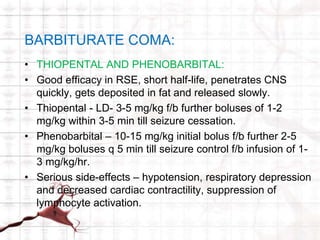
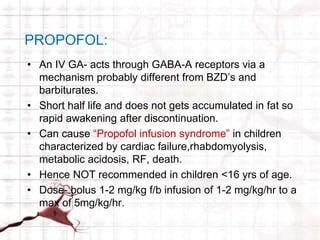
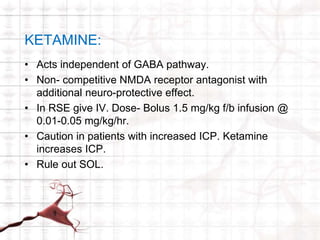
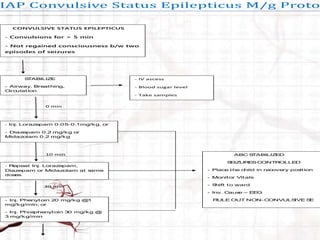
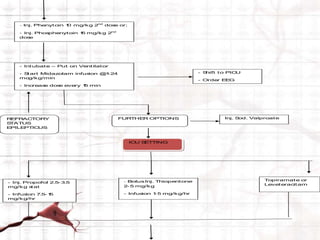
Status epilepticus (SE) is defined as continuous seizure activity lasting more than 5 minutes or 2 or more seizures within 5 minutes without regaining consciousness. SE is a medical emergency that requires rapid stabilization, seizure termination through pharmacotherapy, and treatment of the underlying cause. First-line drugs for seizure termination include benzodiazepines, phenytoin, and valproate. For refractory SE that does not respond to initial treatment, additional options include midazolam infusion, barbiturates, propofol, ketamine, or inhaled anesthetics. Prolonged SE can cause complications and is associated with higher mortality and long-term neurological deficits.