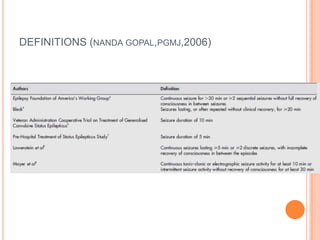
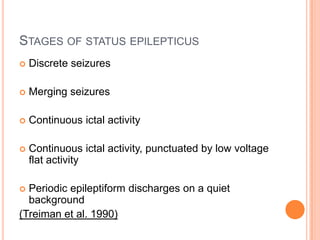
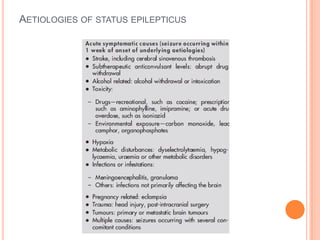
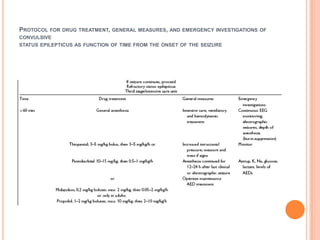
1. Status epilepticus (SE) is a medical emergency defined as a seizure lasting more than 5 minutes or recurrent seizures without regaining consciousness. SE can be convulsive or non-convulsive.
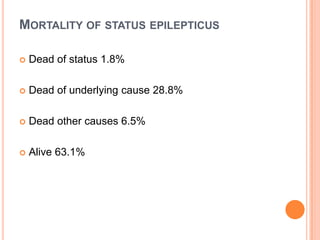
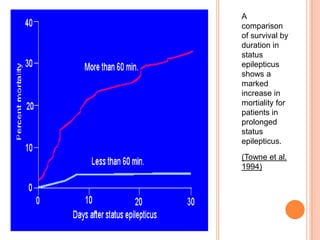
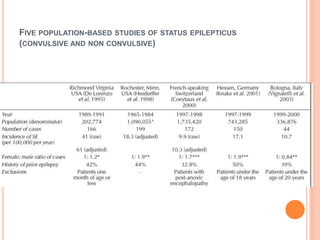
2. The annual incidence of SE is estimated to be between 9,000-14,000 new cases per year in the UK. Mortality is about 20-30% and is higher in the elderly.
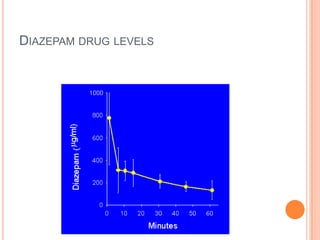
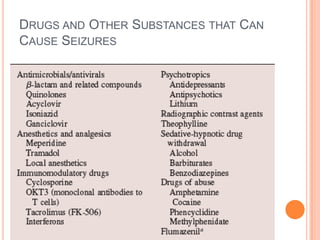
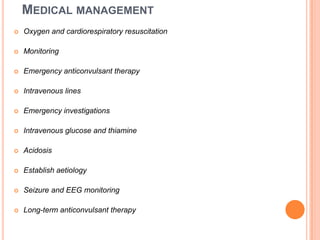
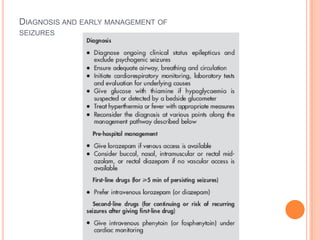
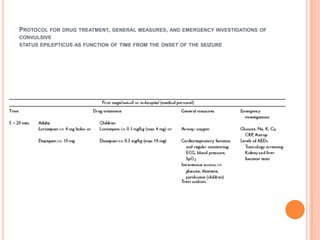
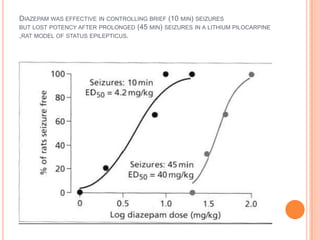
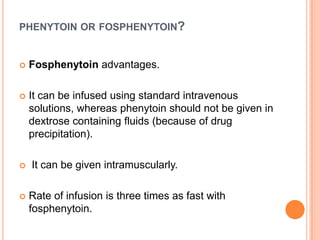
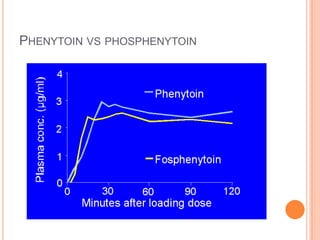
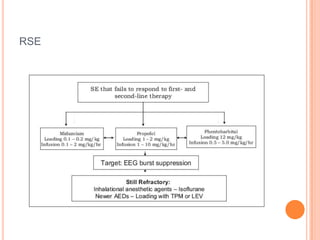
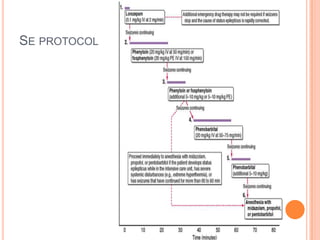
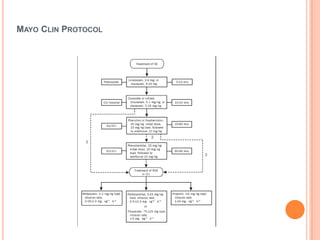
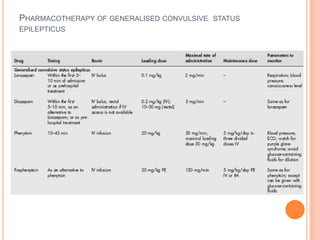
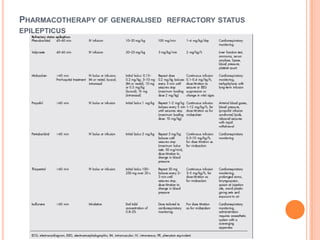
3. SE is initially treated with benzodiazepines like lorazepam or diazepam. If seizures continue, second line drugs like fosphenytoin or phenytoin are used. For refractory SE, anesthetic drugs under ICU care may be required