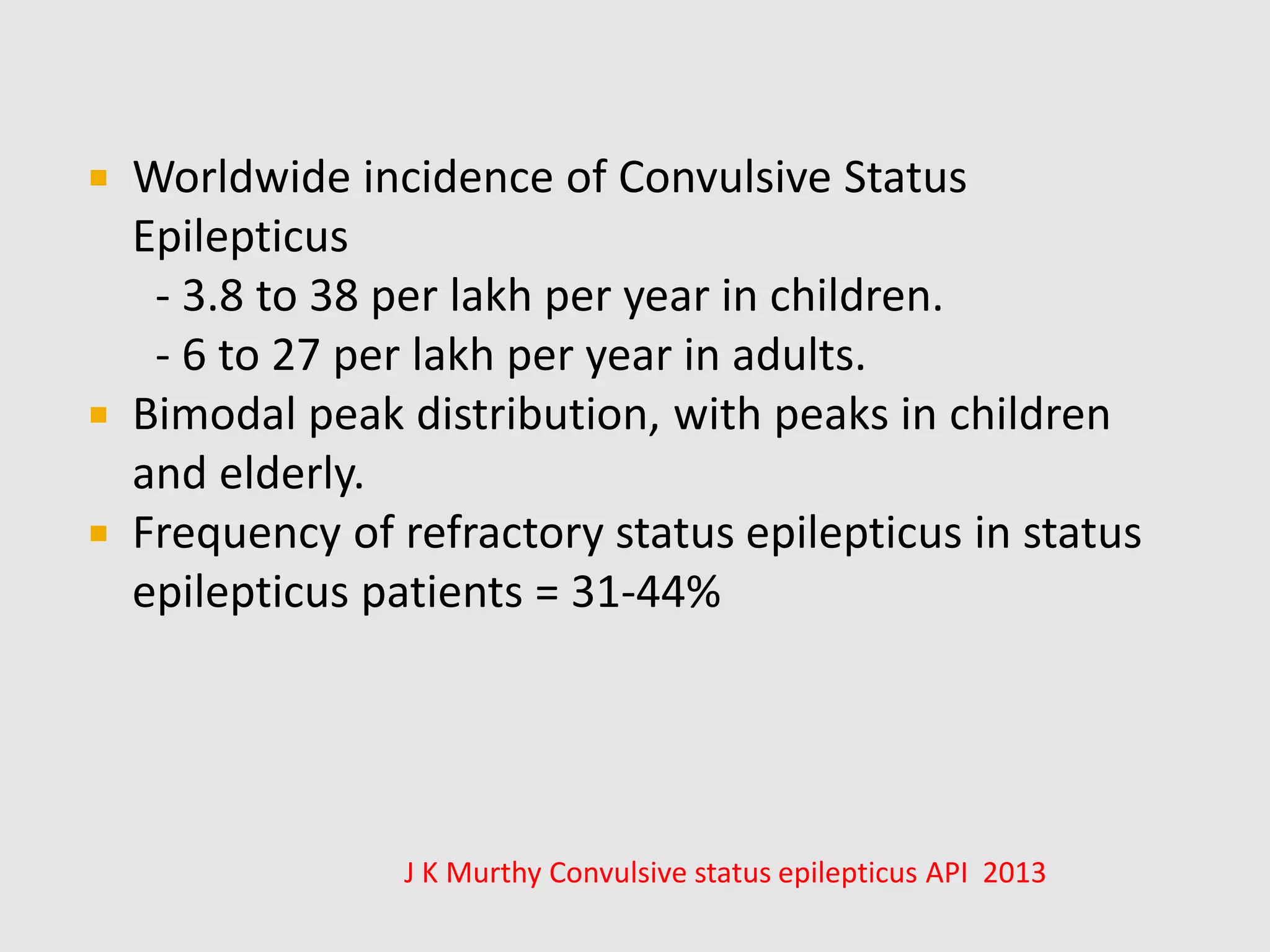
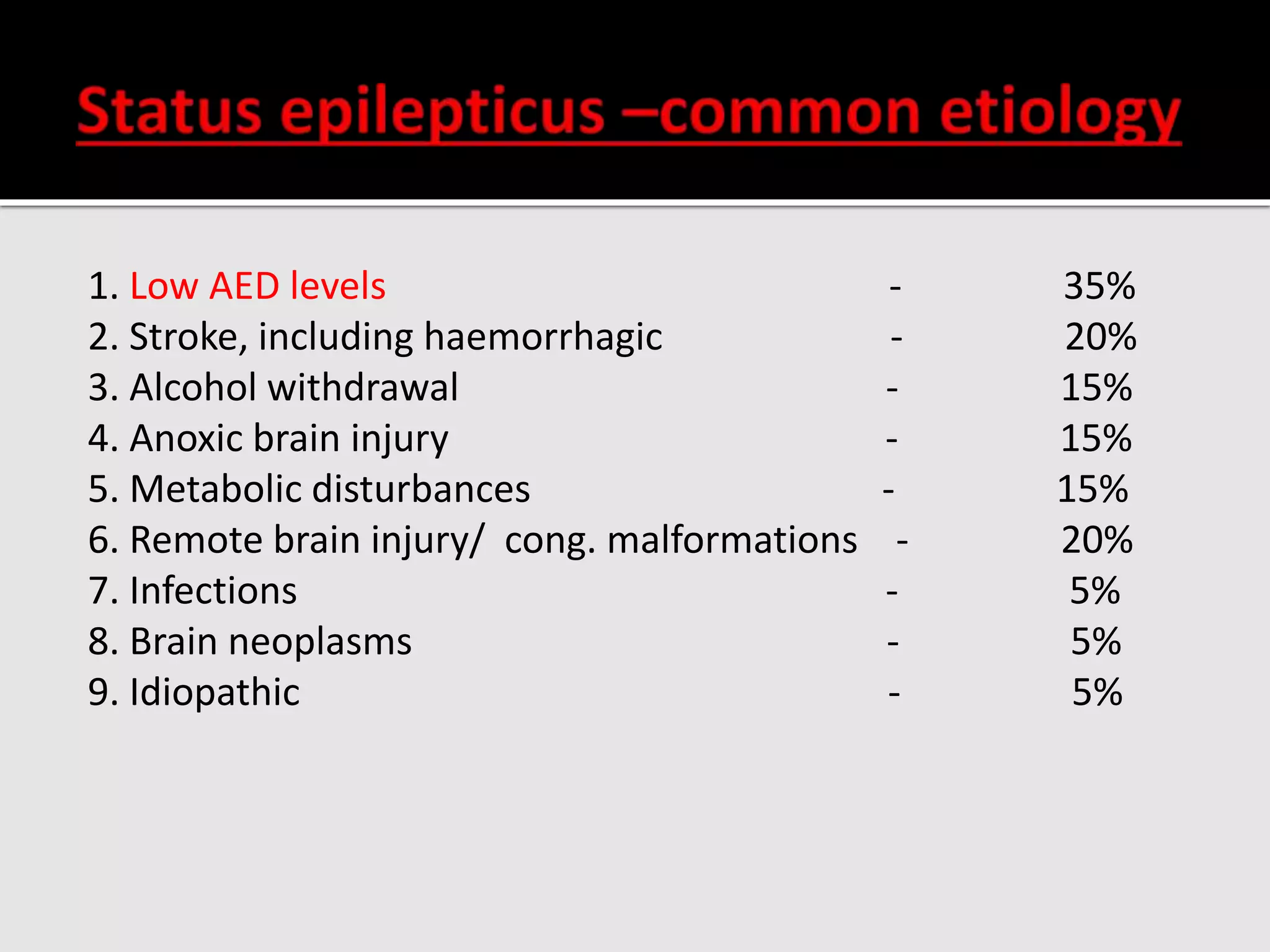
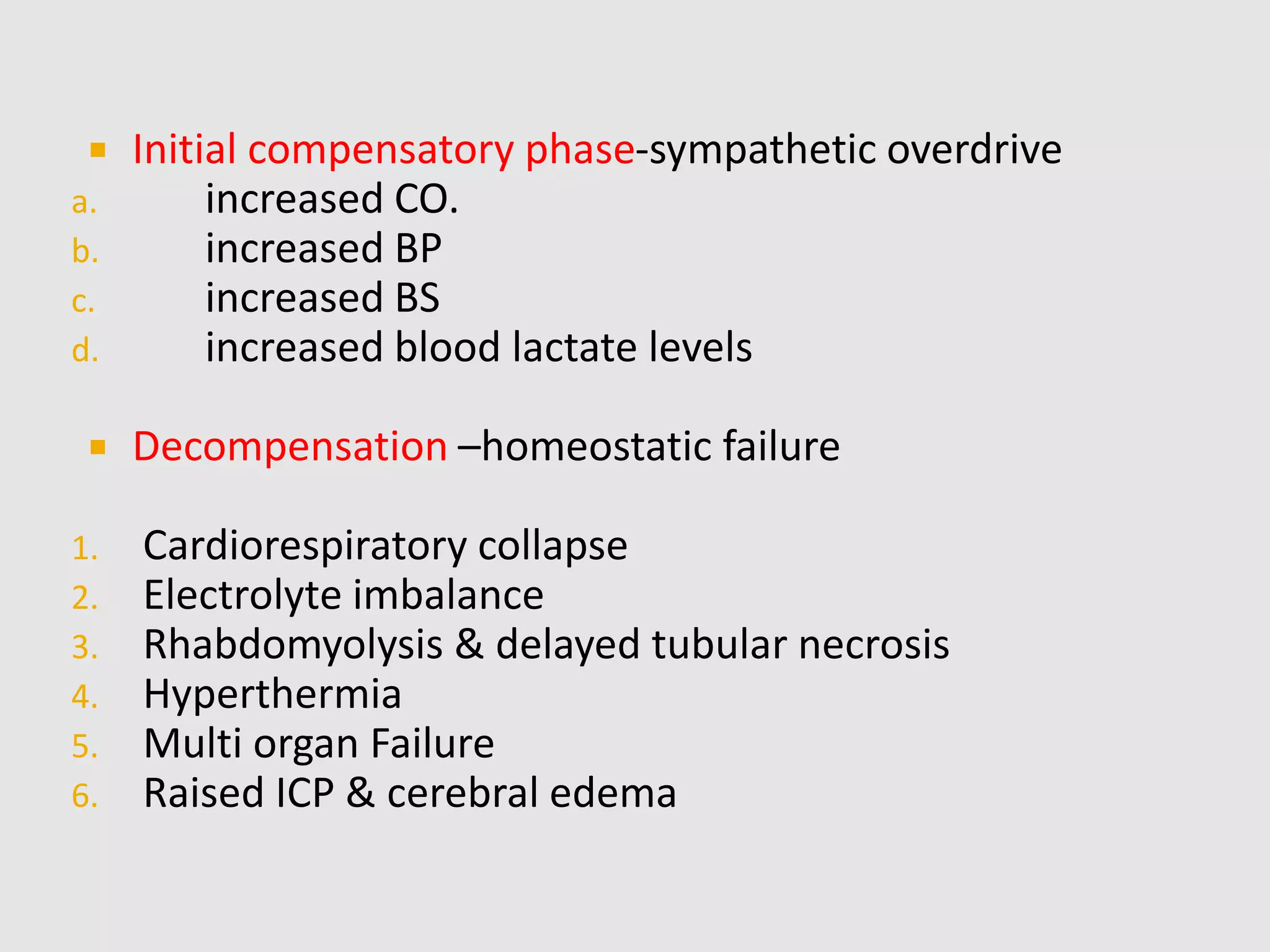
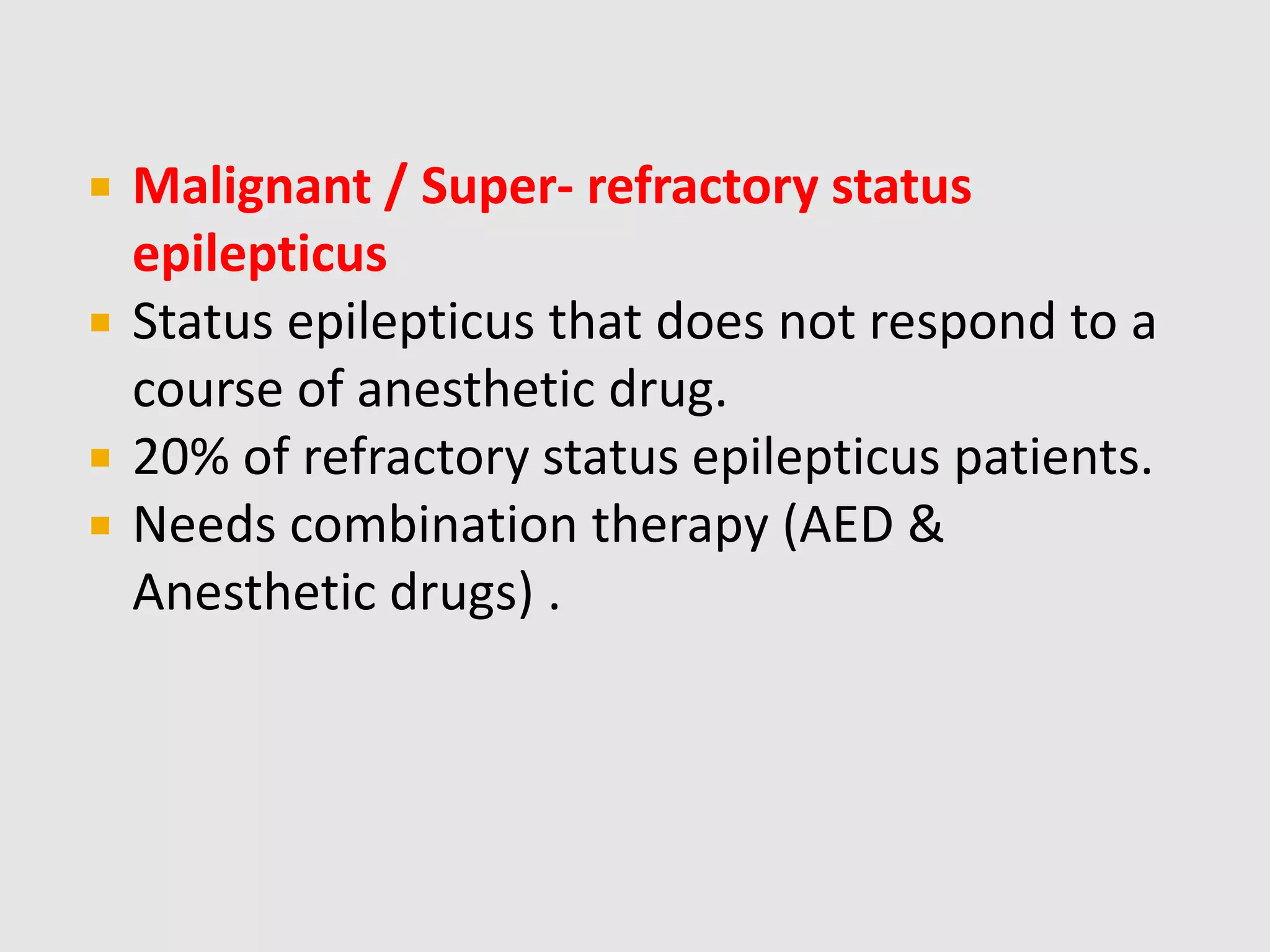
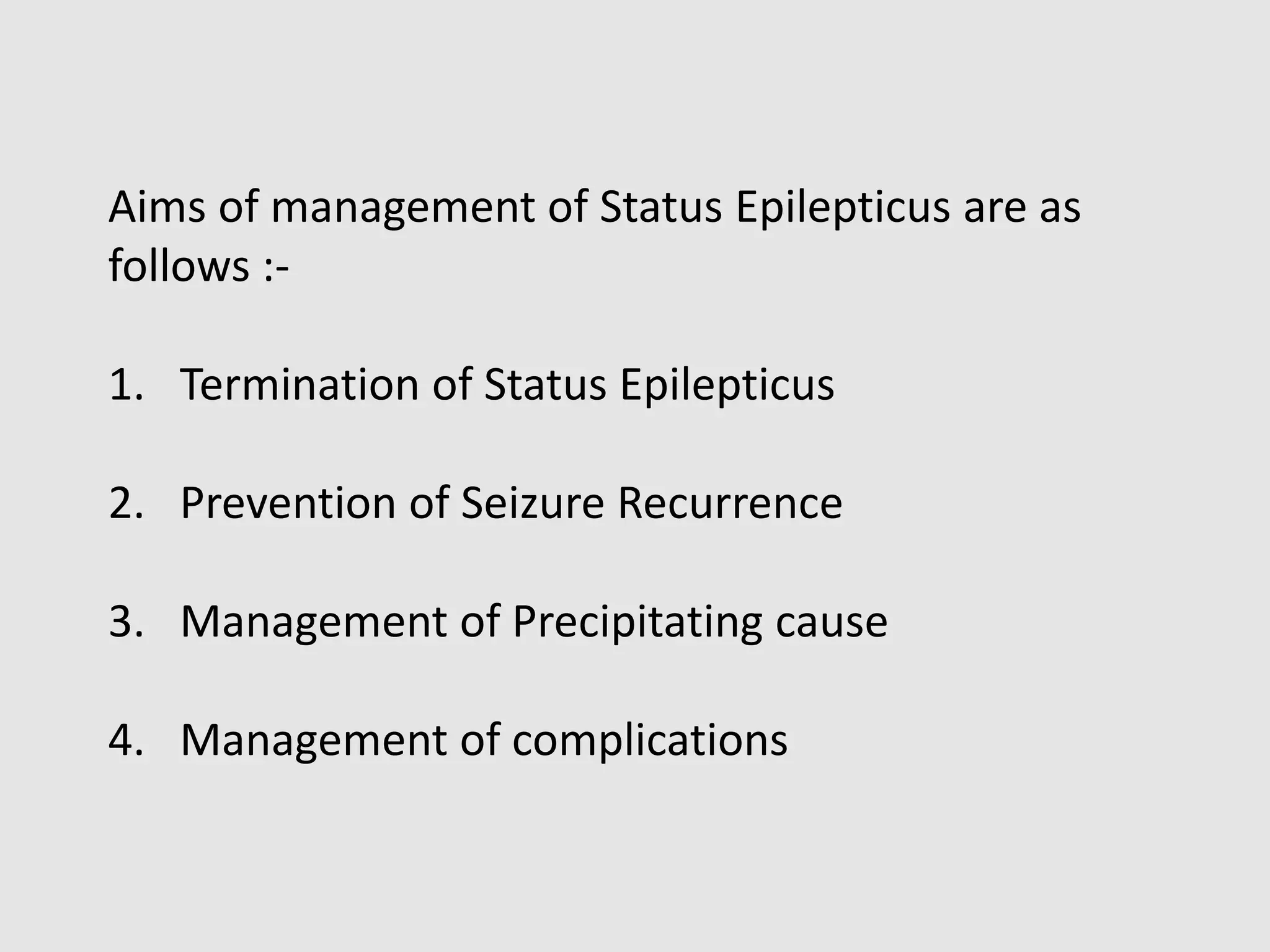
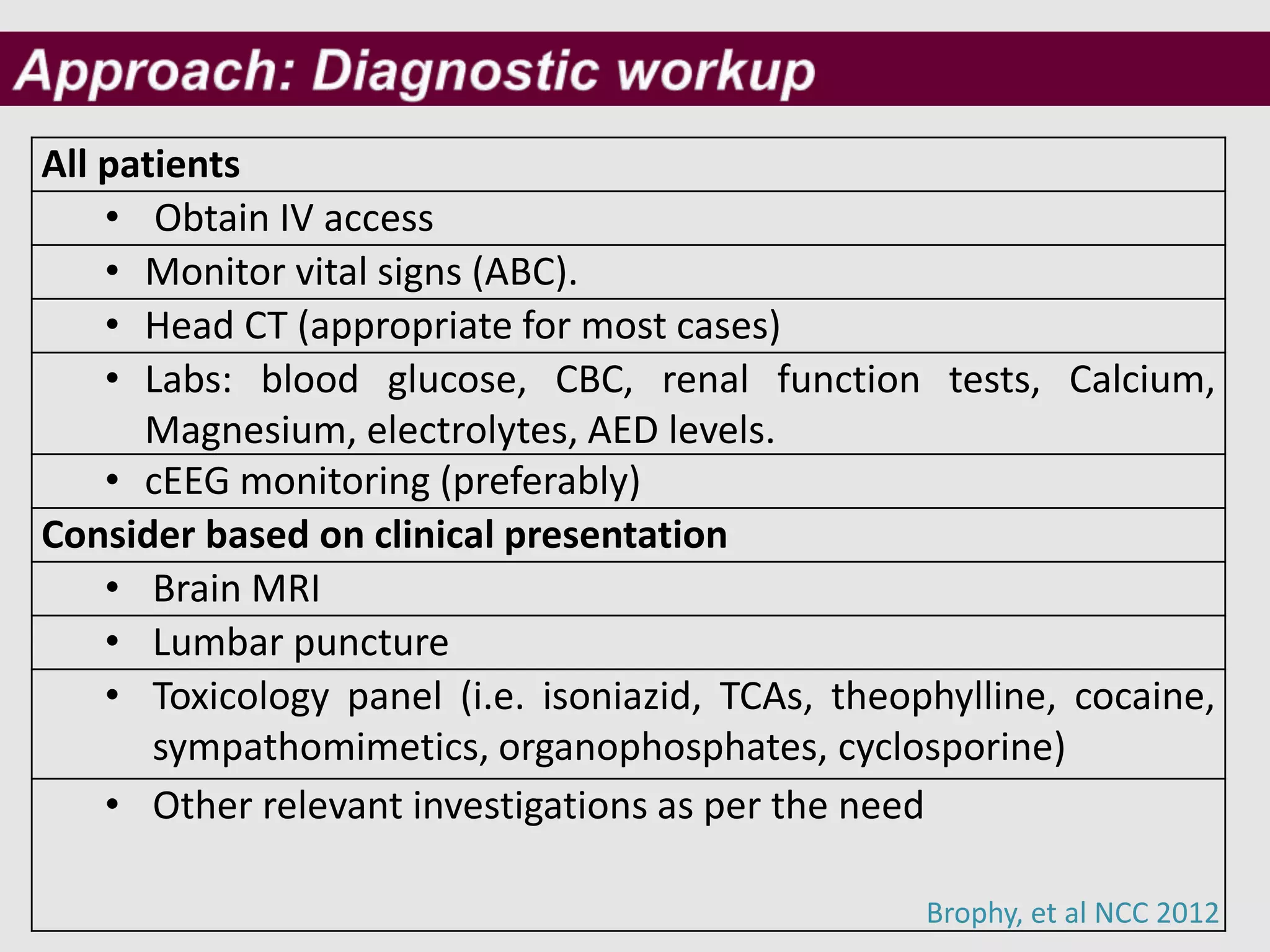
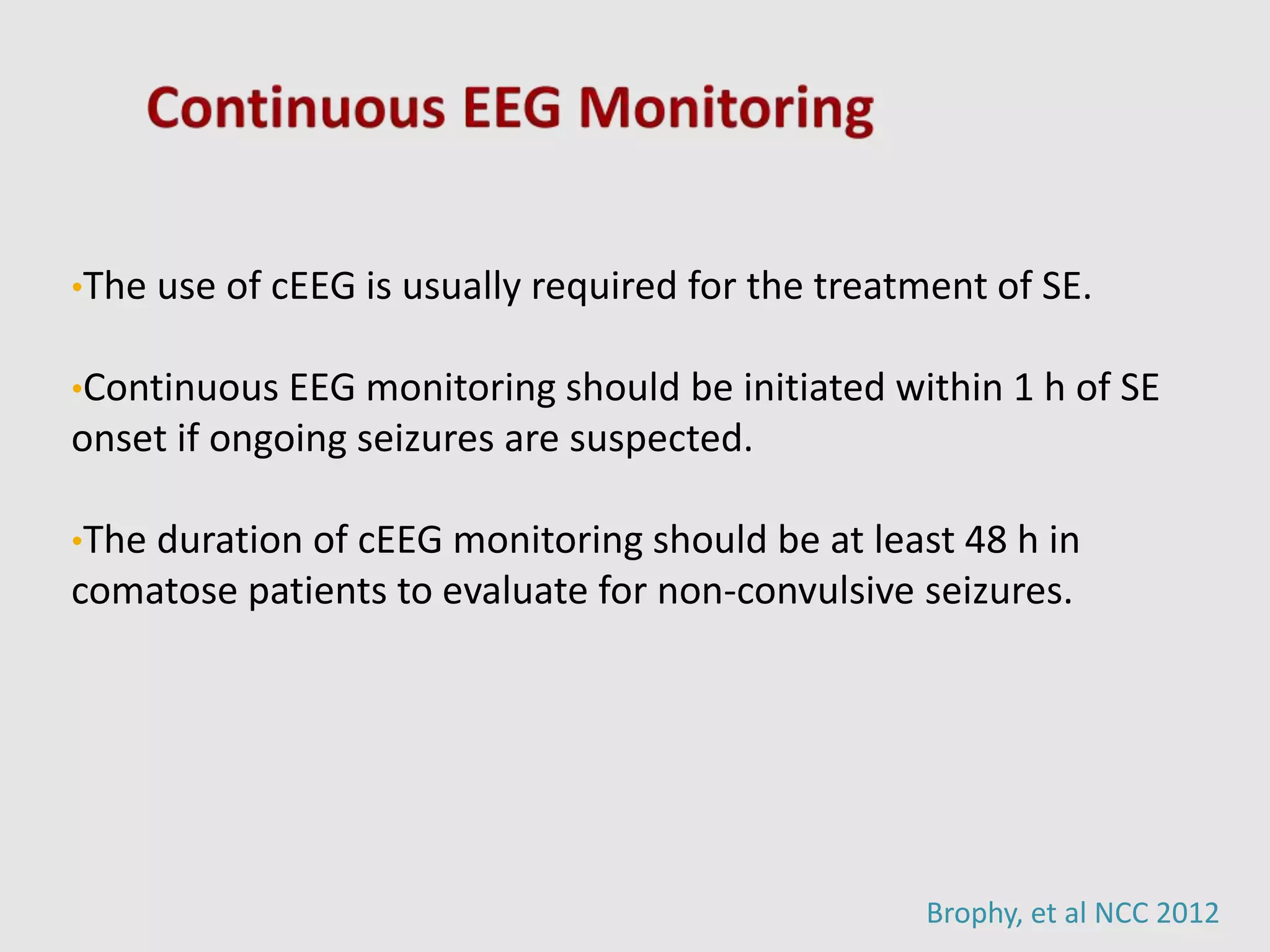
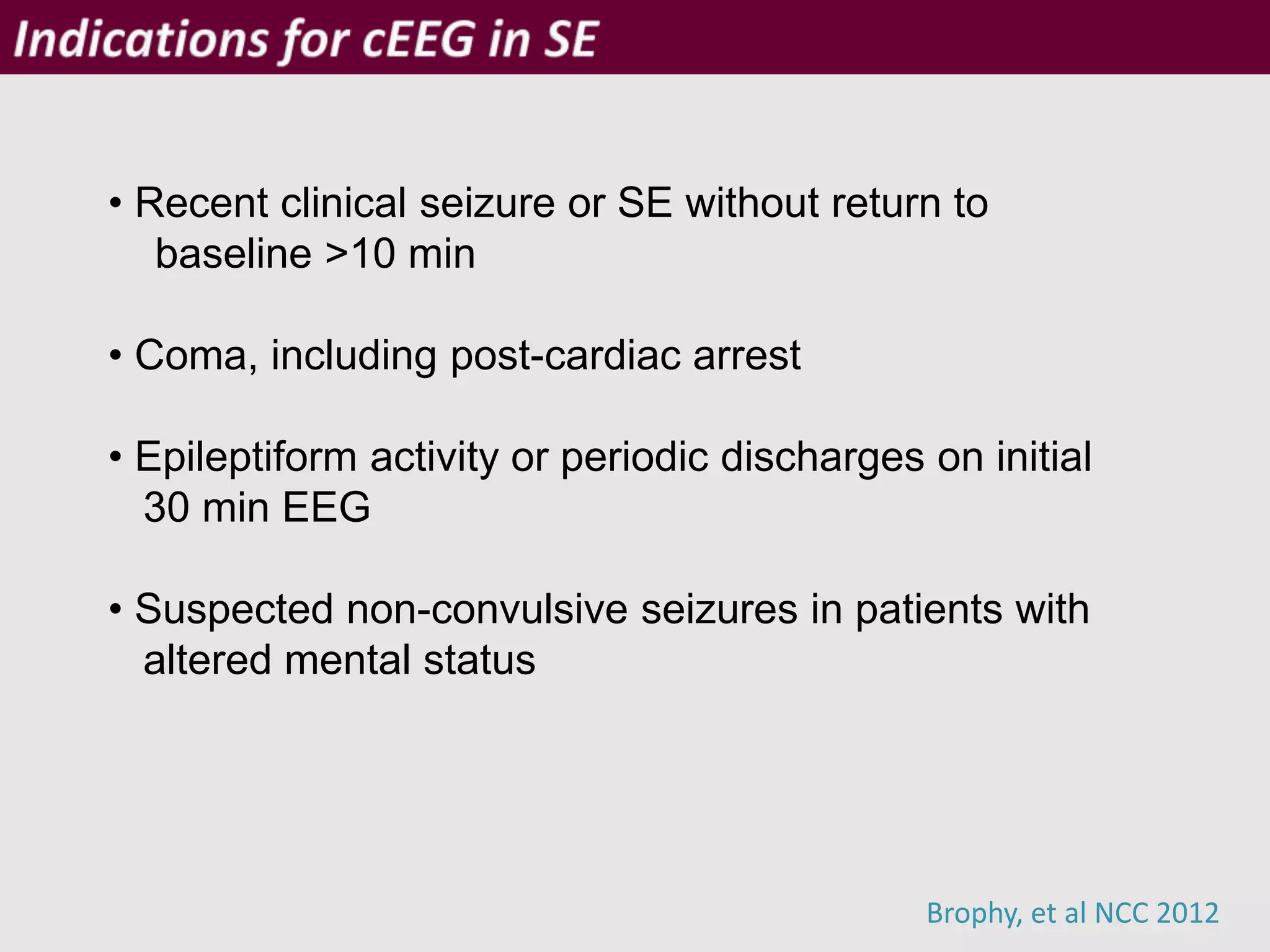
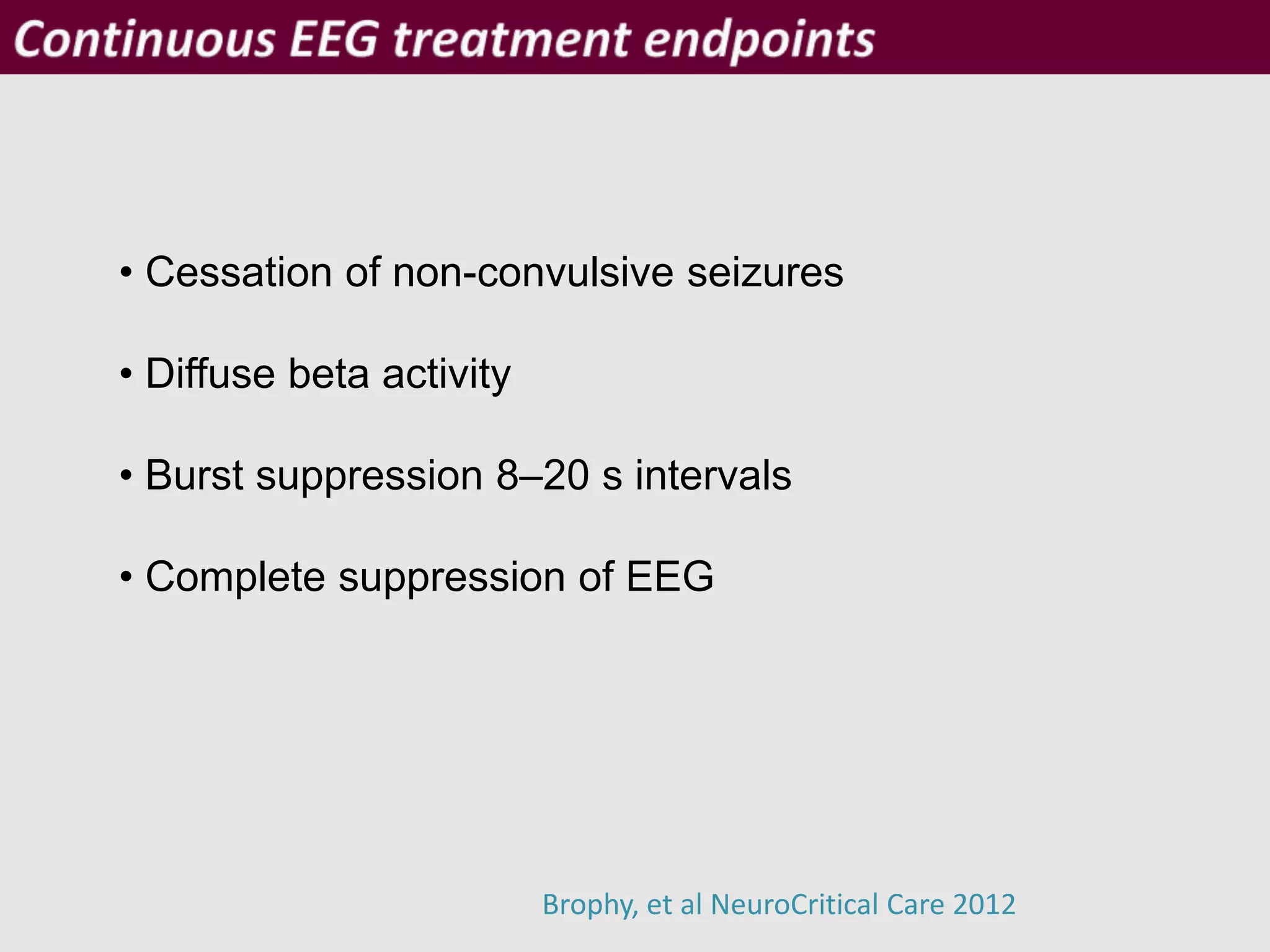
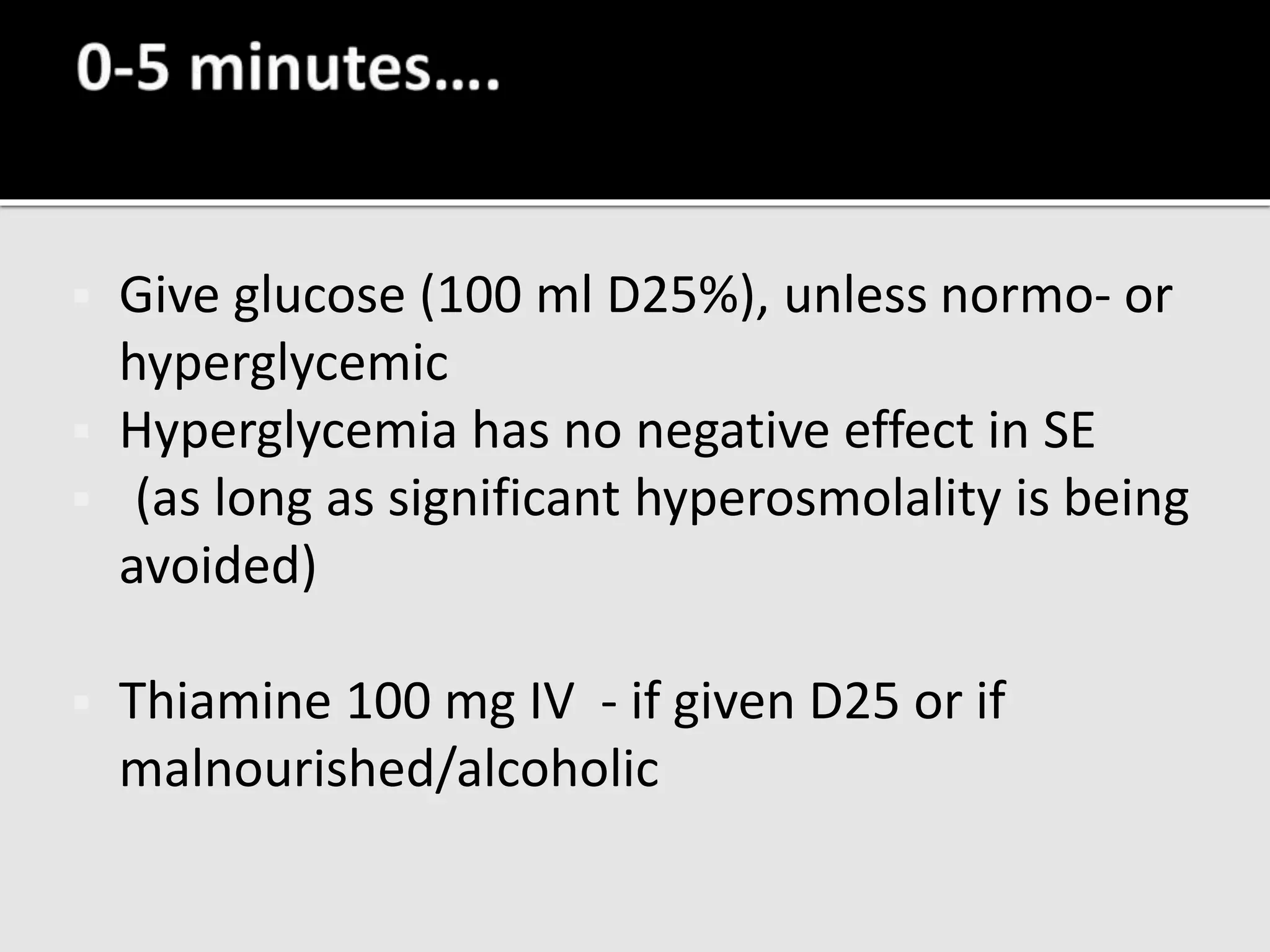
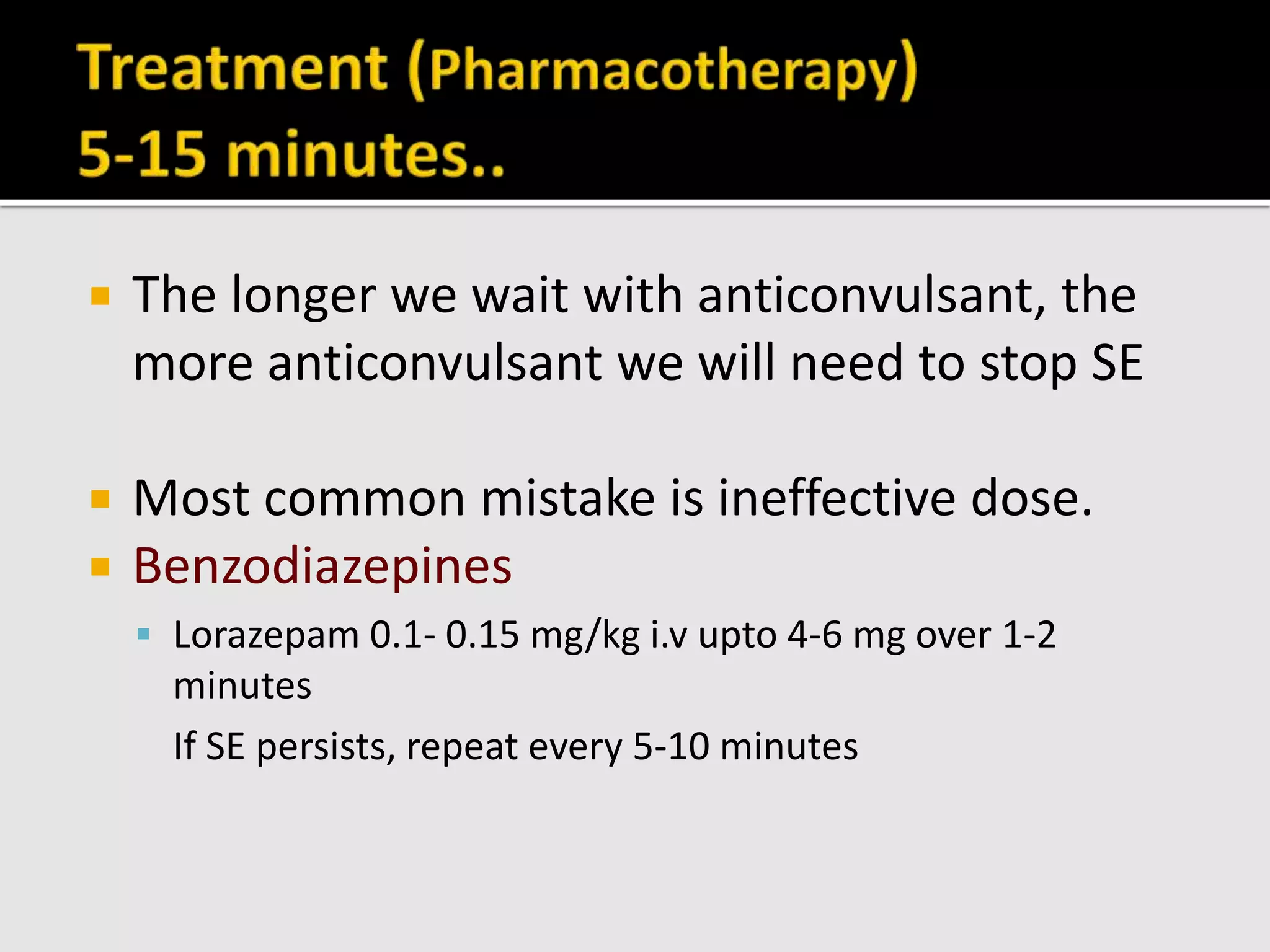
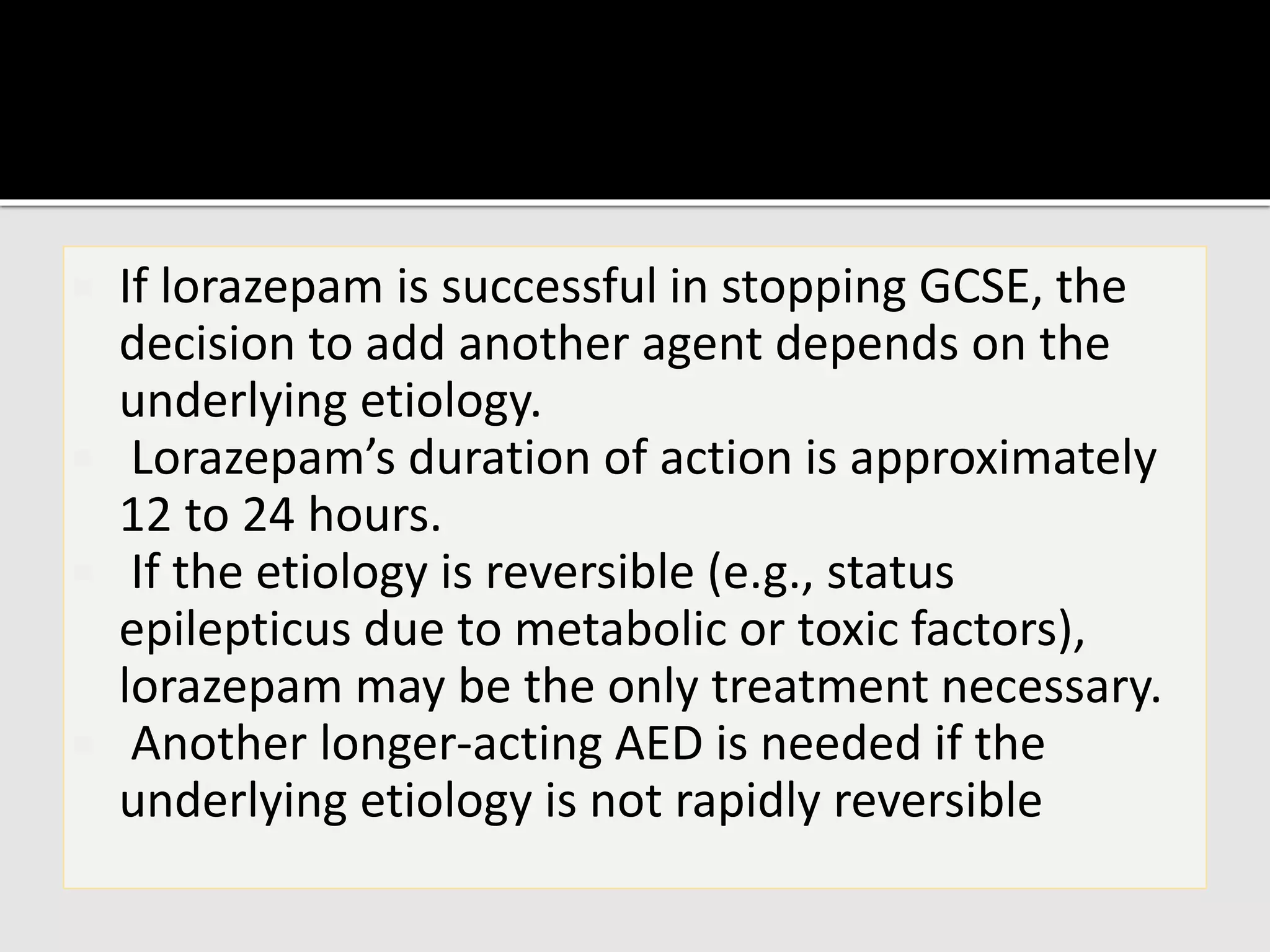
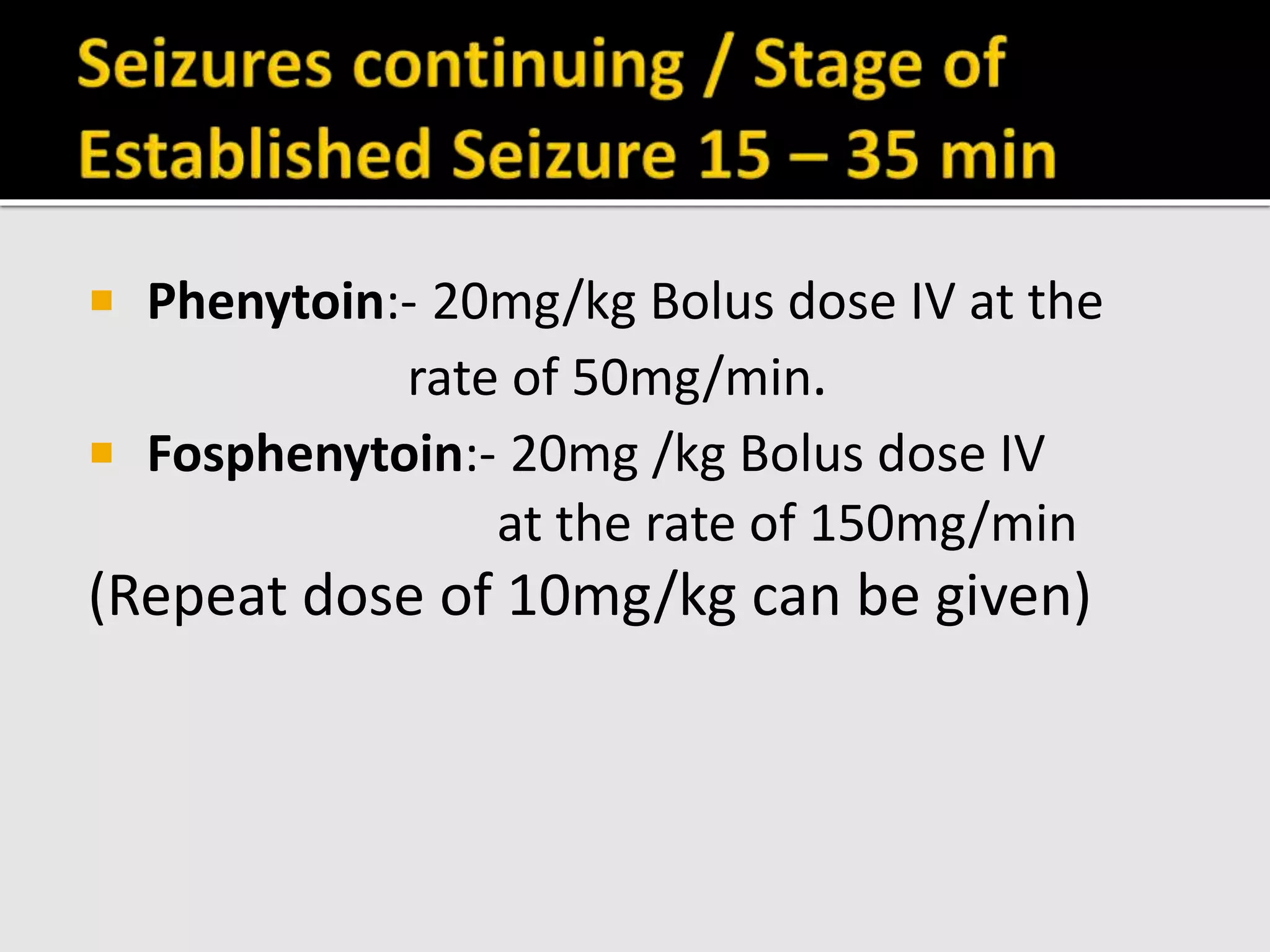
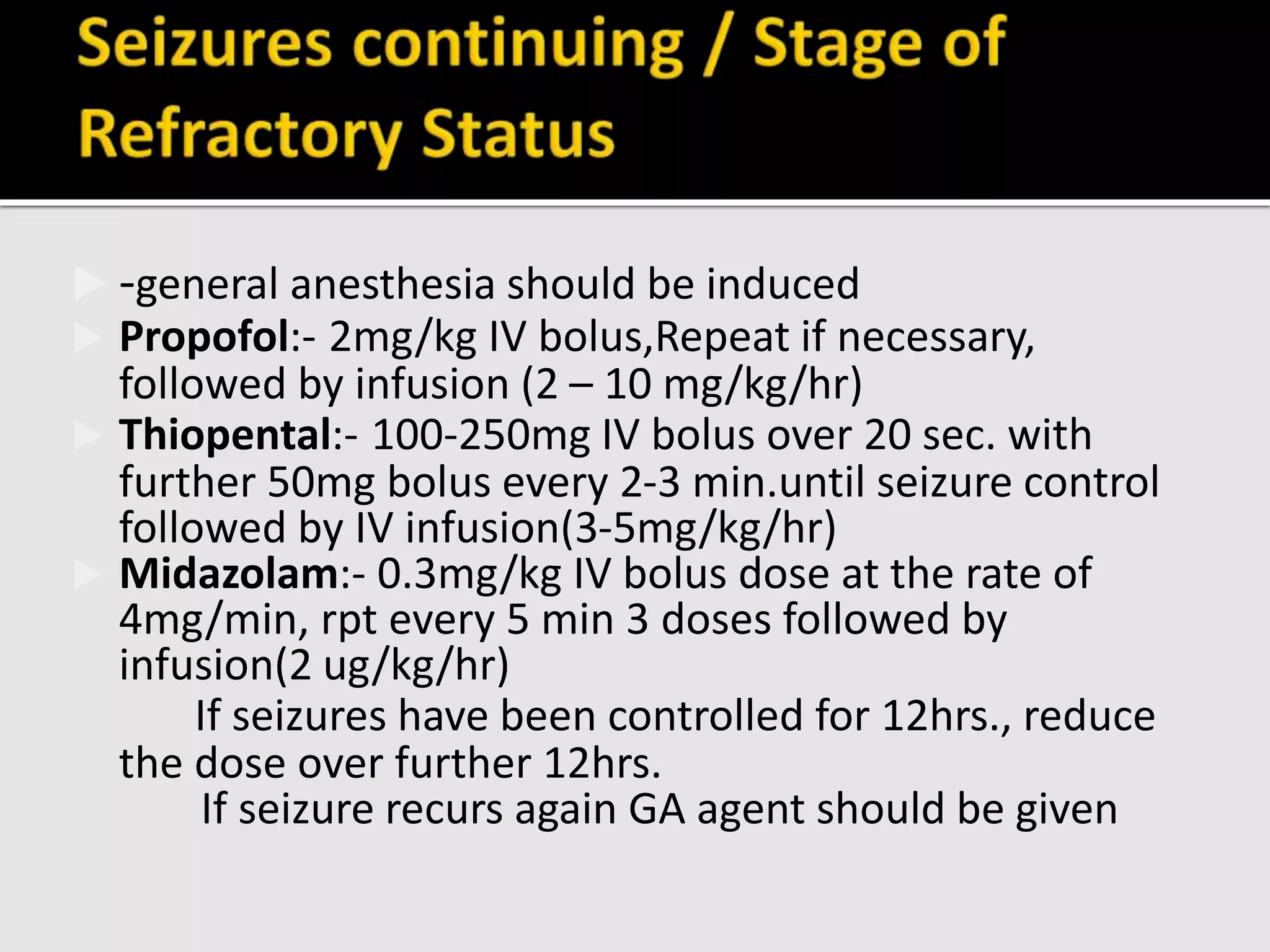
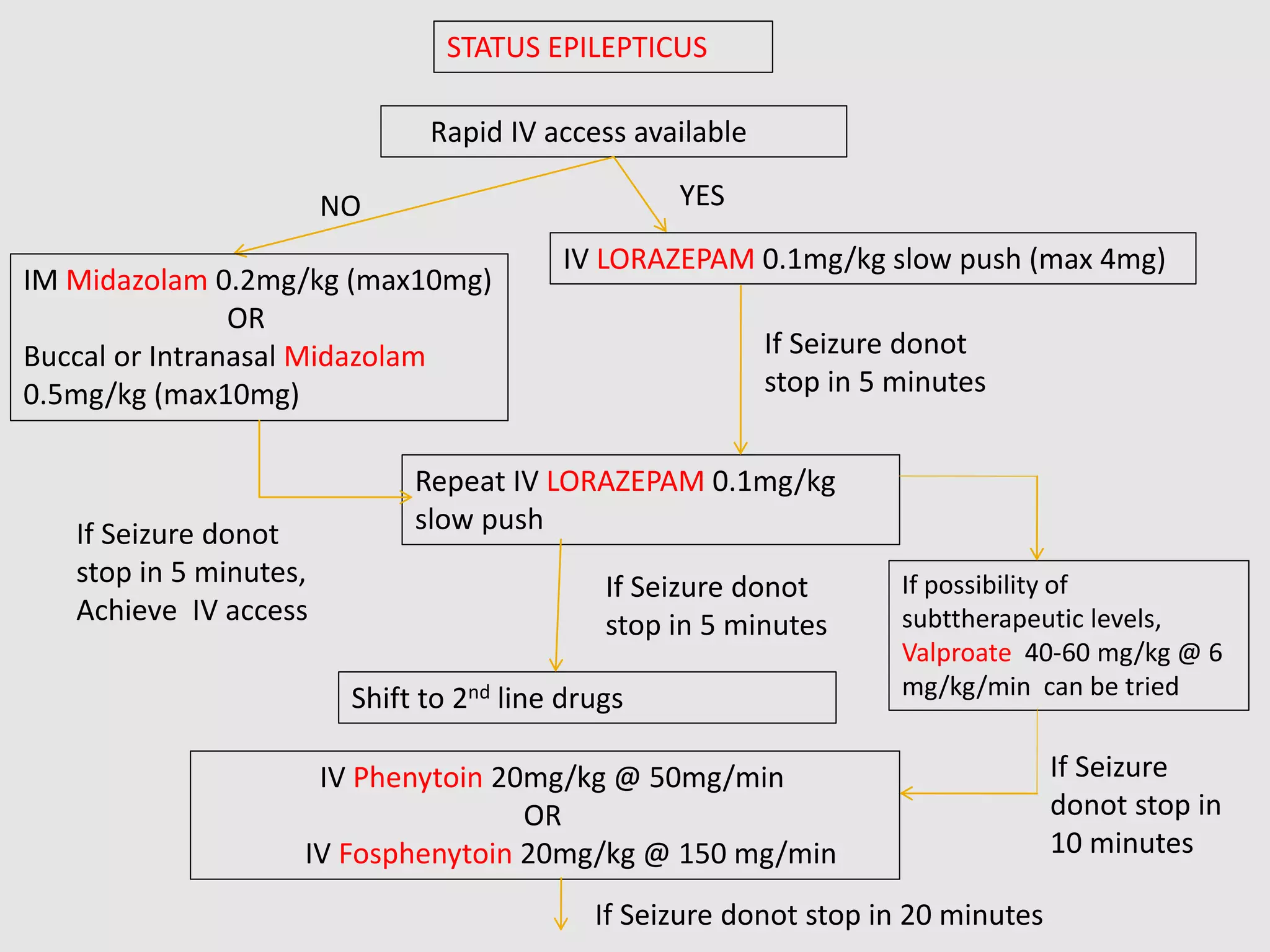
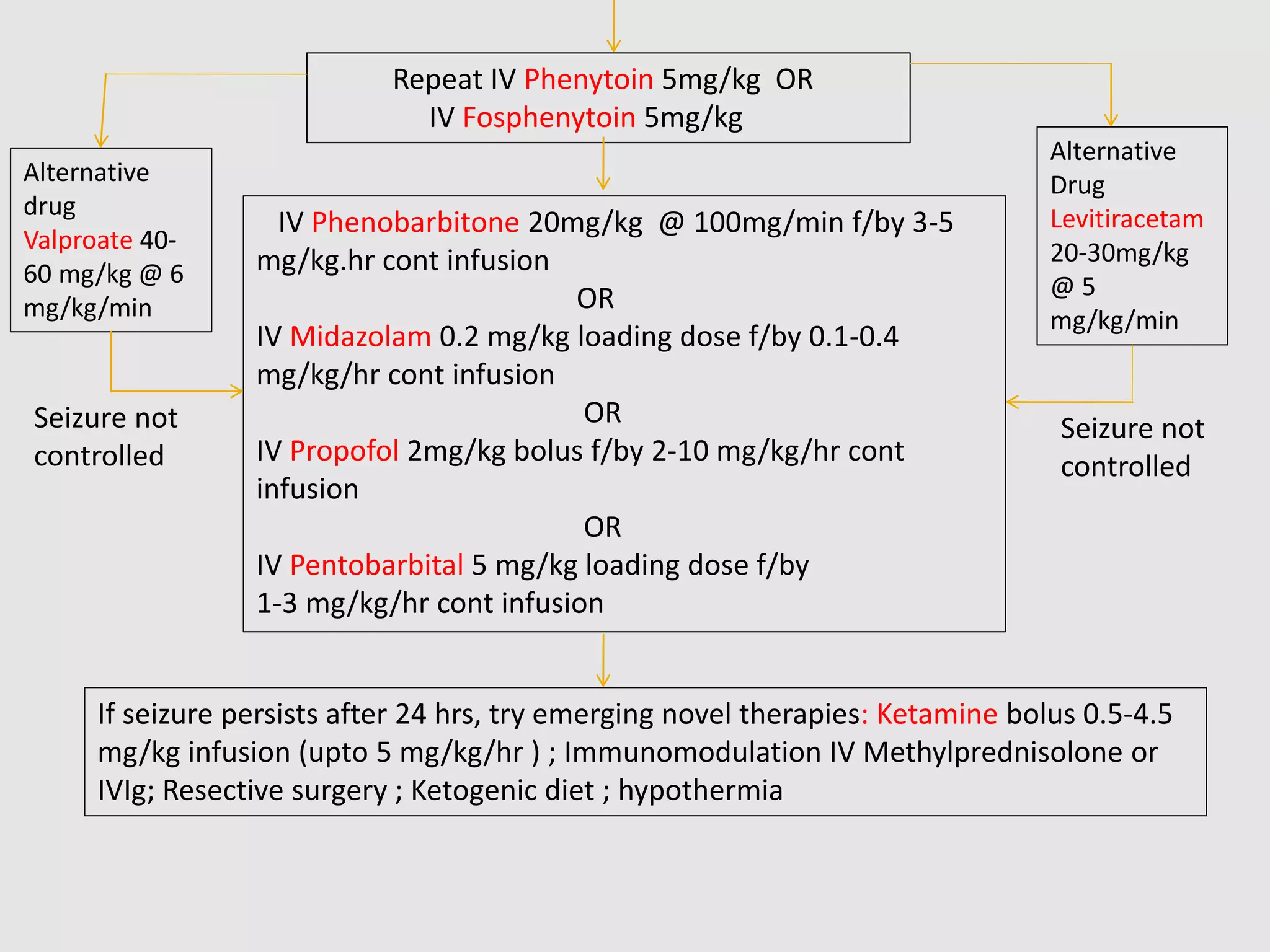
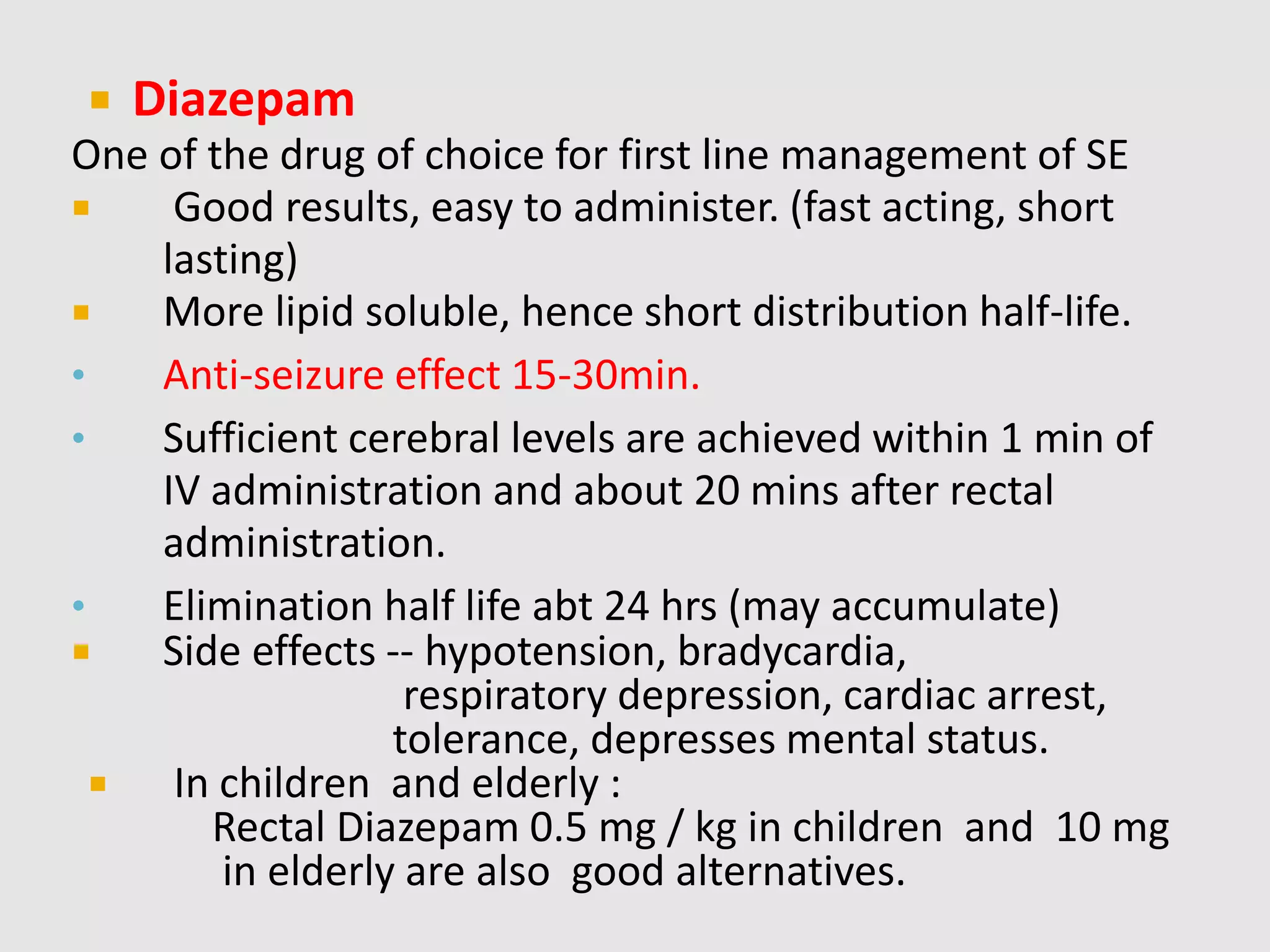
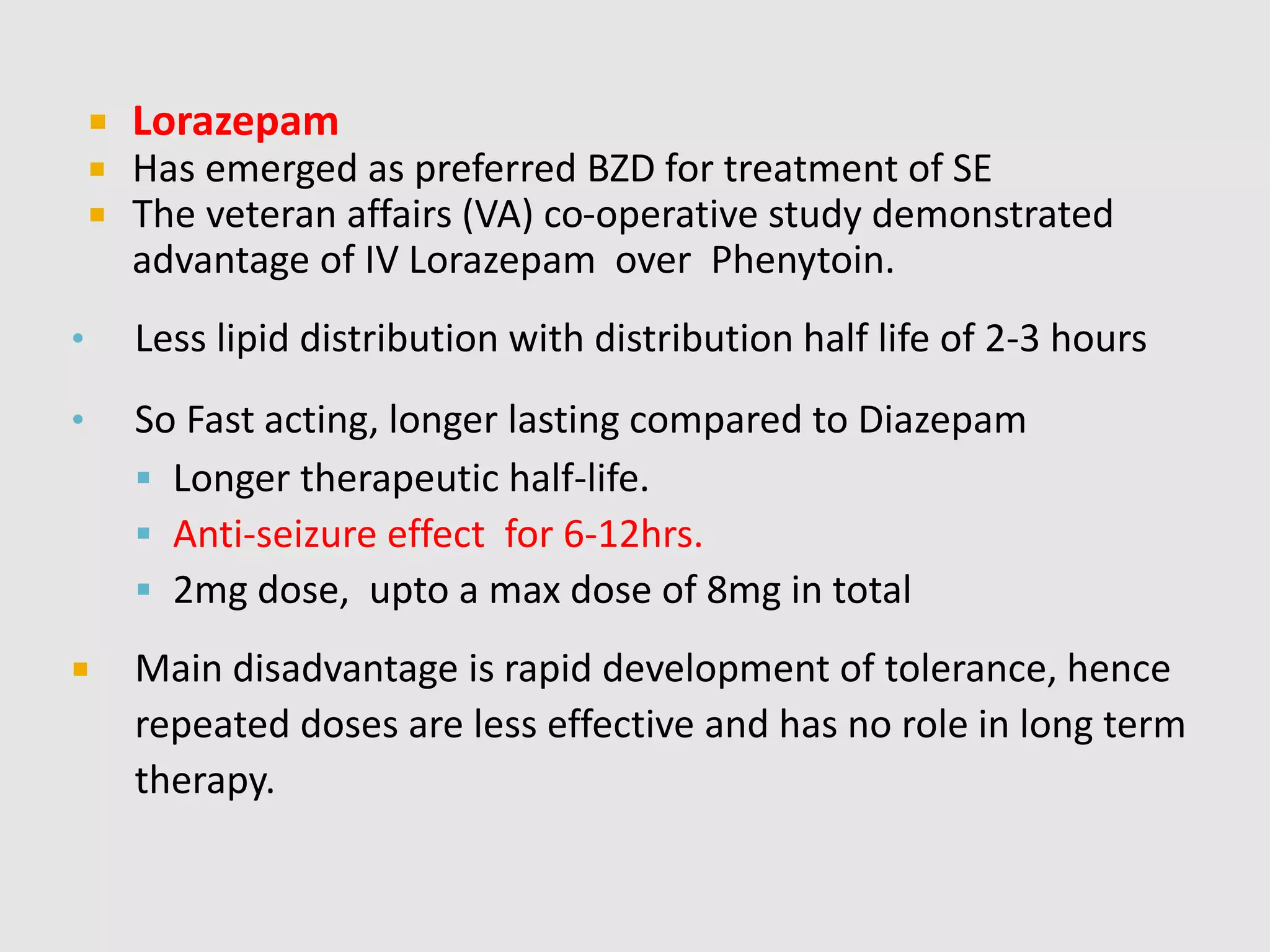
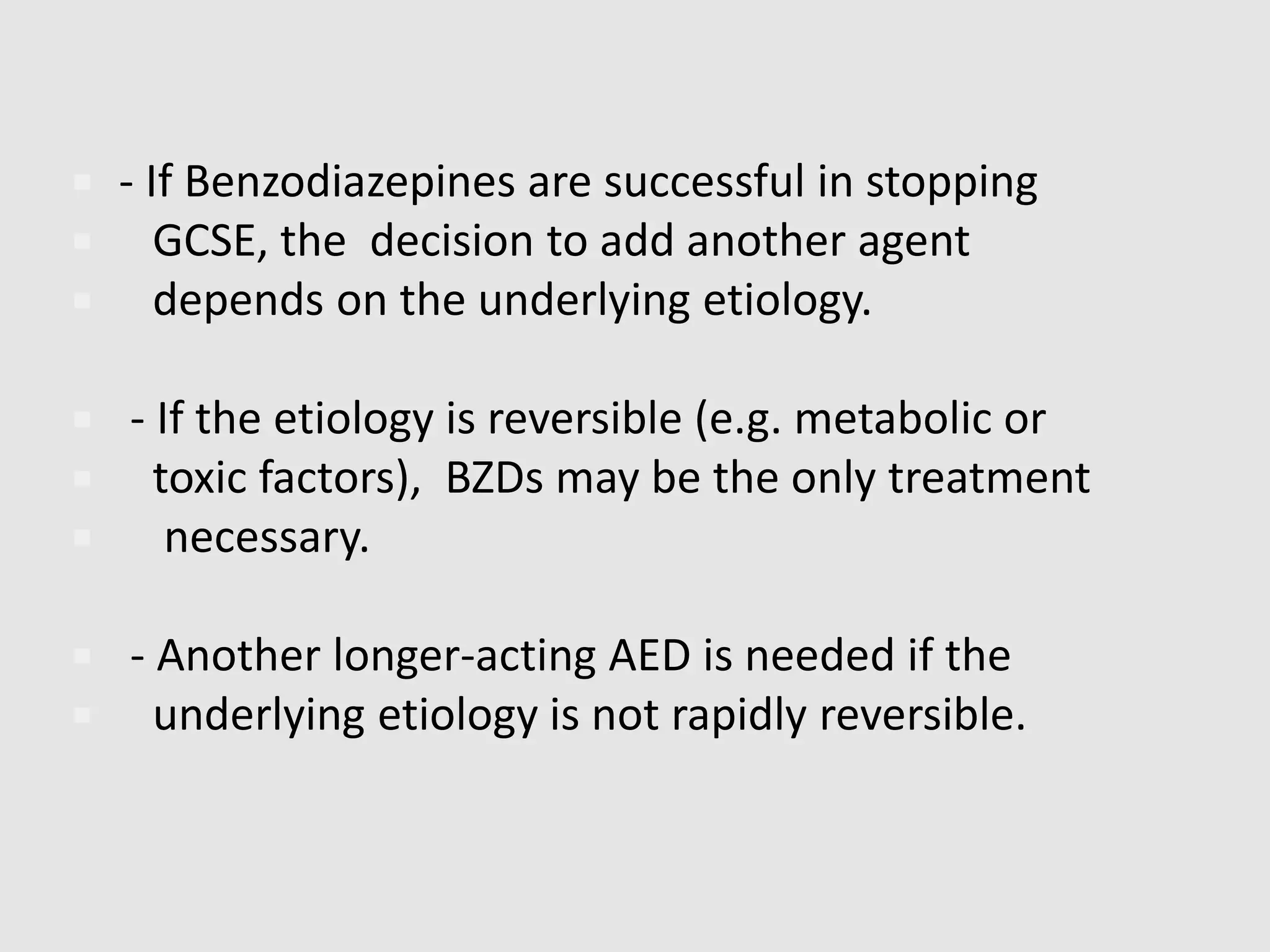
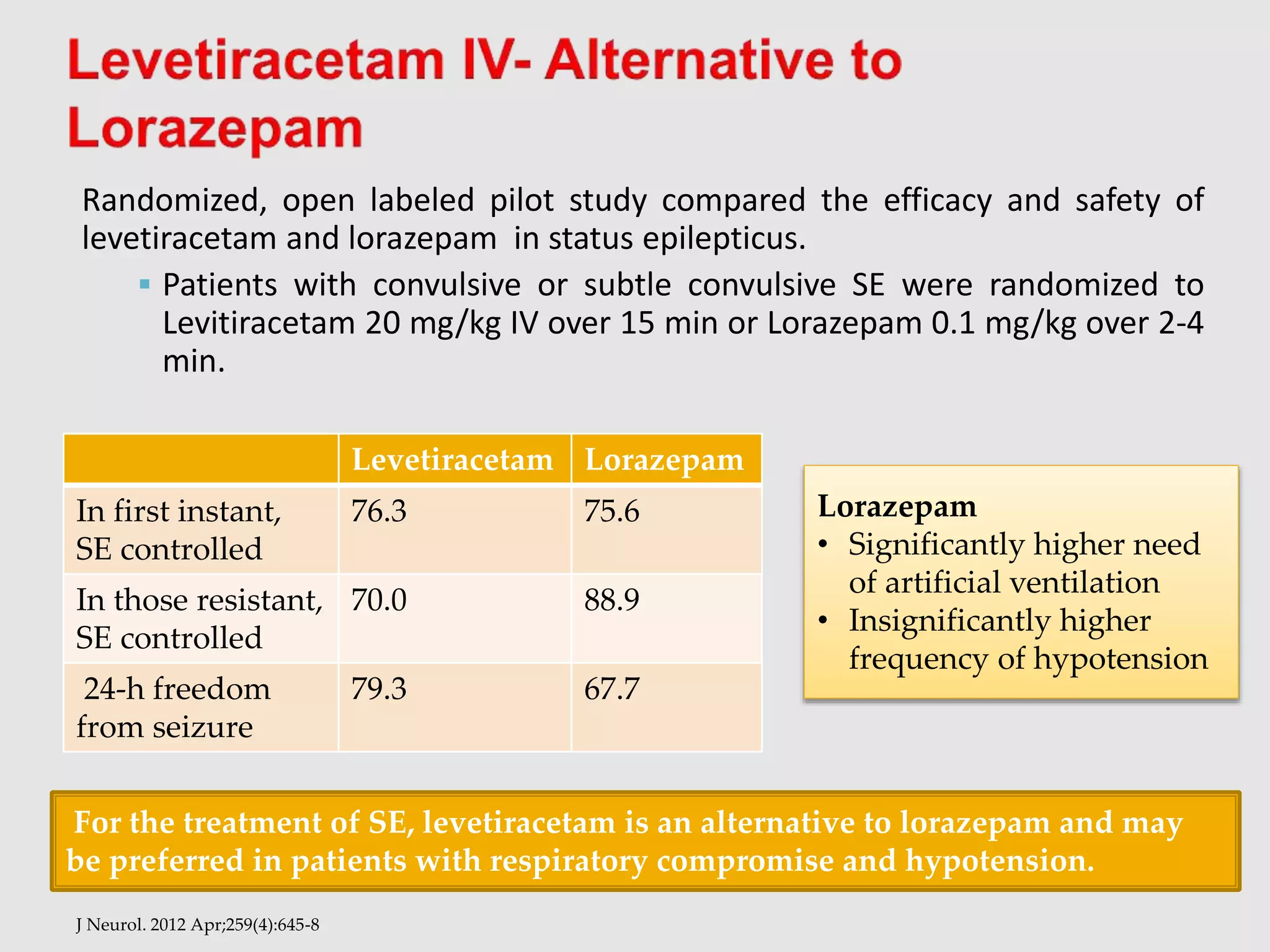
This document discusses convulsive status epilepticus (CSE). It notes that the worldwide incidence of CSE is highest in children and the elderly, with mortality rates ranging from 10.5-28% and neurological sequelae occurring in 11-16% of patients. The most common causes of CSE are listed as low anti-epileptic drug levels, stroke, alcohol withdrawal, anoxic brain injury, and metabolic disturbances. The document provides details on the definition, types, risk factors, complications, management, and treatment of CSE.