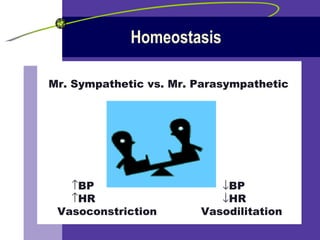
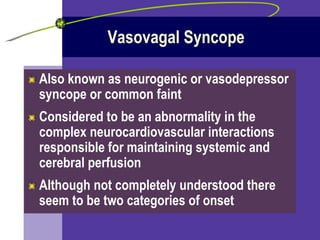
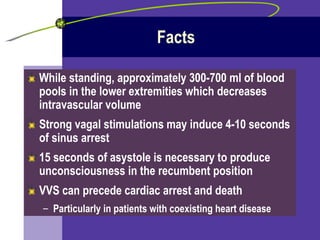
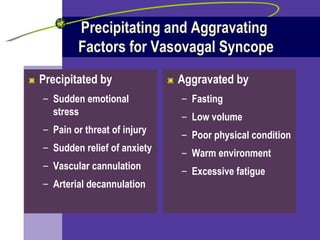
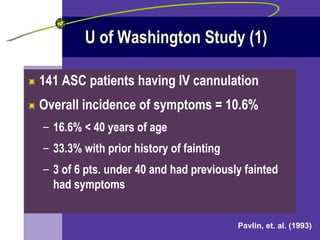
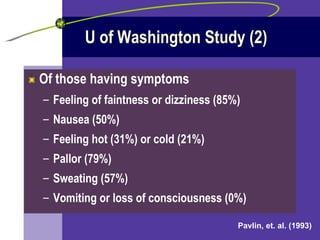
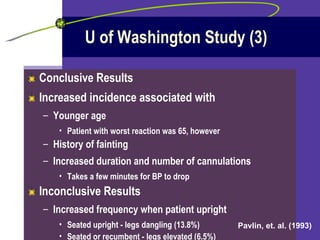
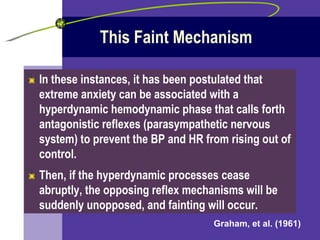
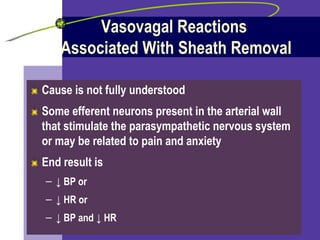
Vasovagal syncope (VVS) is caused by an abnormal response of the autonomic nervous system that leads to a drop in blood pressure and sometimes heart rate. It is triggered by pain, anxiety, or emotional stress and causes feelings of faintness. Those at highest risk include younger patients and those with a history of fainting. Nursing care focuses on recognizing VVS symptoms and treating lowered blood pressure and heart rate by having patients lie down with legs elevated.