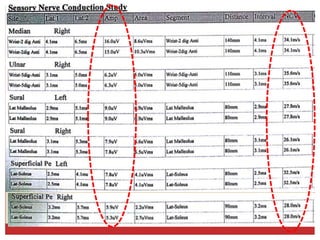
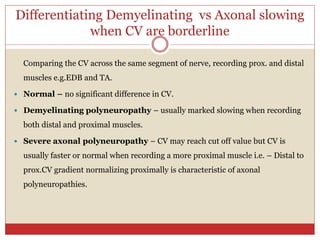
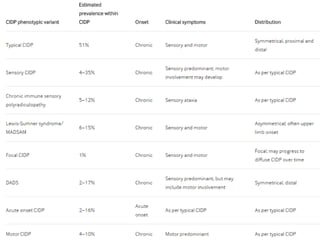
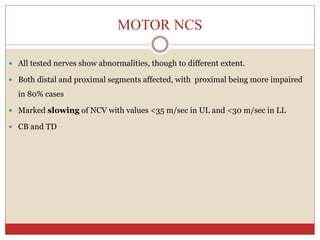
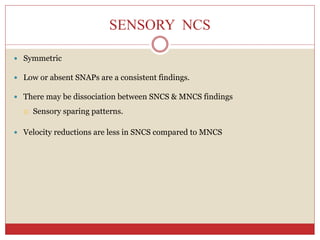
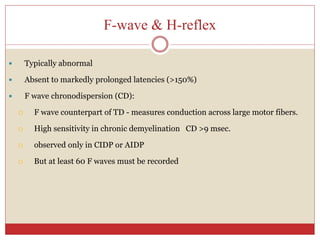
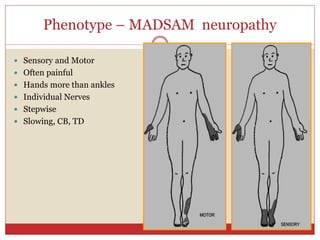
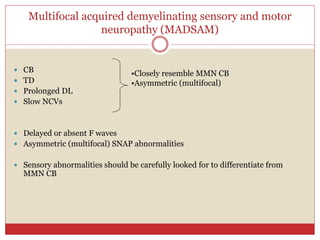
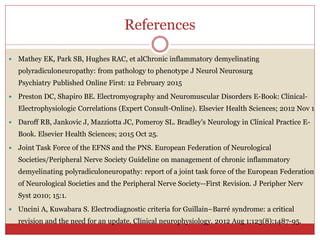
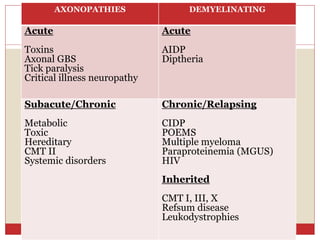
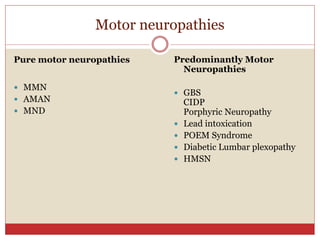
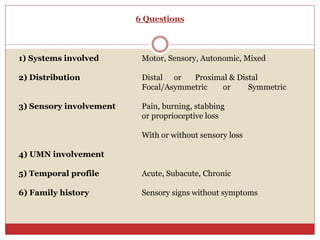
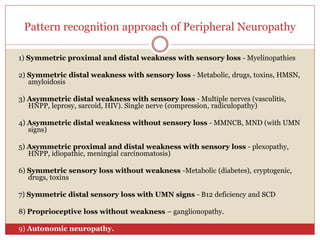
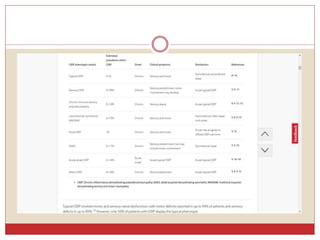
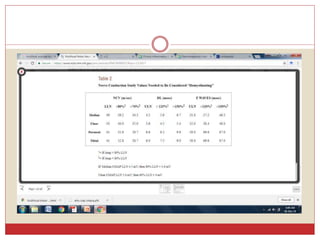
This document discusses electrodiagnostic approaches to peripheral neuropathy. It begins with the anatomy and physiology of peripheral nerves and clinical clues in diagnosis. It then covers electrodiagnostic principles in nerve conduction studies and their use in evaluating various pathologies. Specific examples discussed include mononeuropathy, polyneuropathy, mononeuritis multiplex, and demyelinating vs axonal neuropathies. Case examples are also provided of common conditions like carpal tunnel syndrome, Guillain-Barré syndrome, and chronic inflammatory demyelinating polyneuropathy.