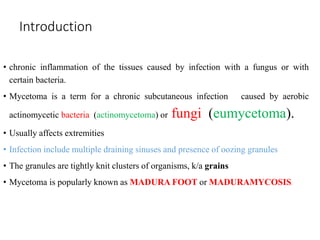
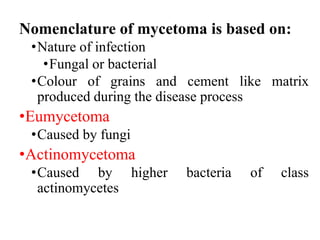
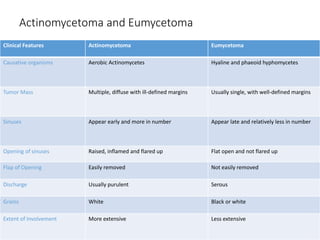
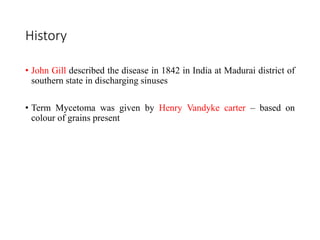
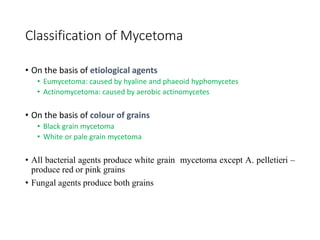
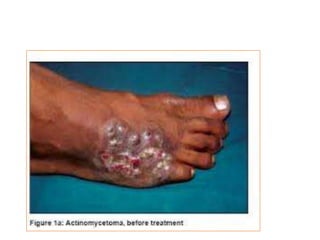
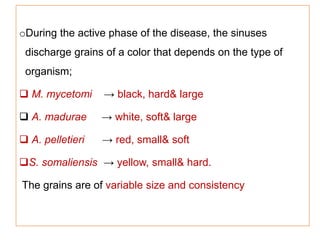
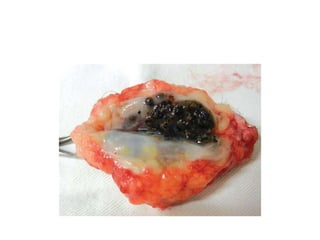
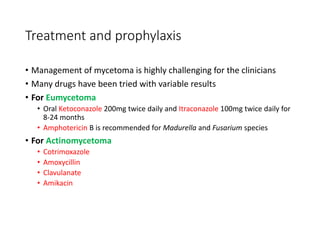
- Mycetoma is a chronic subcutaneous infection caused by fungi or bacteria that is characterized by tumor-like swellings, draining sinuses, and the discharge of colored grains from the sinuses.
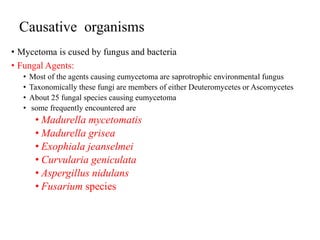
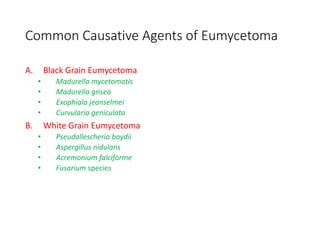
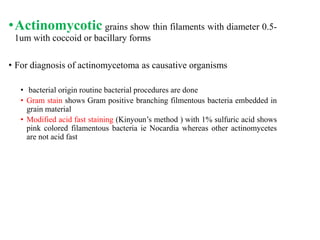
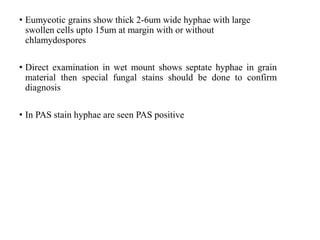
- It is most commonly caused by Nocardia and Streptomyces bacteria (actinomycetoma) or fungi of the genera Madurella and Exophiala (eumycetoma).
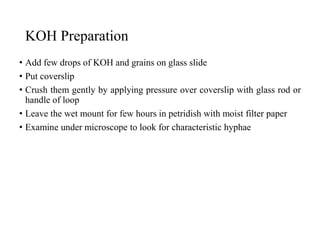
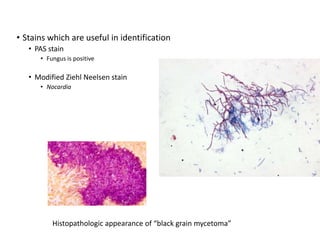
- The infection occurs after traumatic introduction of the causative agents into the skin, most often in the extremities. It progresses slowly over years and can cause extensive tissue destruction if left untreated. Diagnosis involves examination of grains discharged from sinuses for fungal or bacterial elements. Treatment involves long-term