- Status epilepticus is defined as continuous seizure activity lasting more than 30 minutes or recurrent seizures without regaining consciousness. It is a medical emergency requiring prompt treatment.
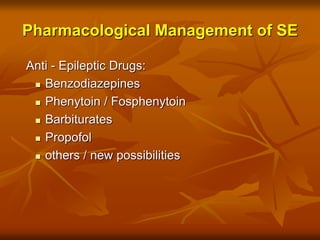
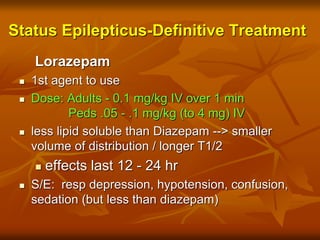
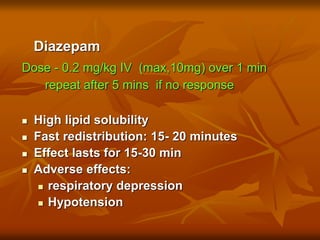
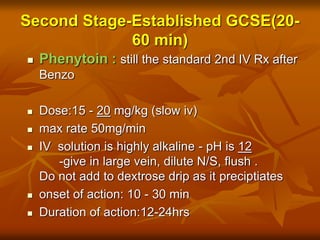
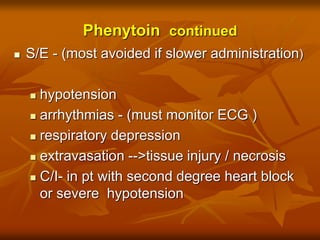
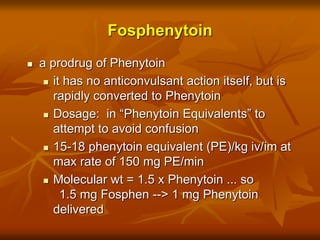
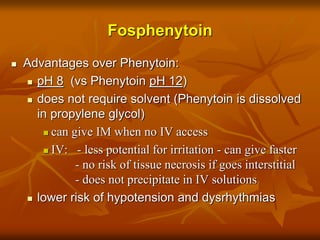
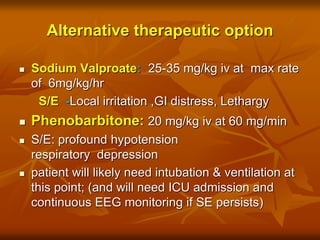
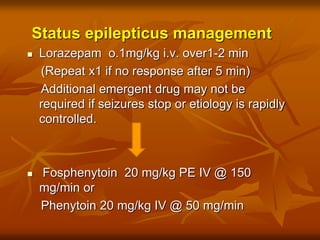
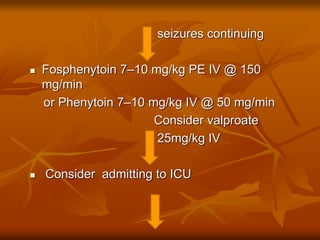
- Initial treatment involves stabilizing airway, breathing, and circulation. Intravenous lorazepam, diazepam, fosphenytoin, or phenytoin are then used to stop seizures.
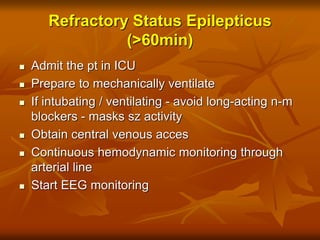
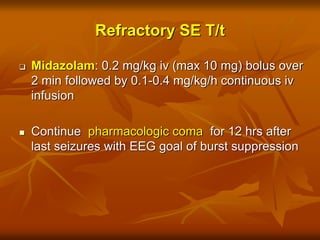
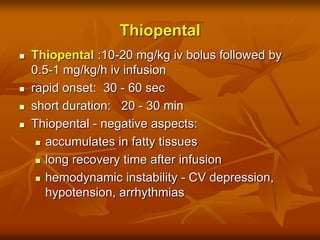
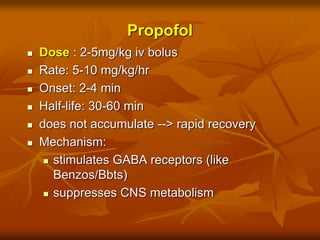
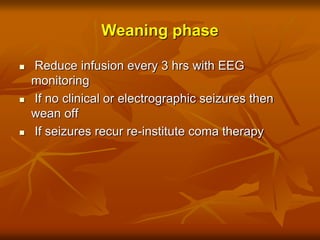
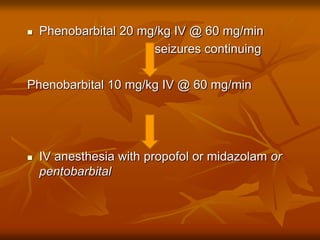
- For refractory status epilepticus lasting over 60 minutes, further treatment with midazolam, thiopental, propofol, or pentobarbital infusion is needed to induce a medically-induced coma. Maintenance anti-epileptic drugs are then used to prevent seizure recurrence.