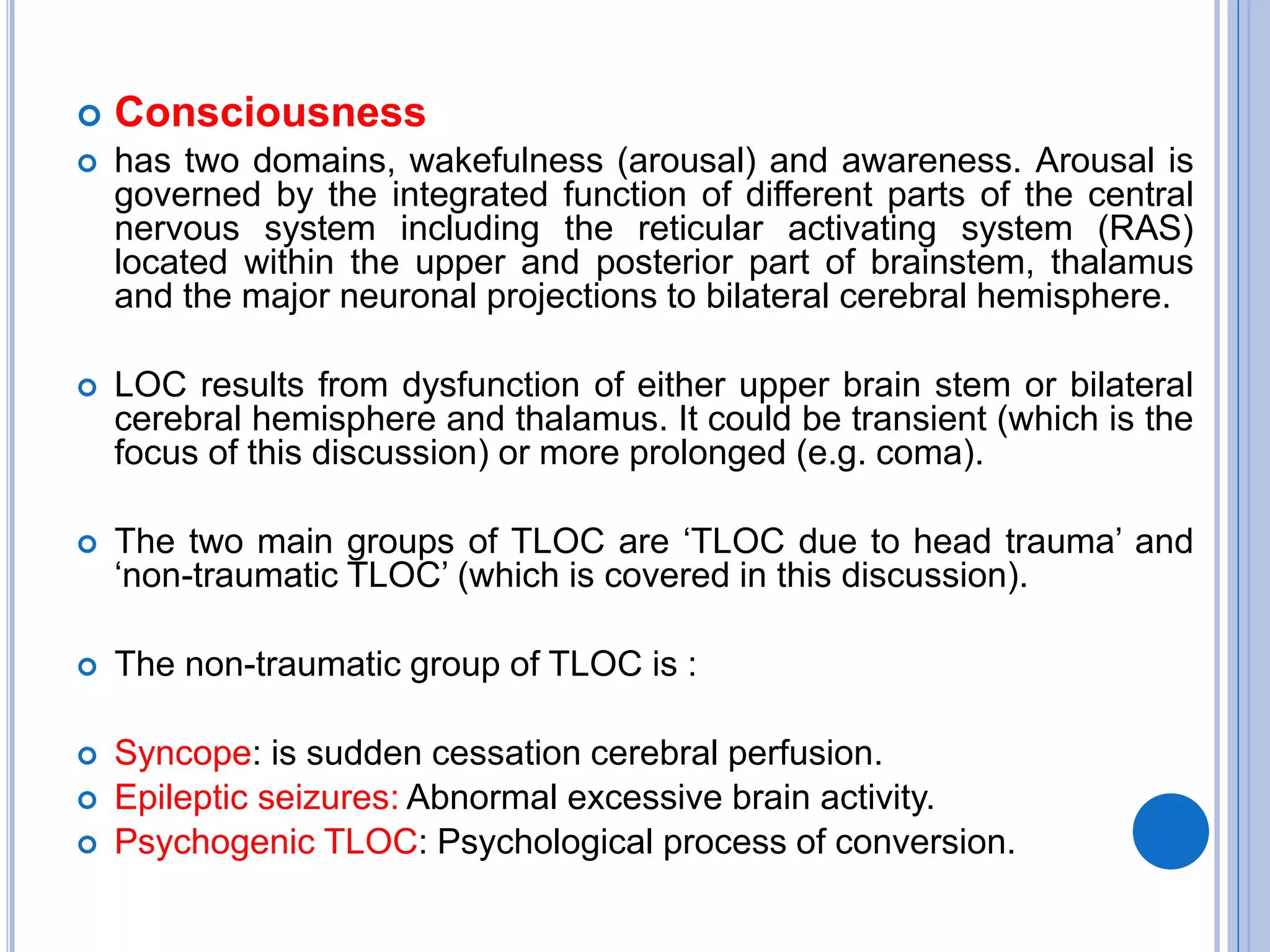
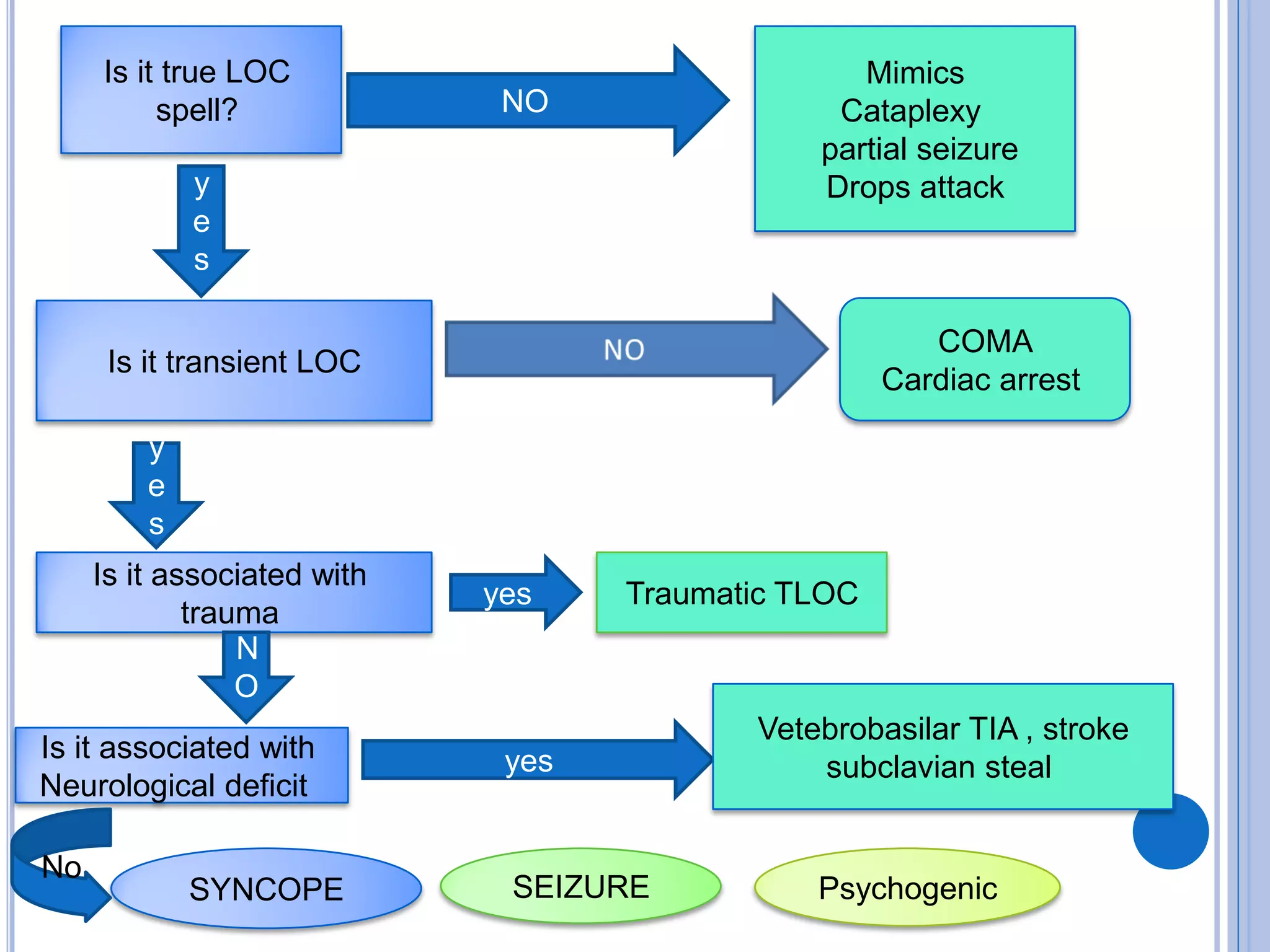
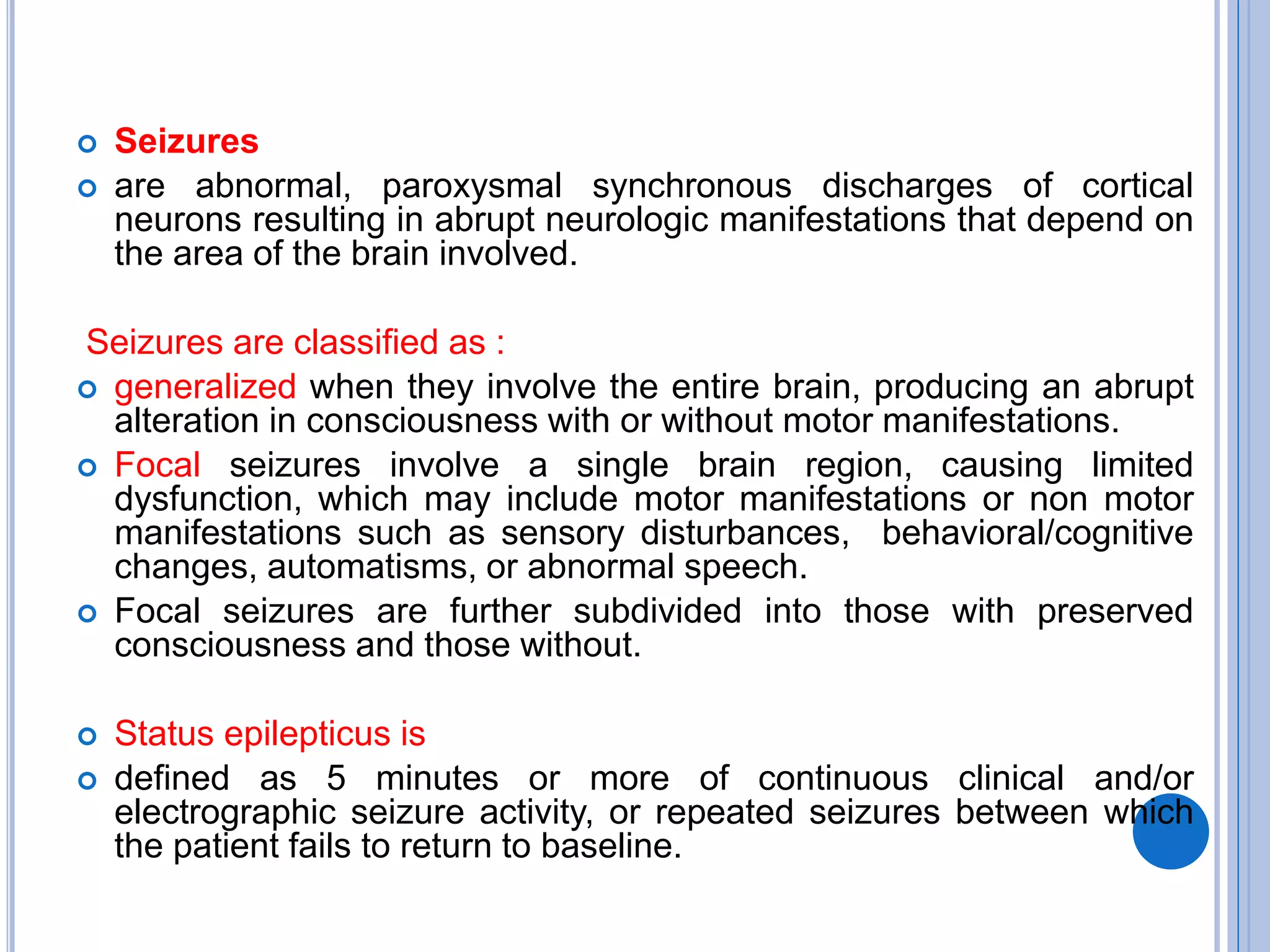
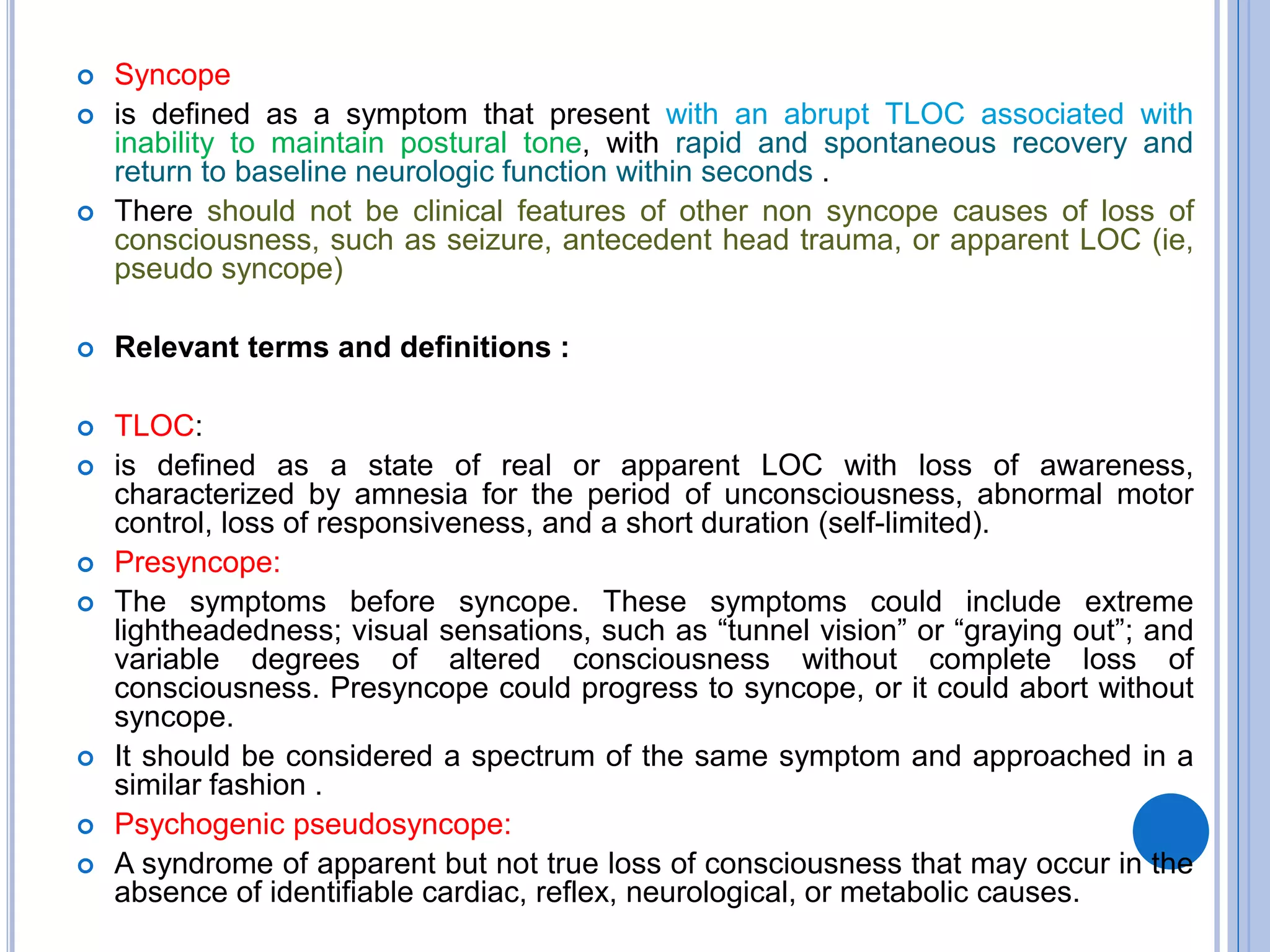
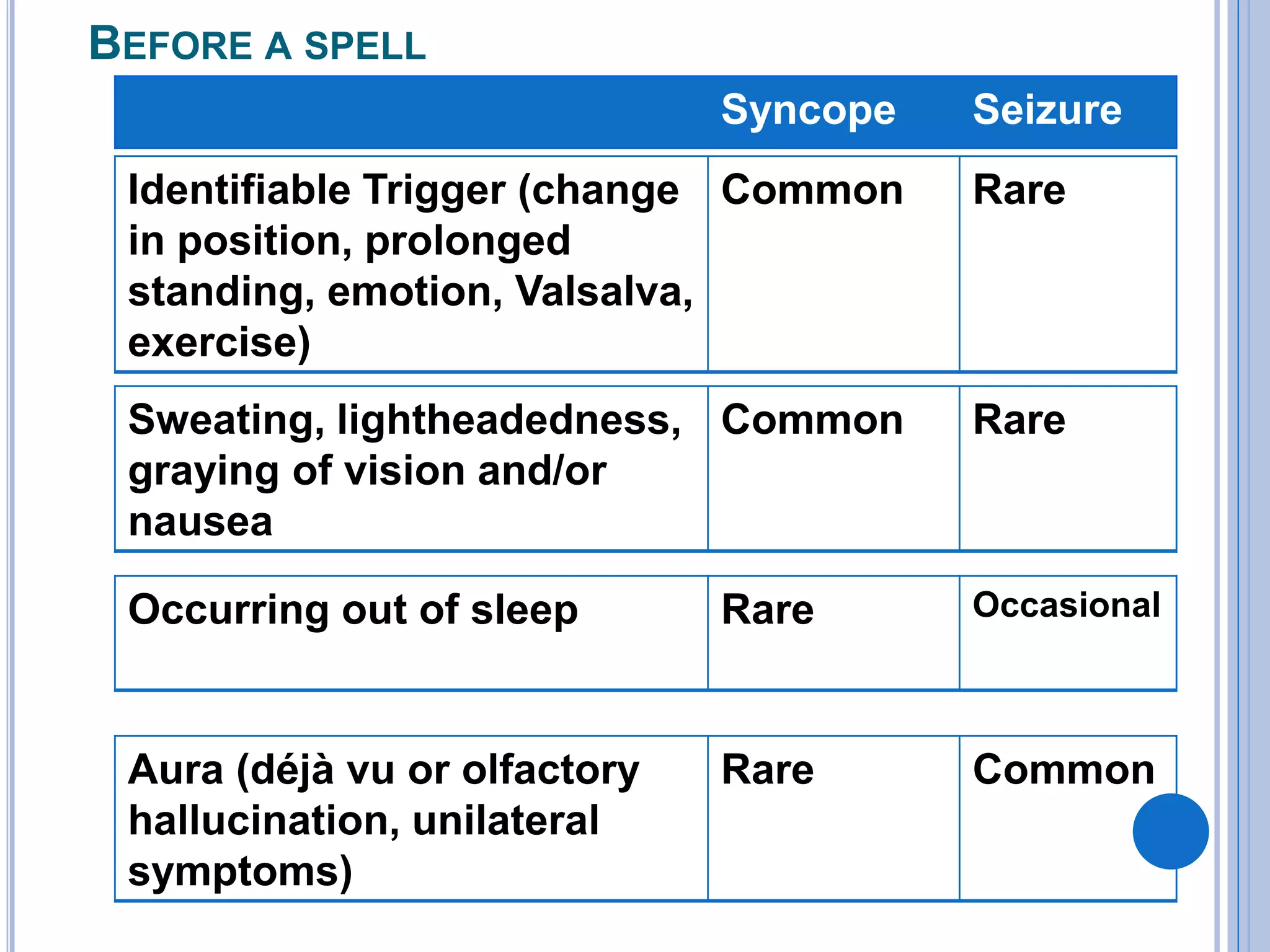
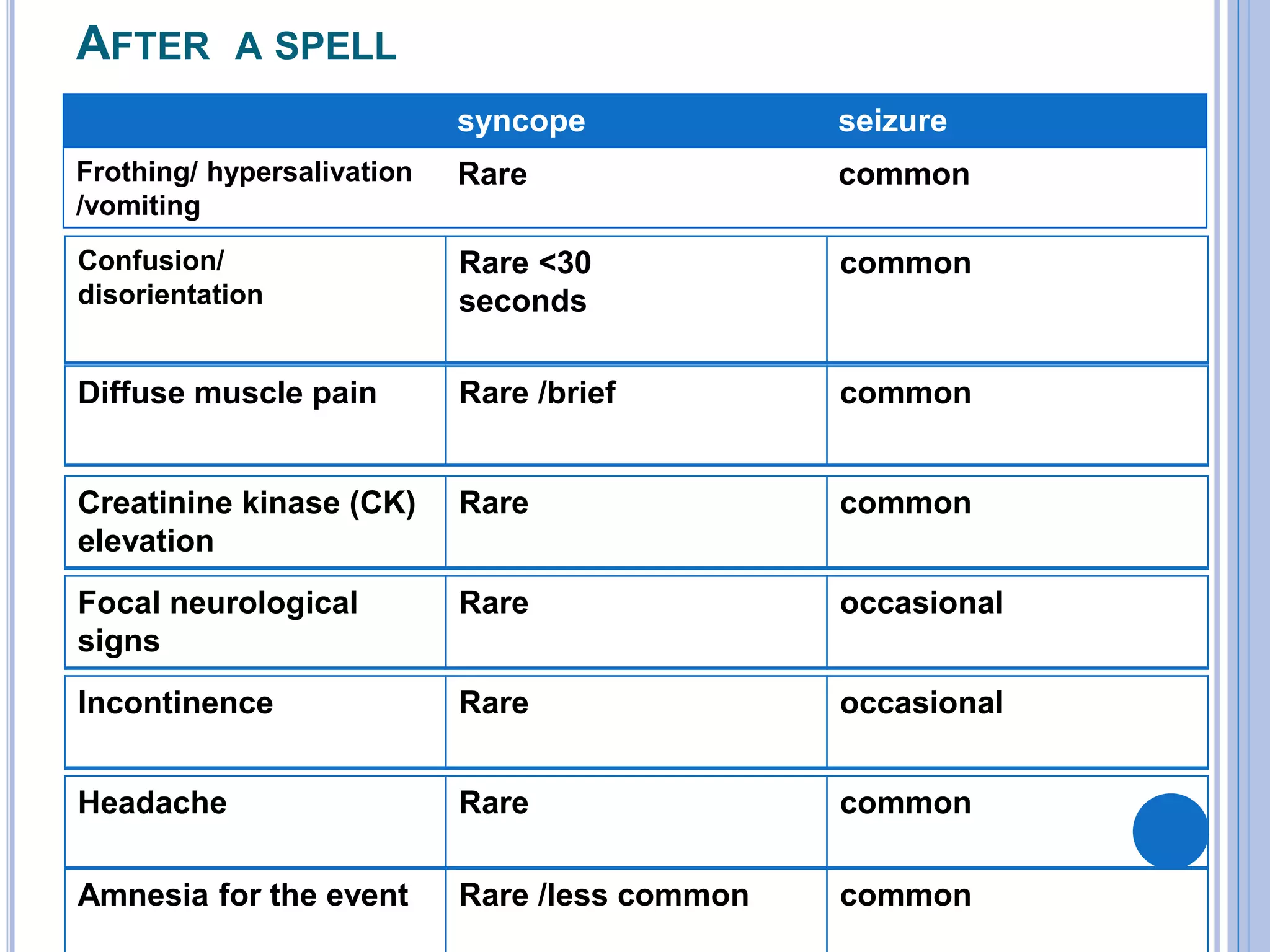
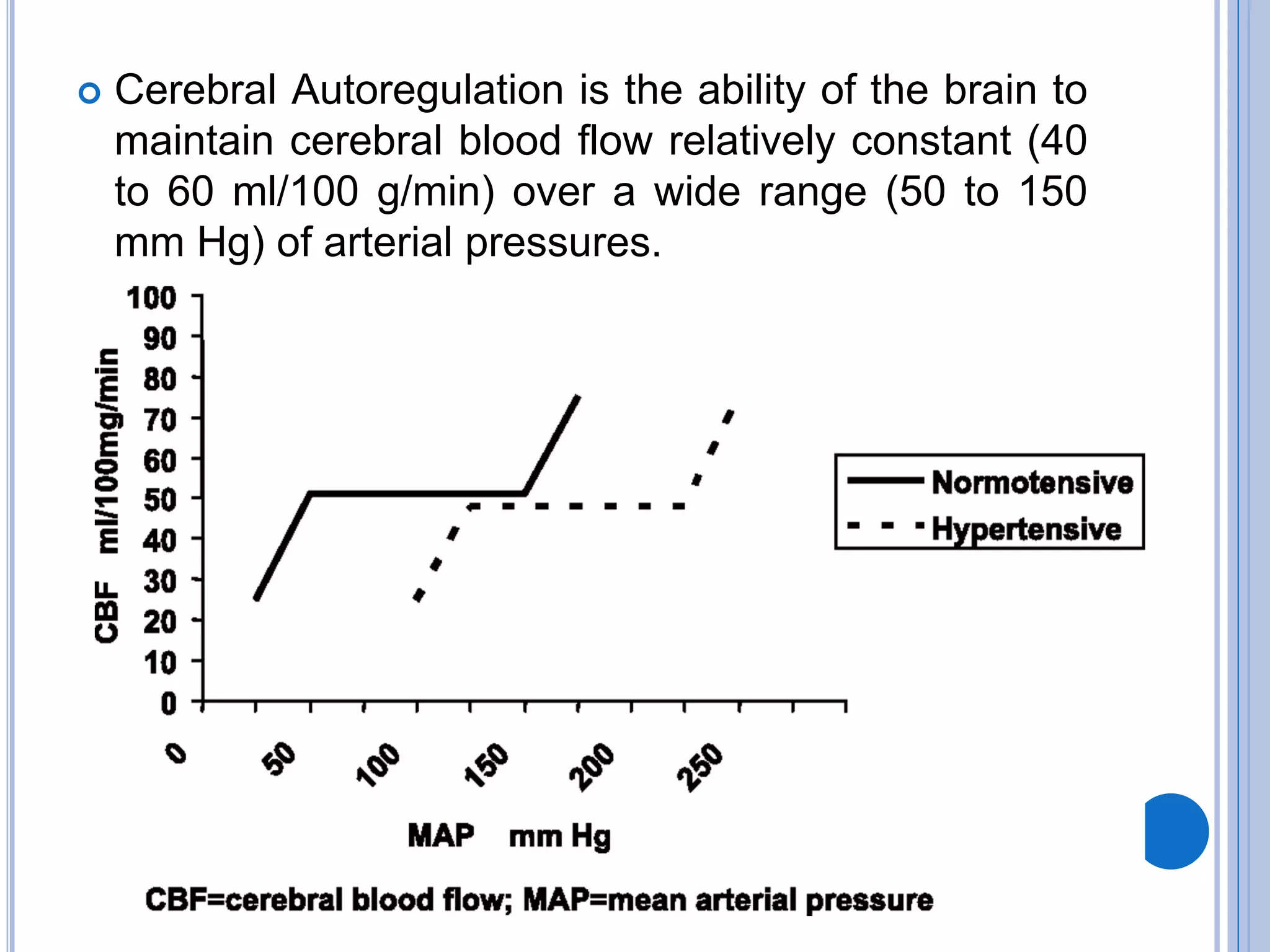
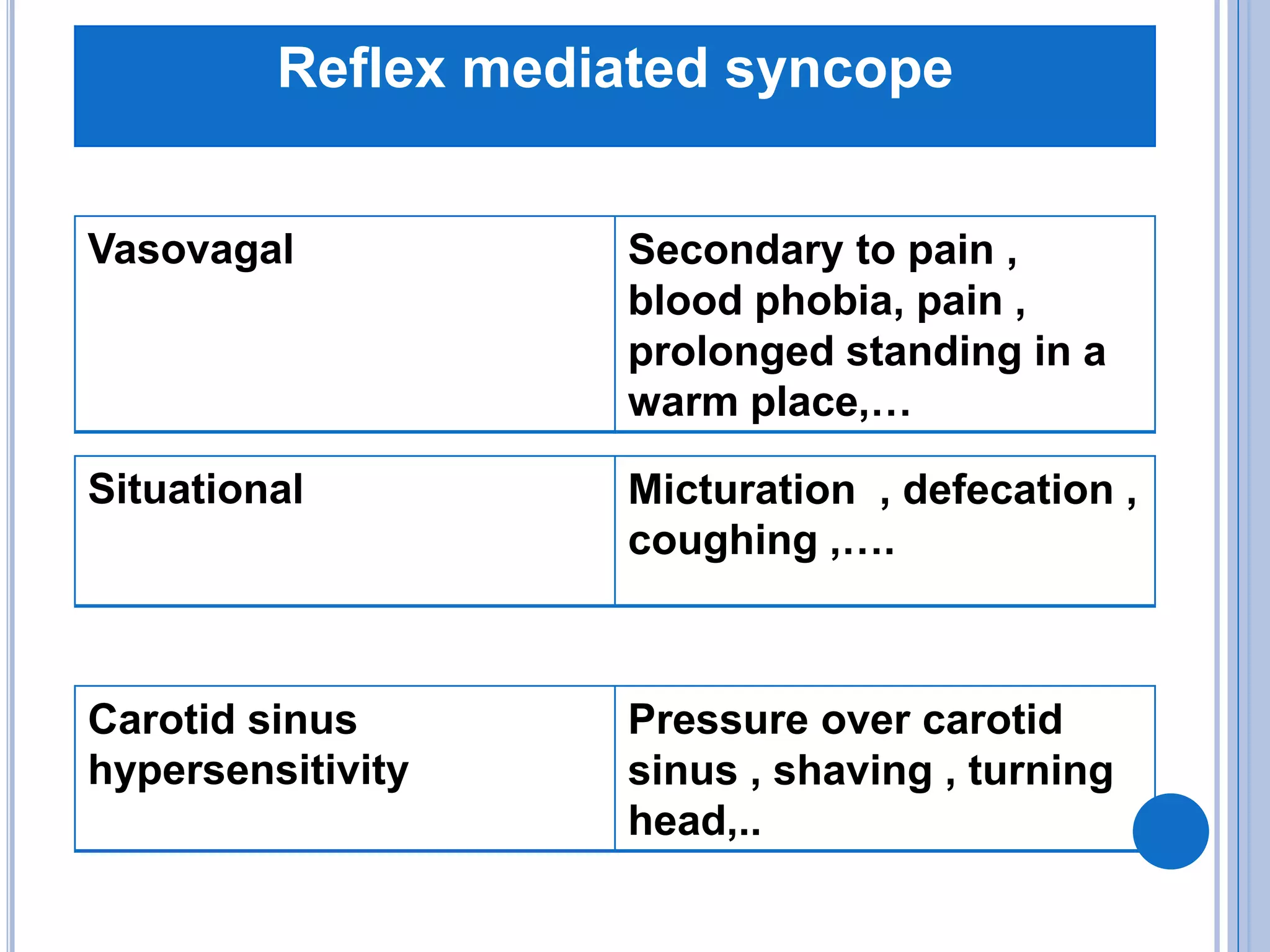
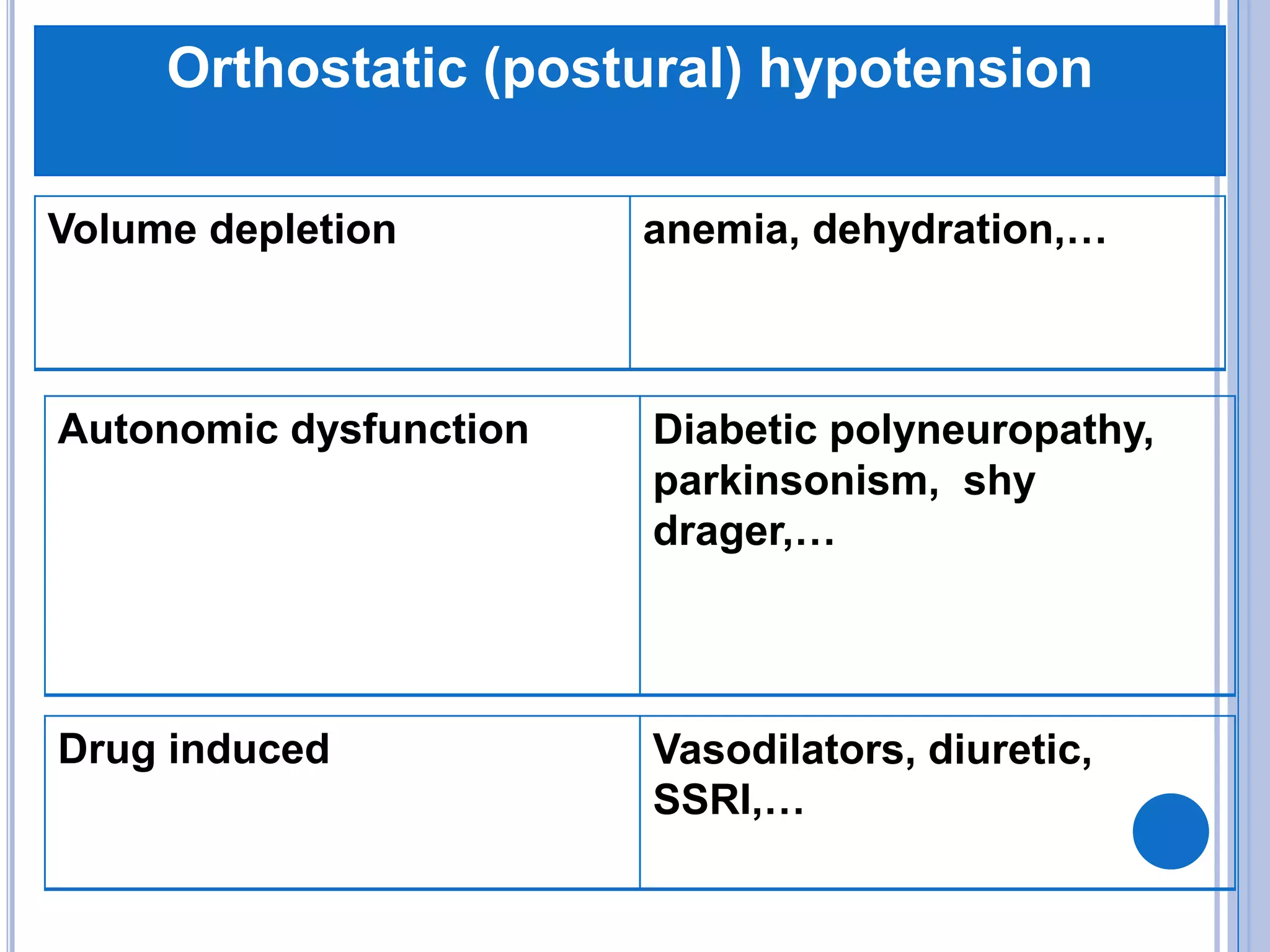
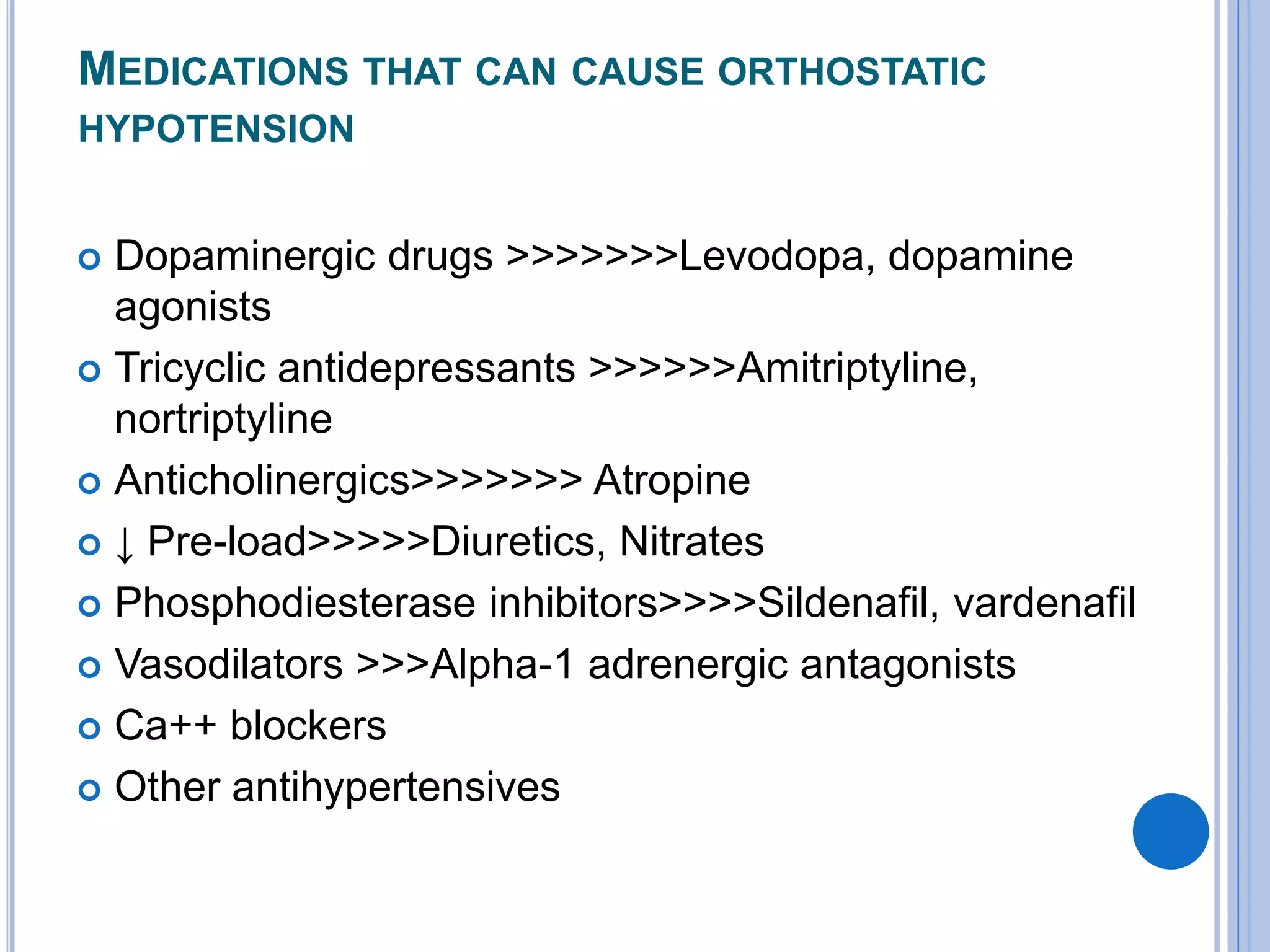
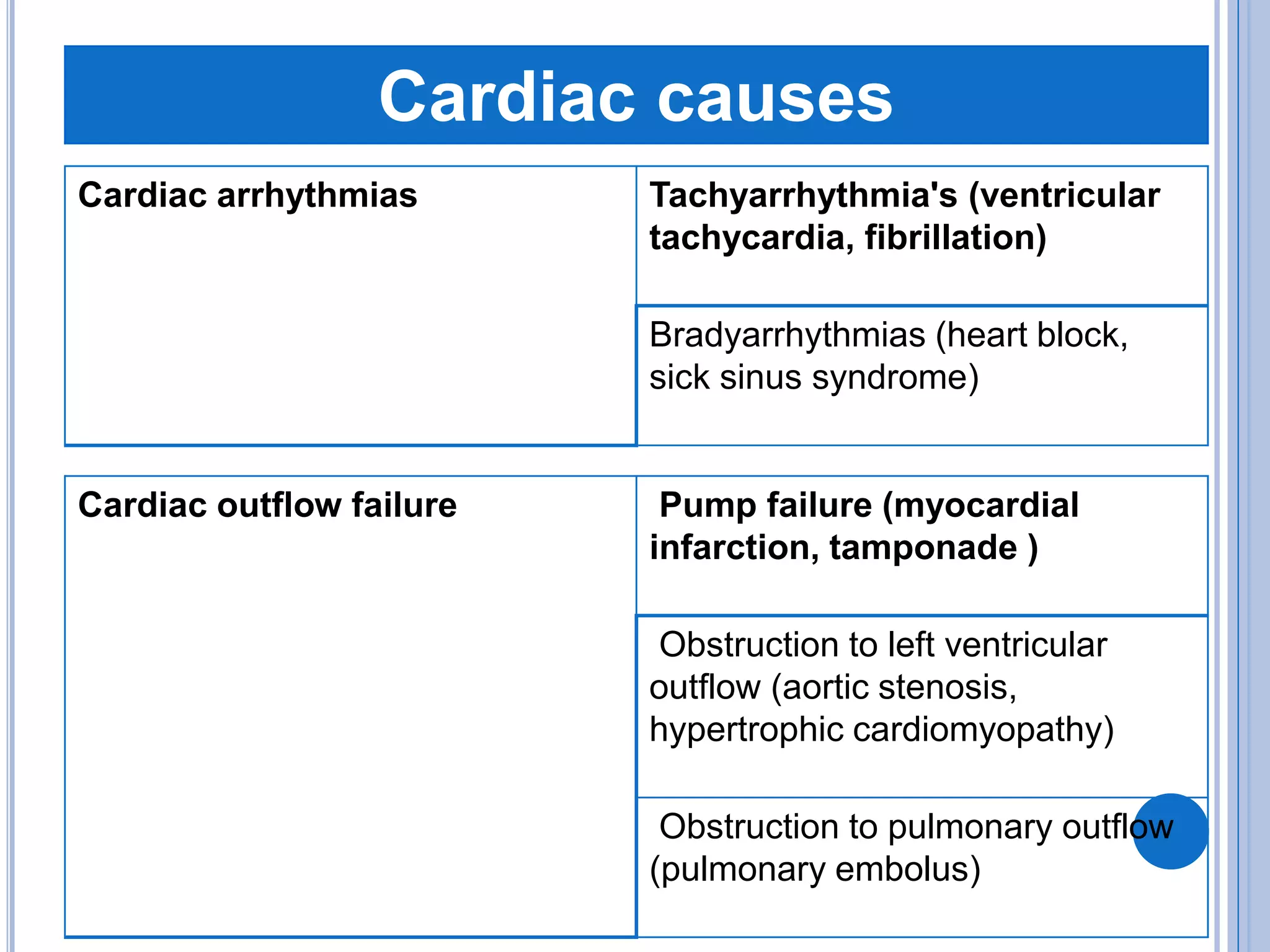
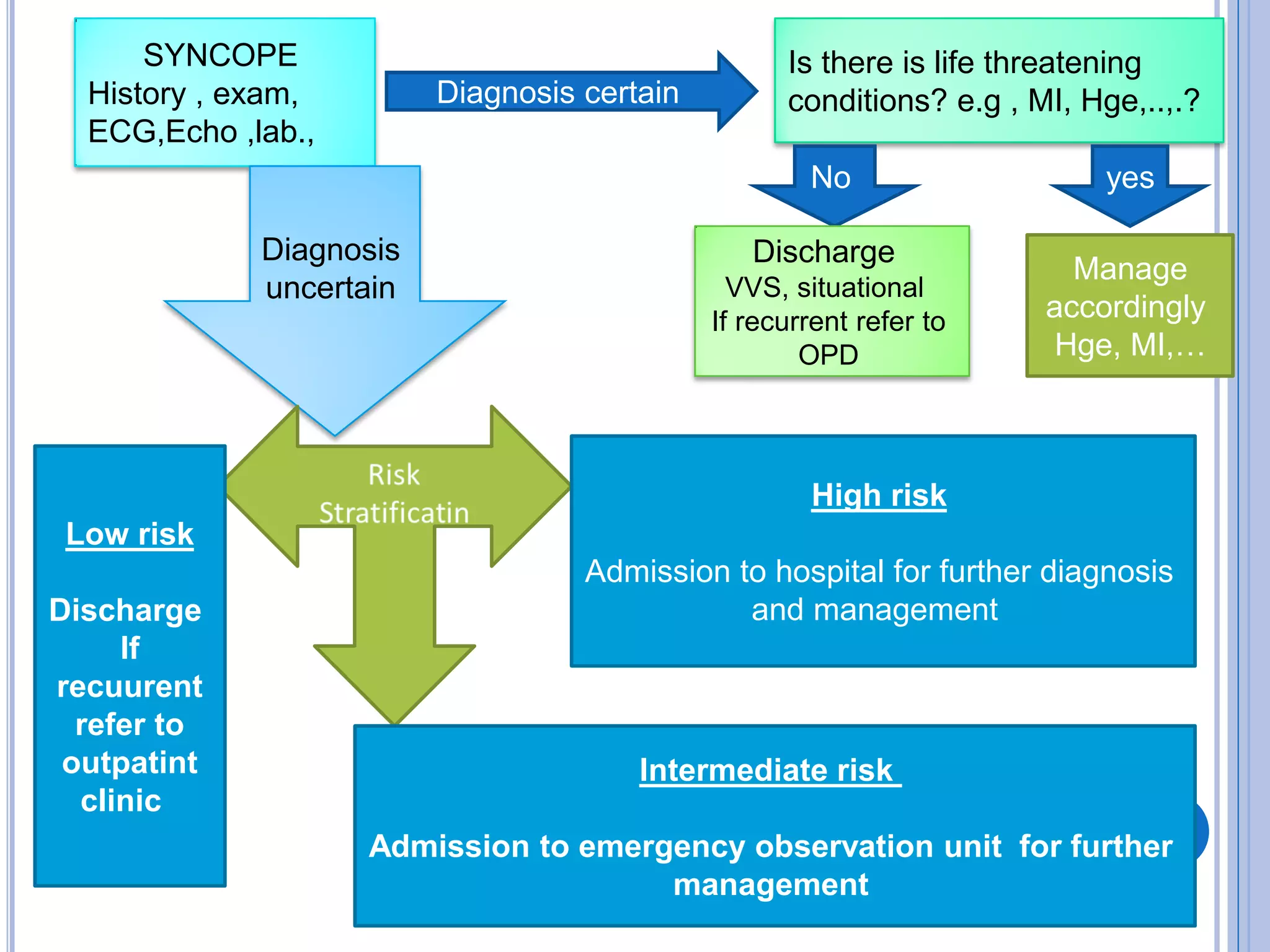
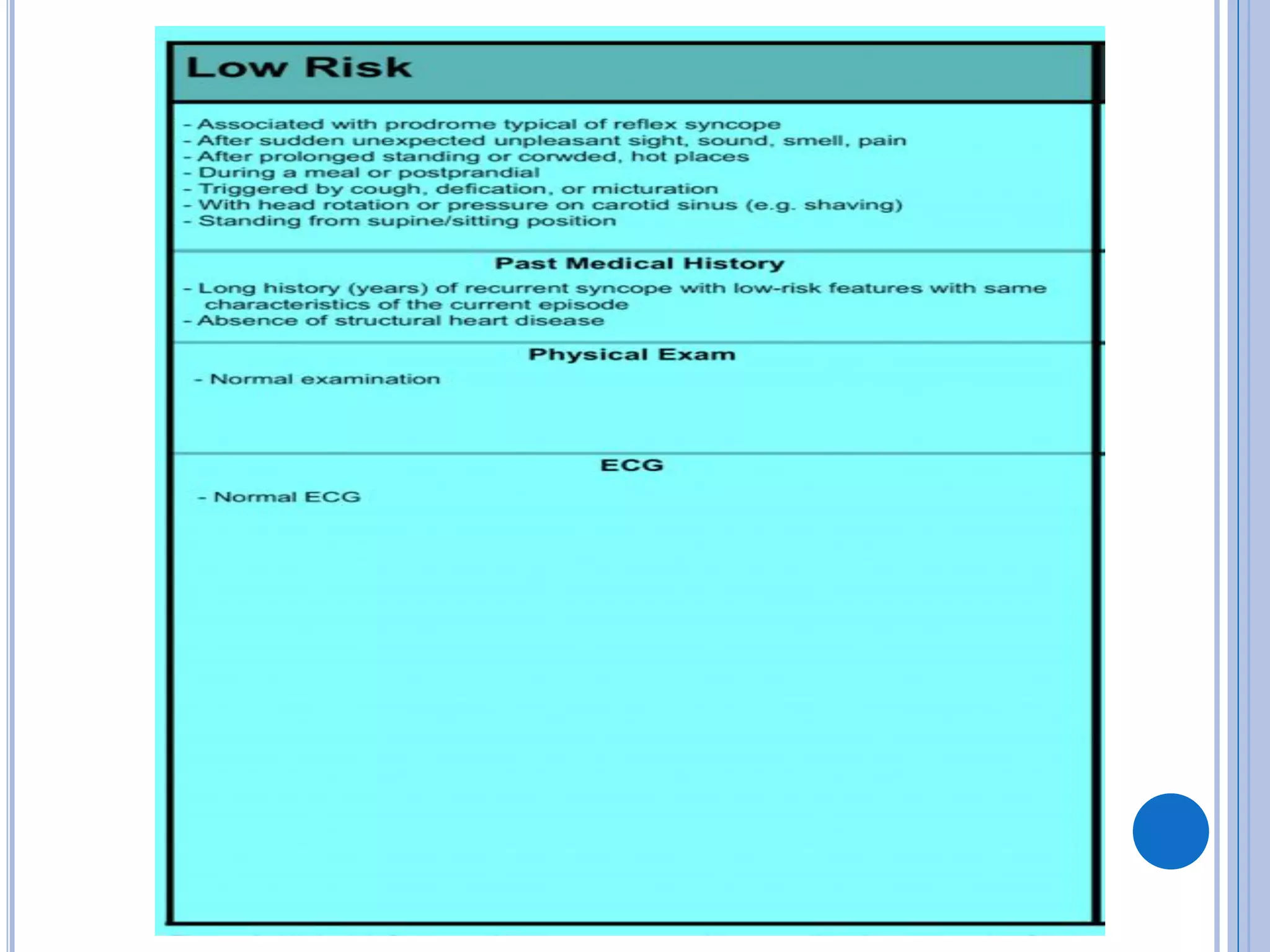
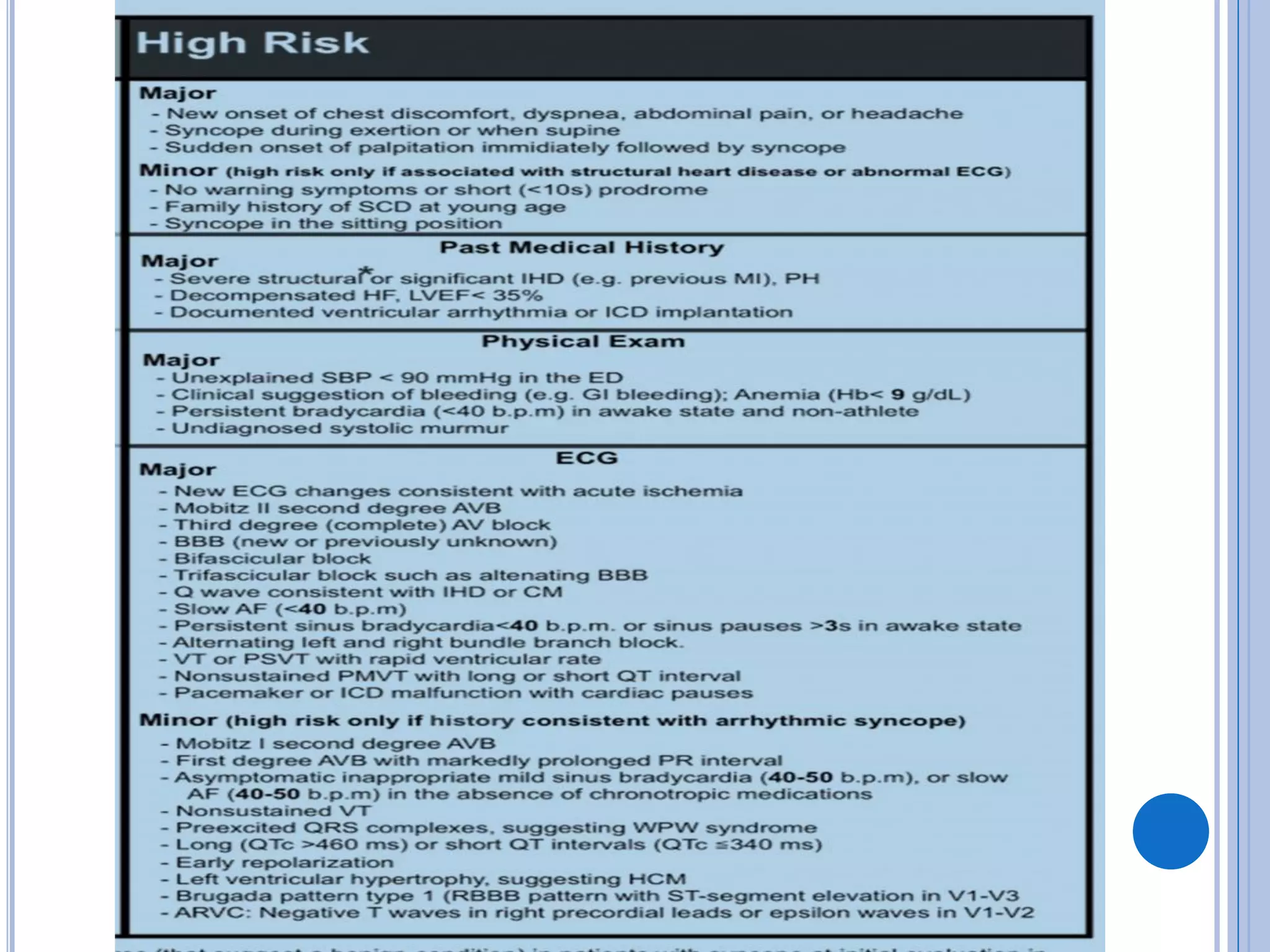
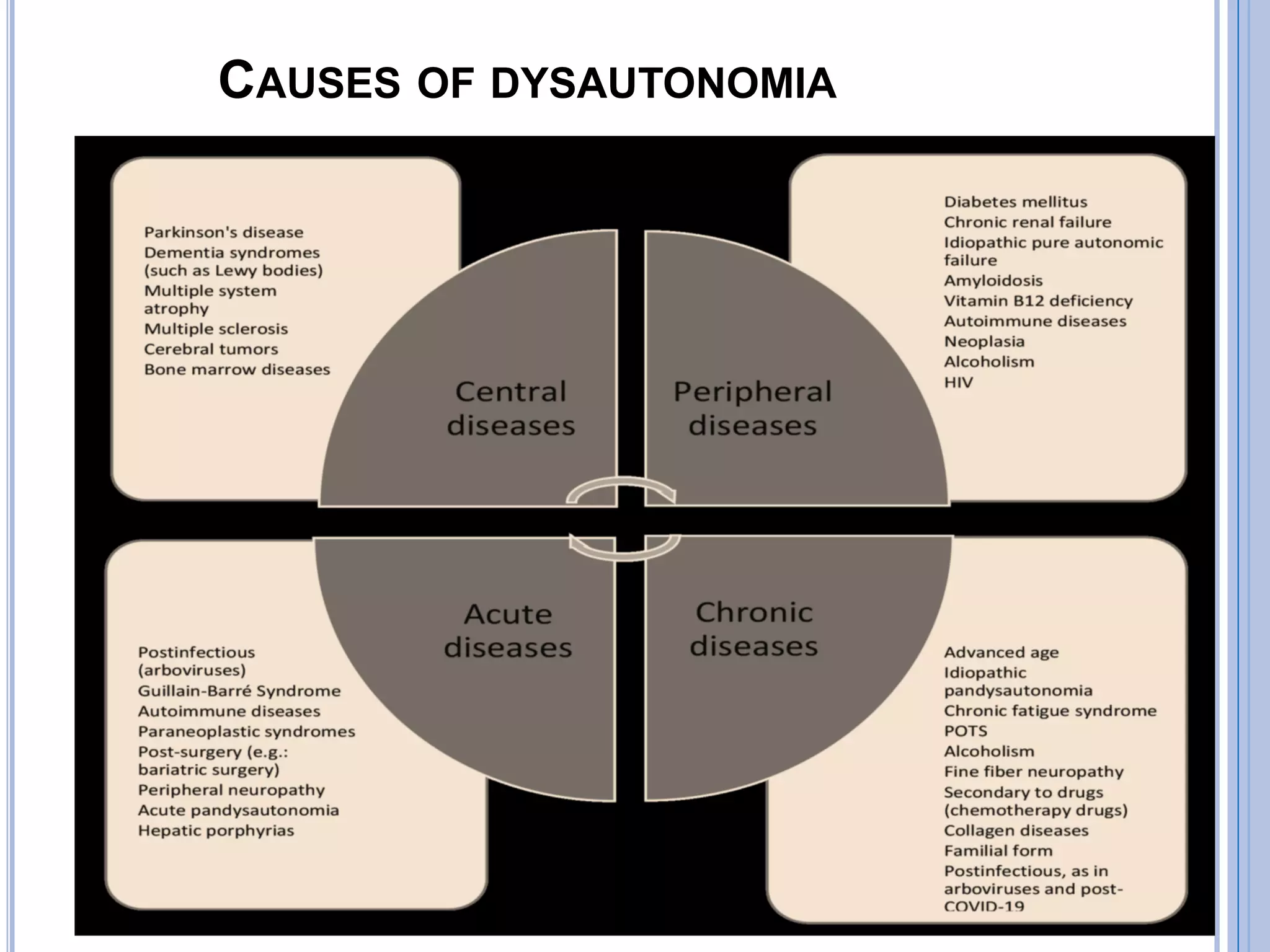
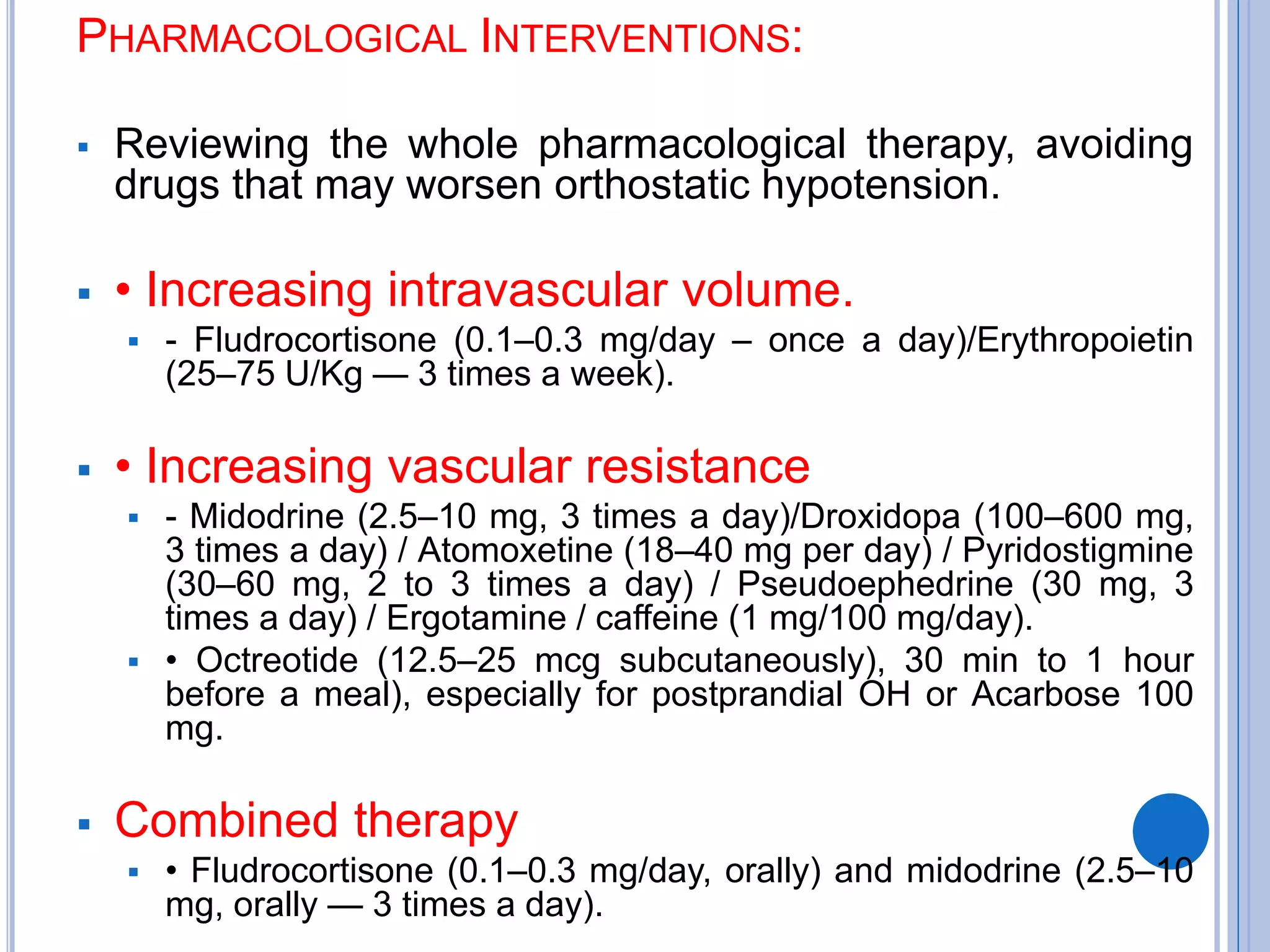
The document discusses transient loss of consciousness (TLOC), highlighting its two main types: traumatic and non-traumatic, the latter encompassing syncope, epileptic seizures, and psychogenic TLOC. It explains the mechanisms behind these conditions, their symptoms, classifications, and management strategies, including pharmacological and non-pharmacological interventions. Additionally, it covers the importance of identifying potential life-threatening causes associated with syncope and describes diagnostic procedures for various forms of dysautonomia.