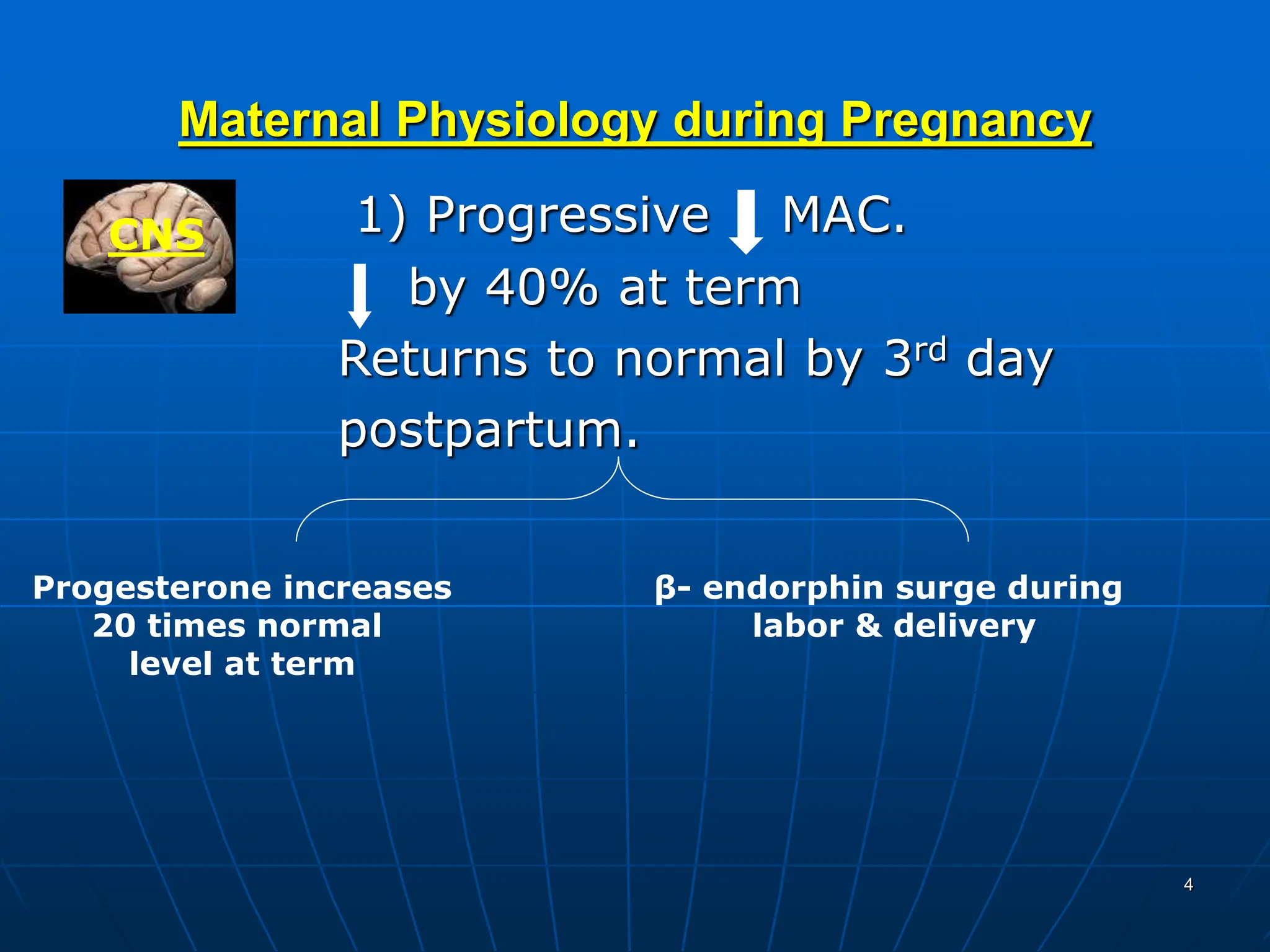
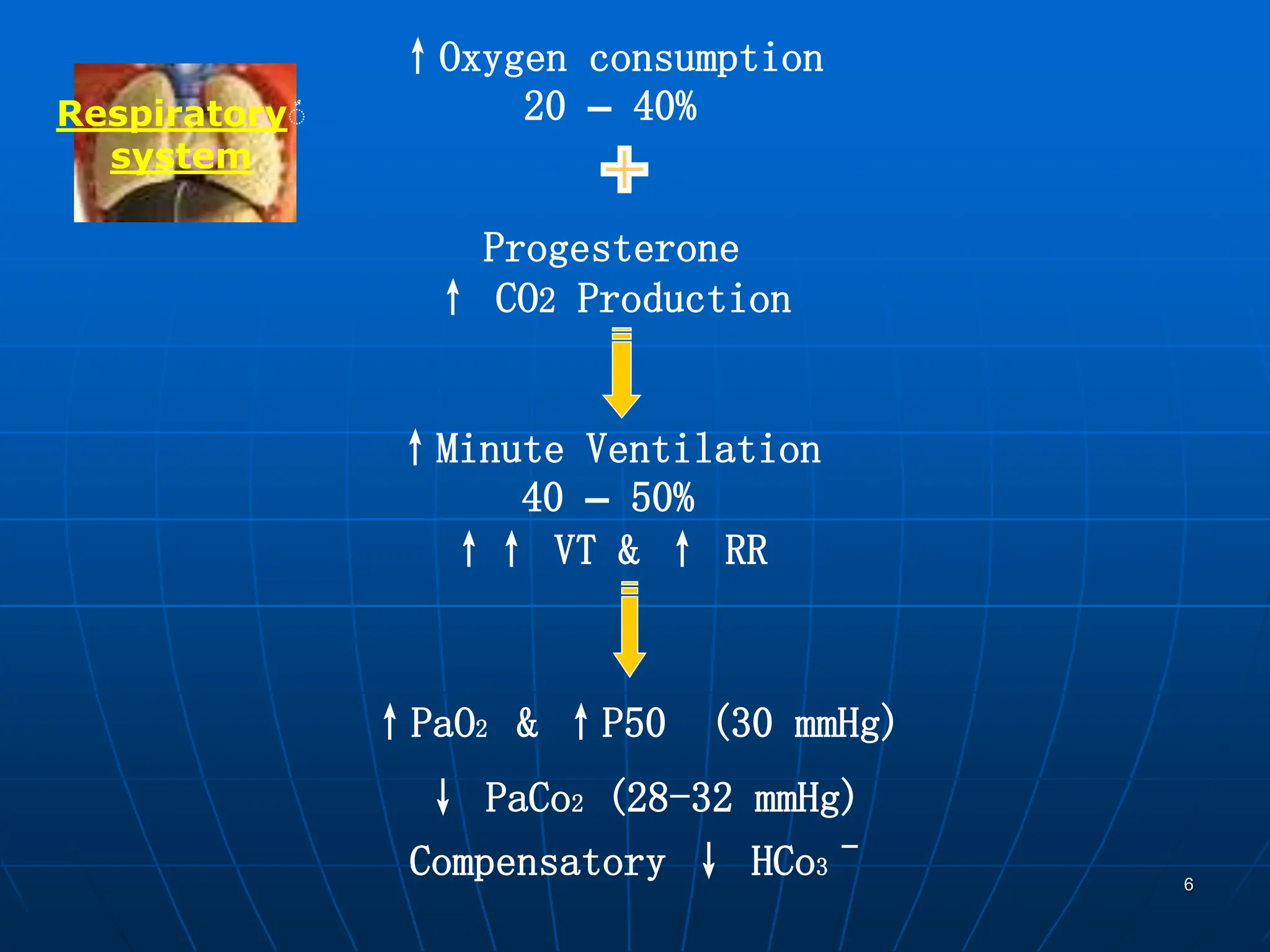
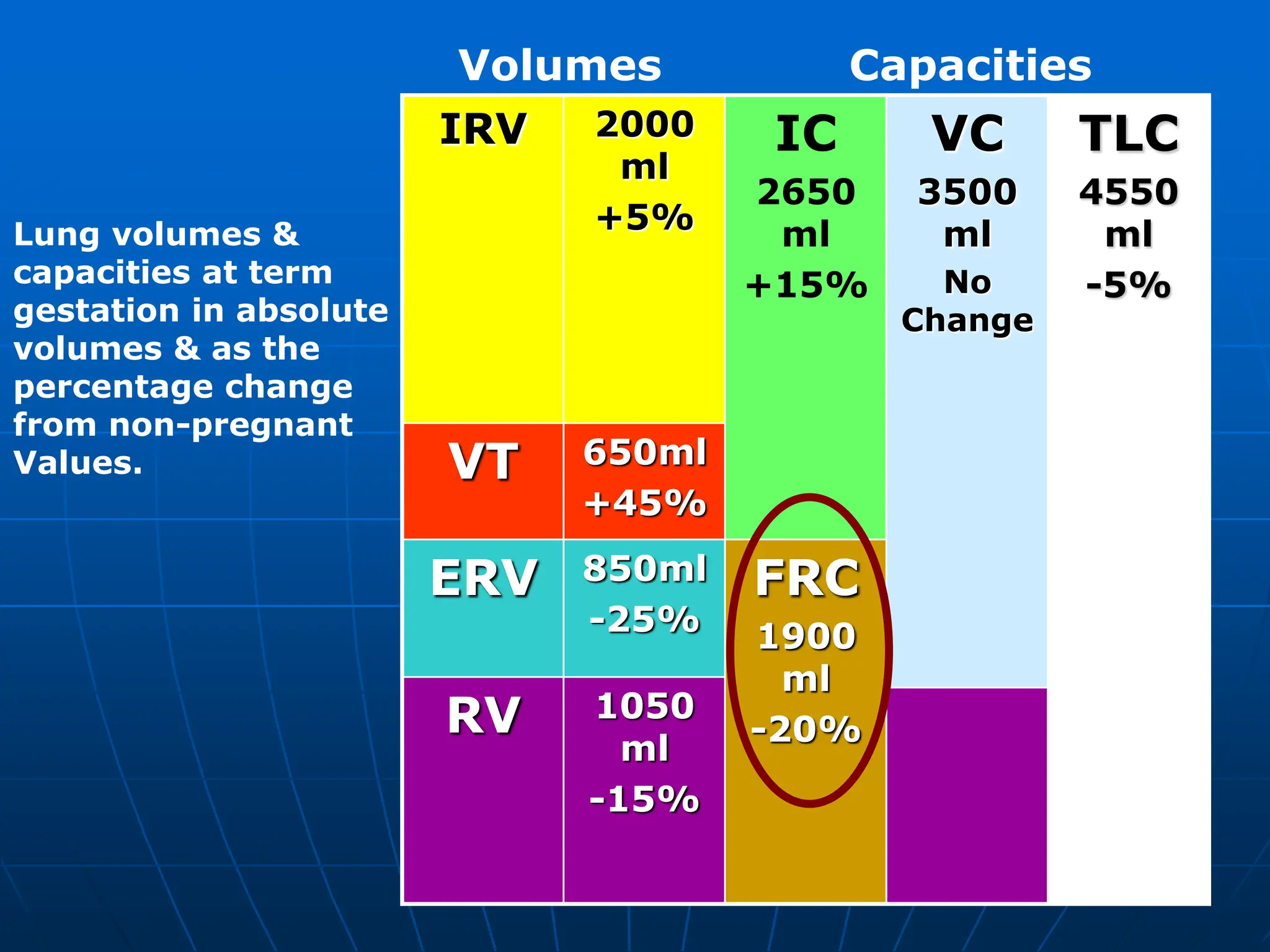
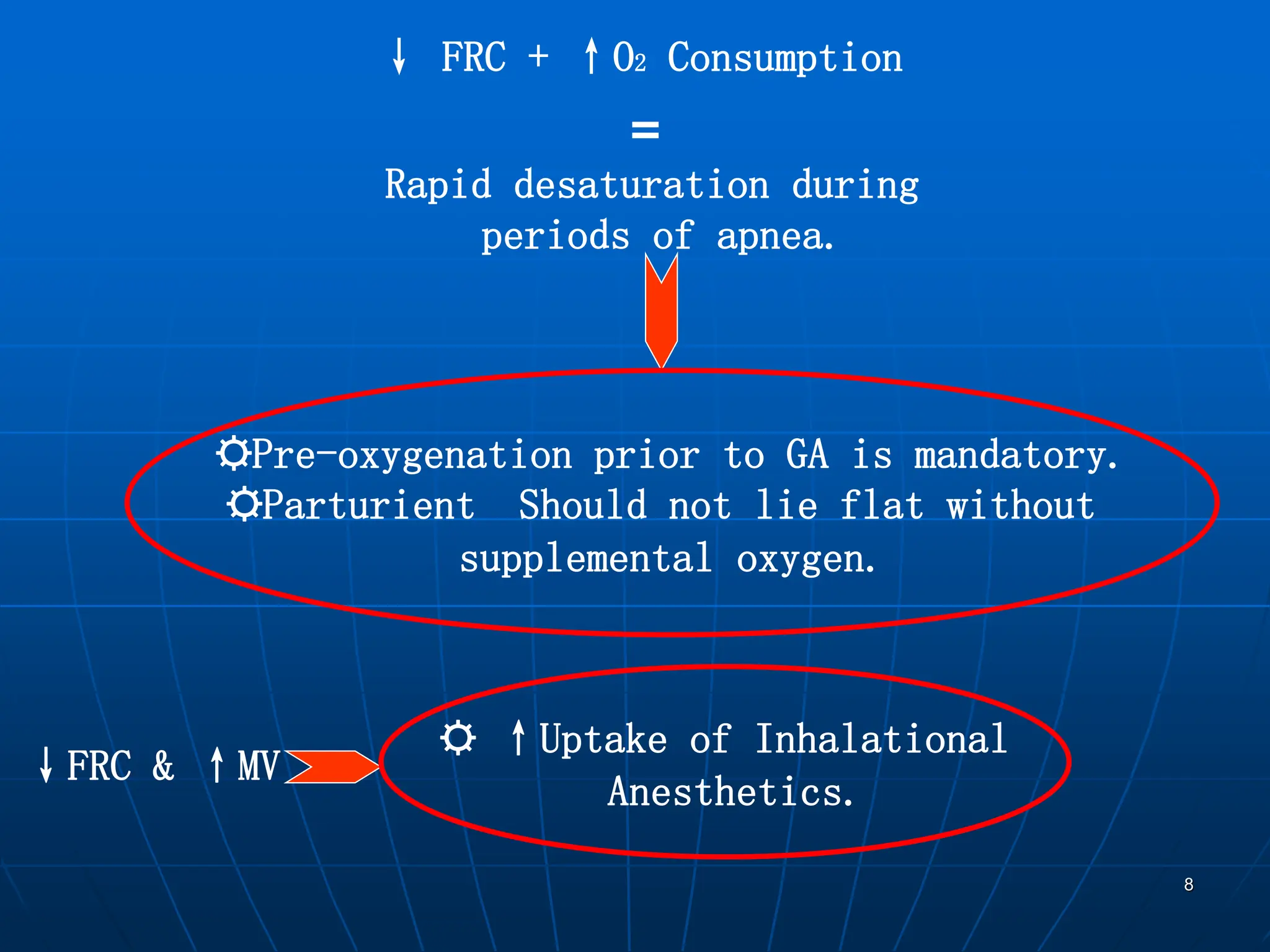
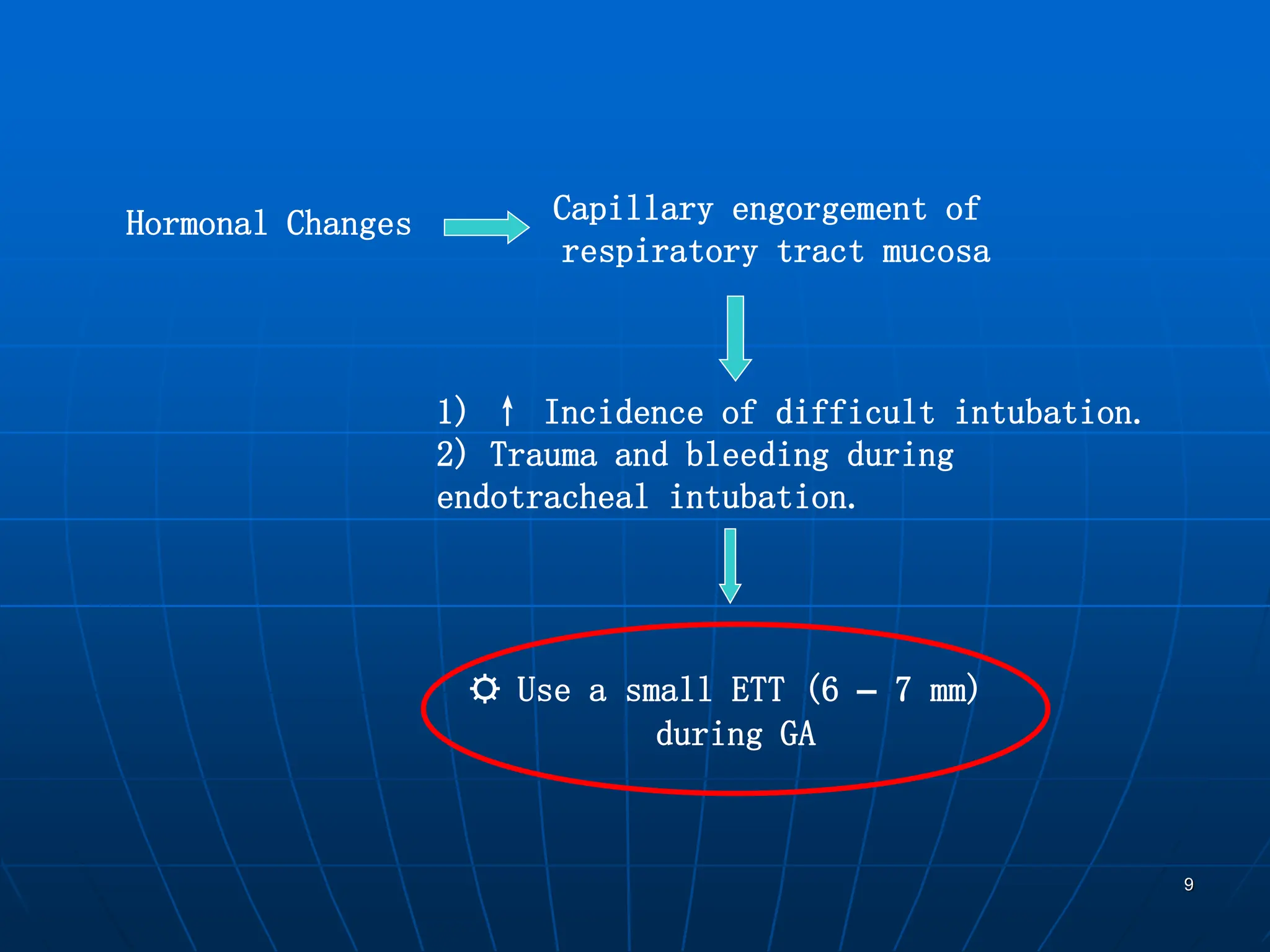
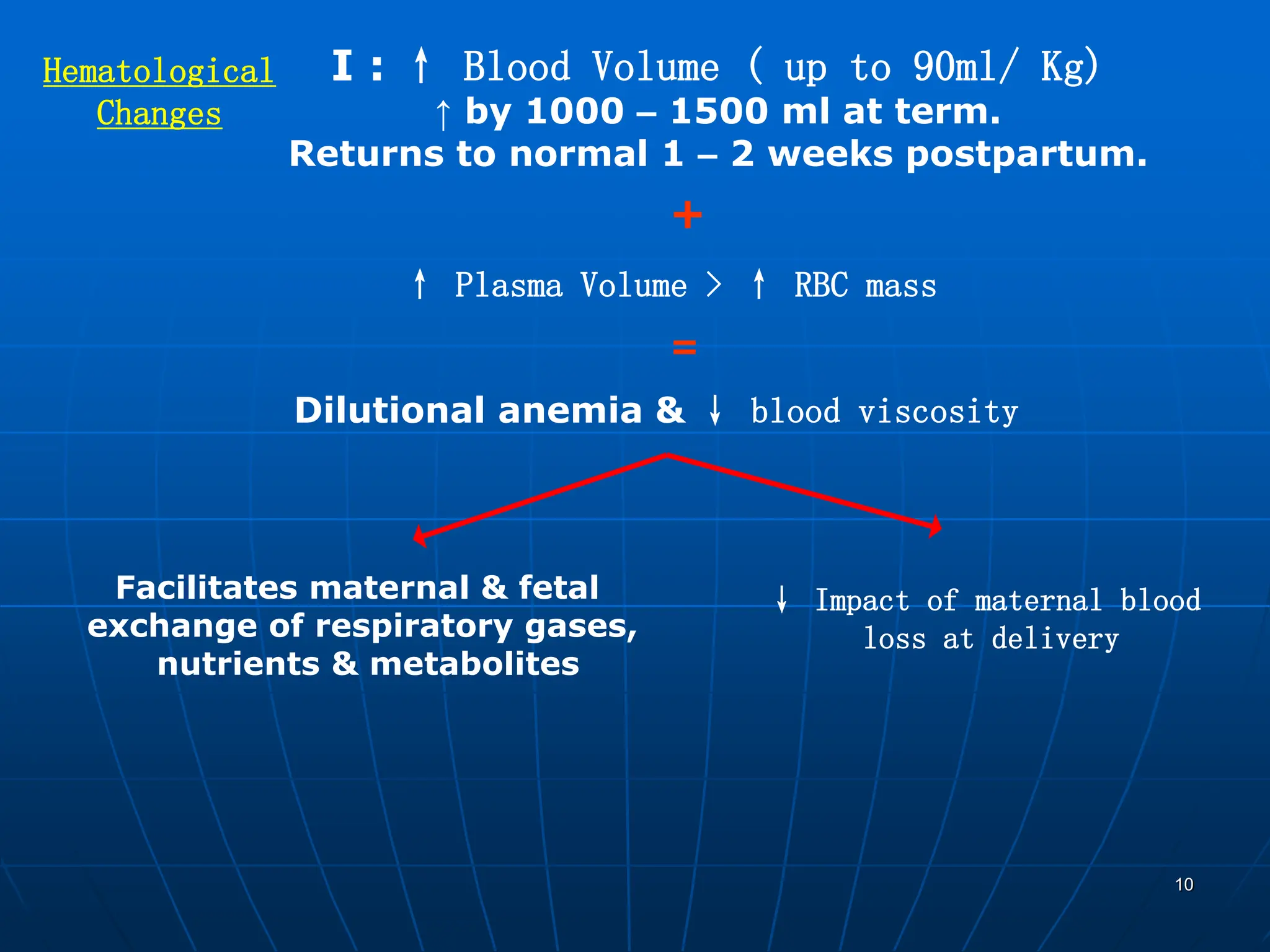
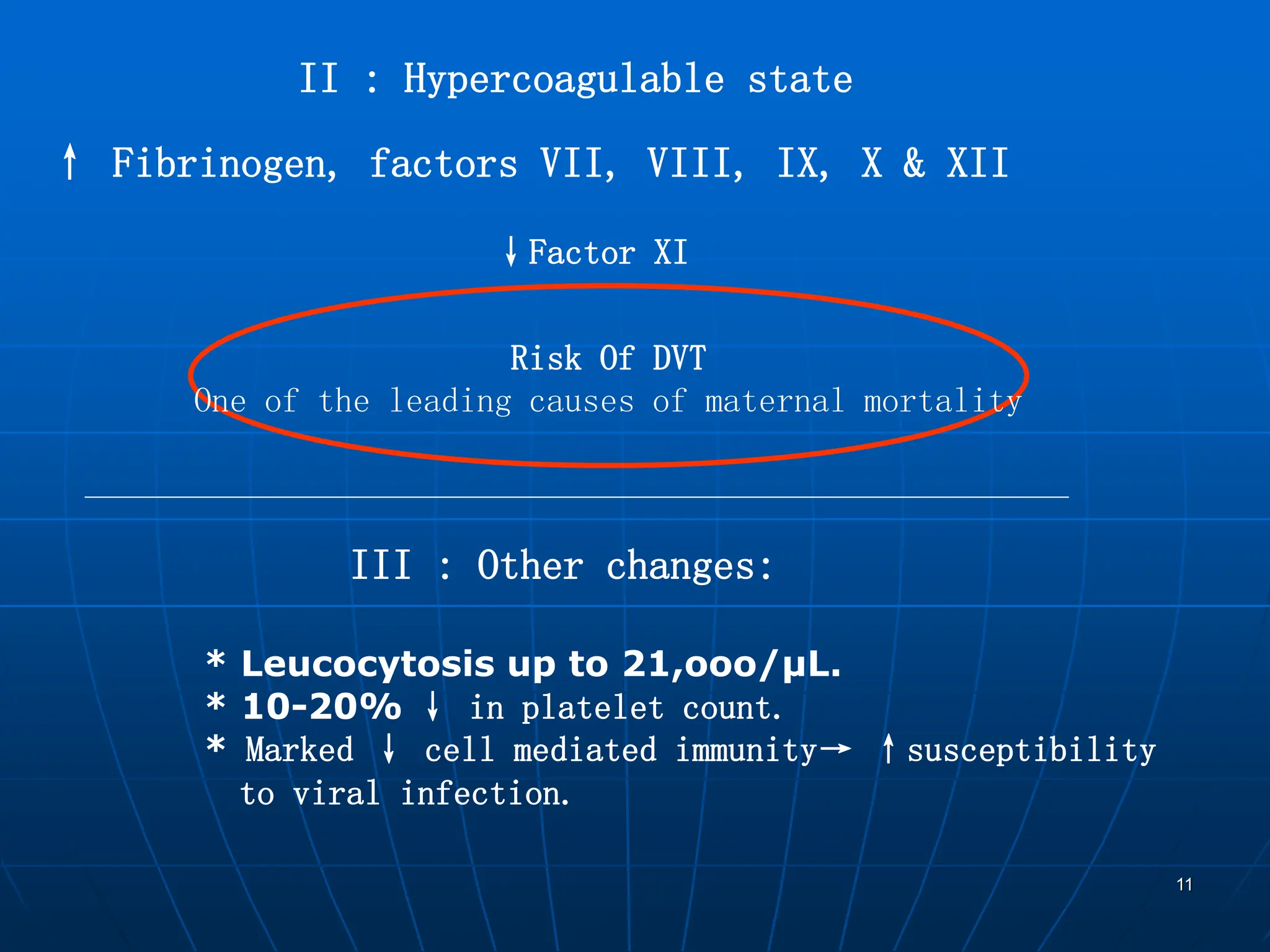
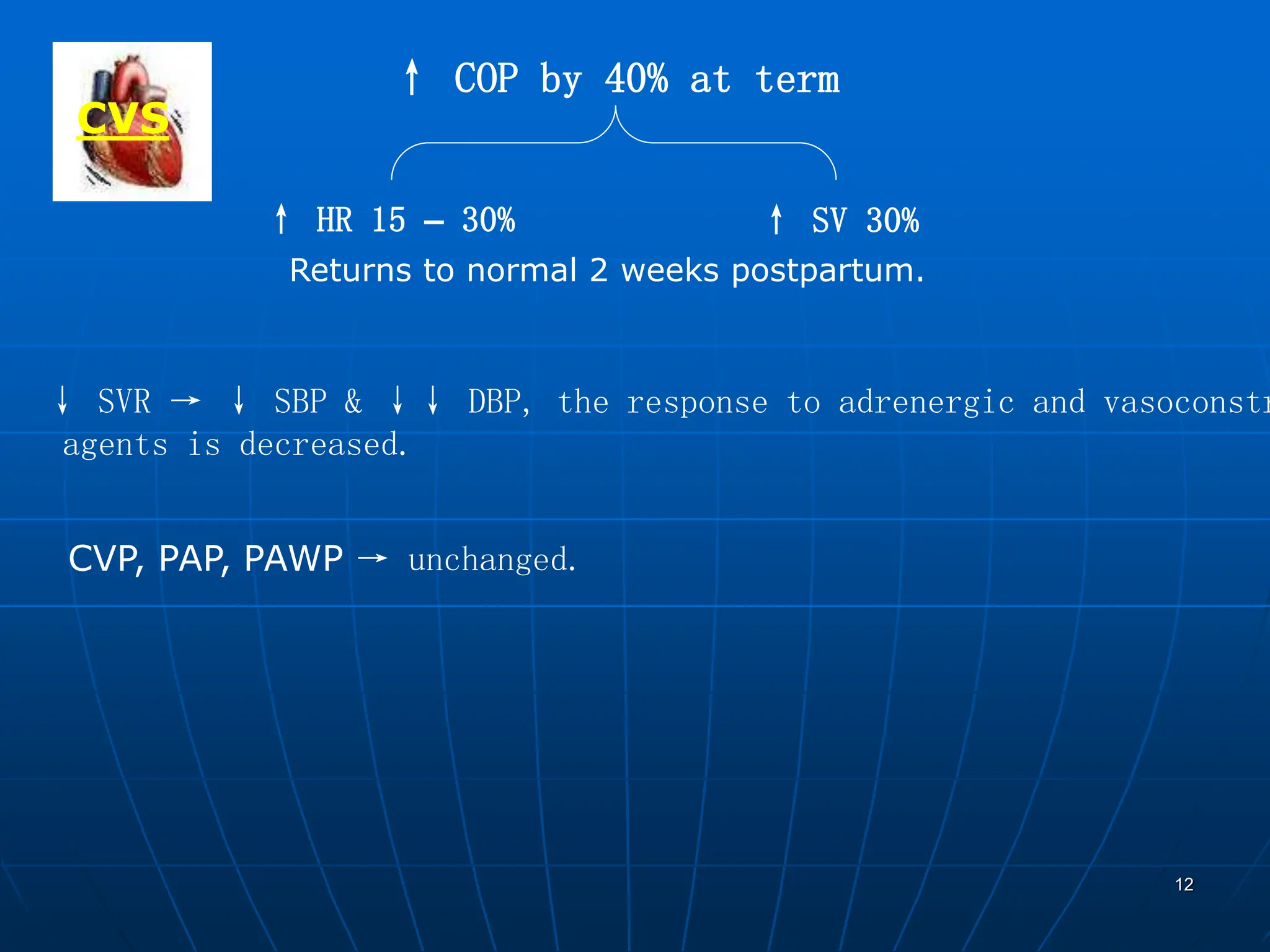
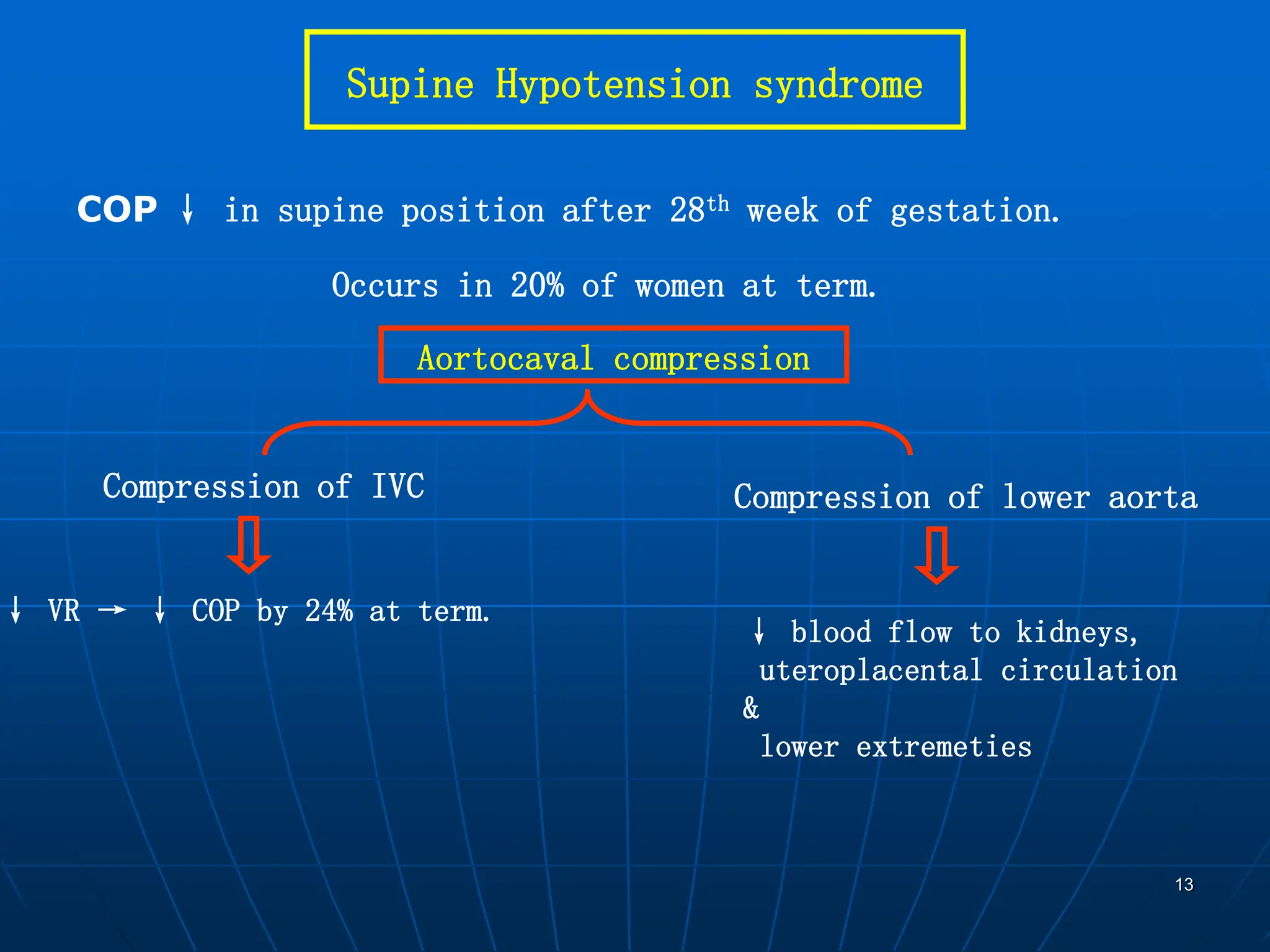
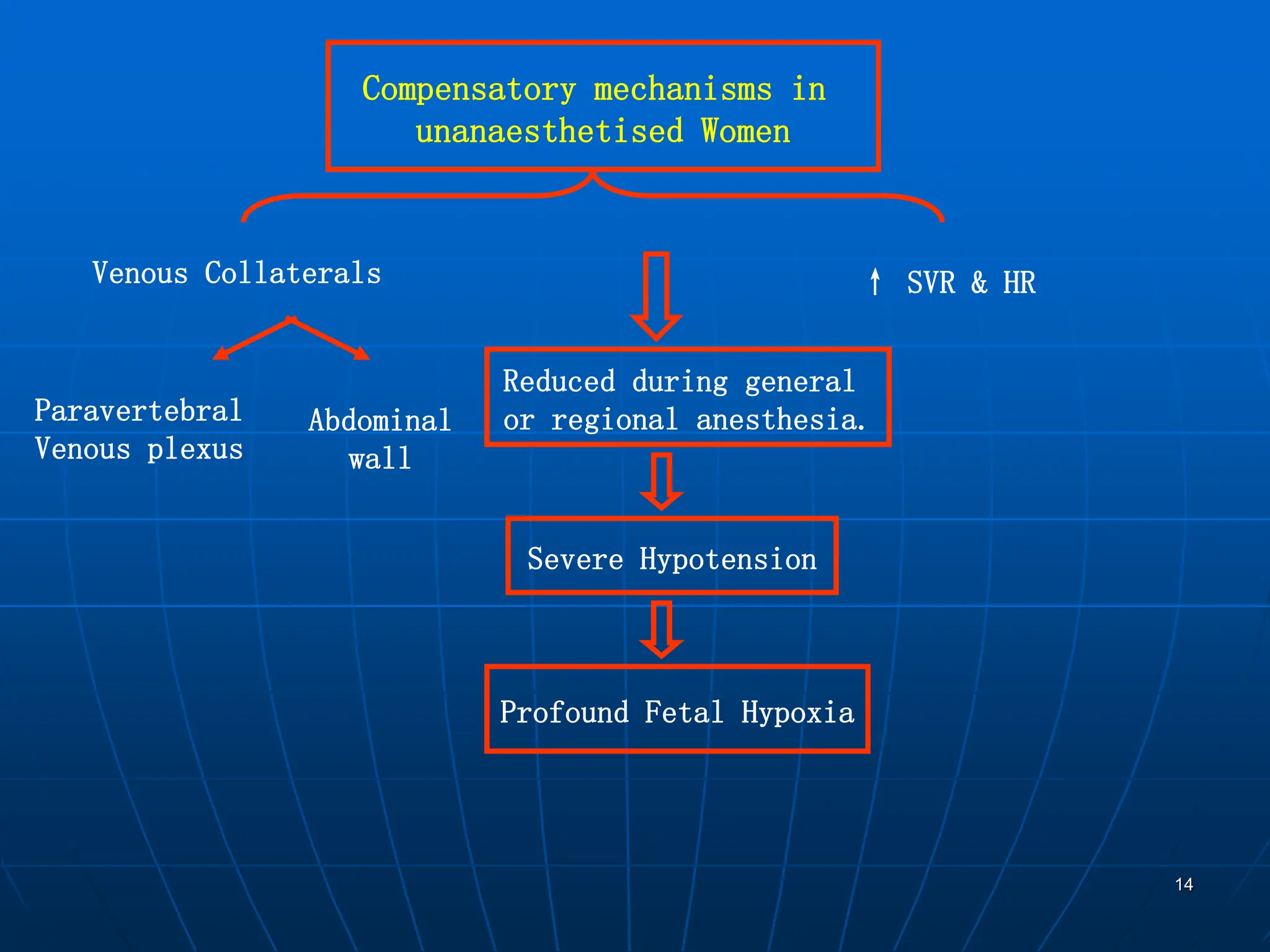
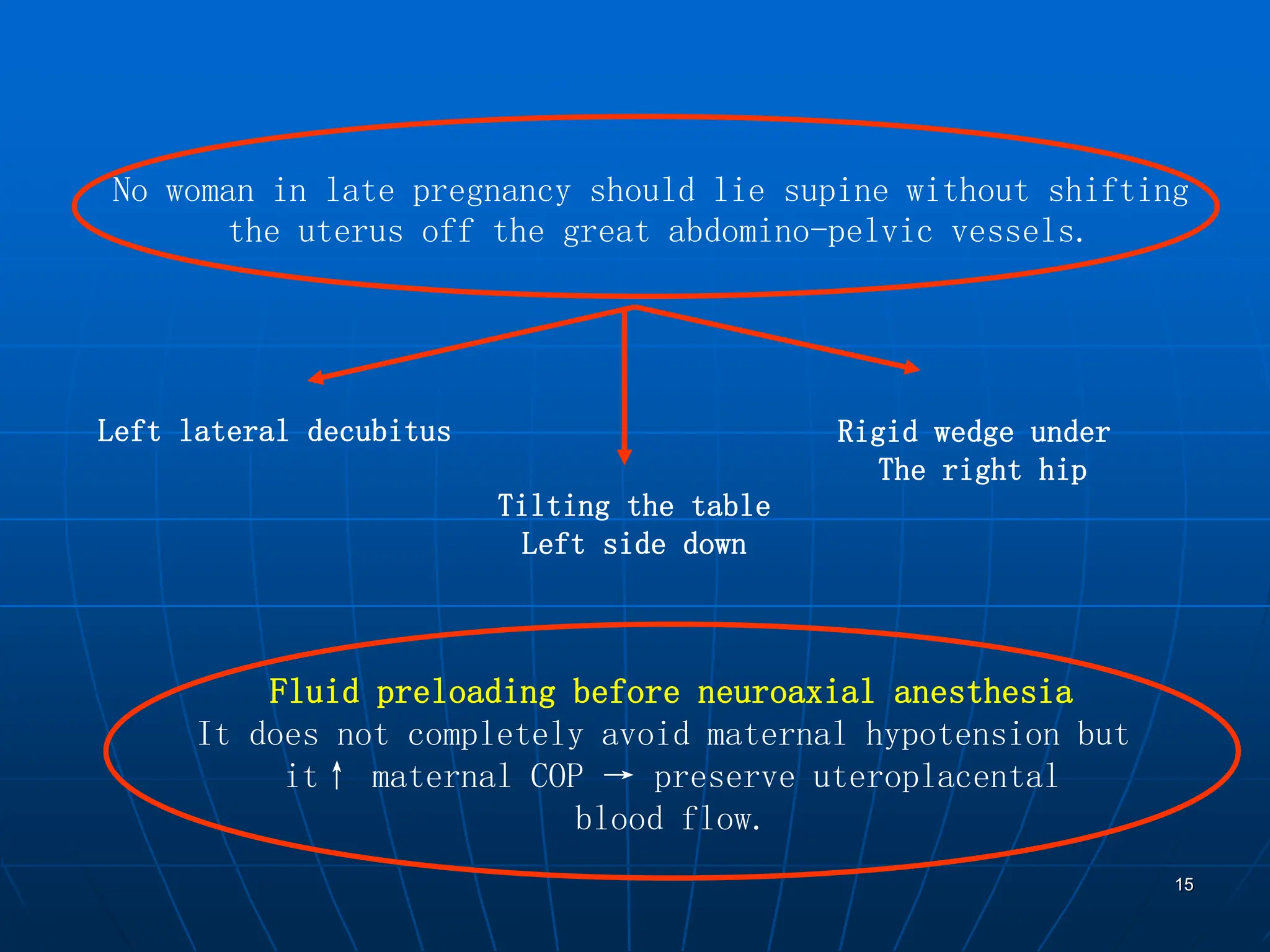
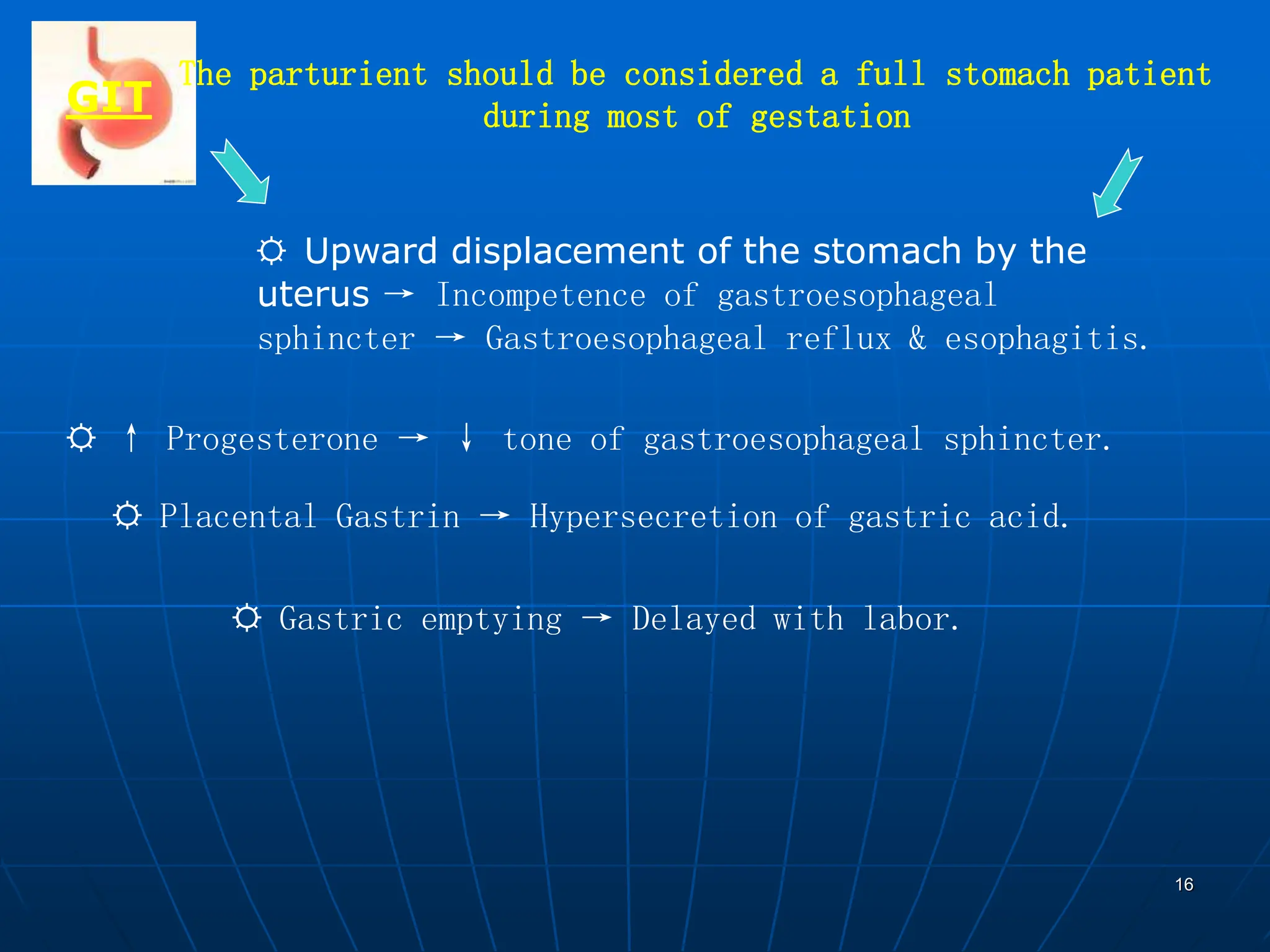
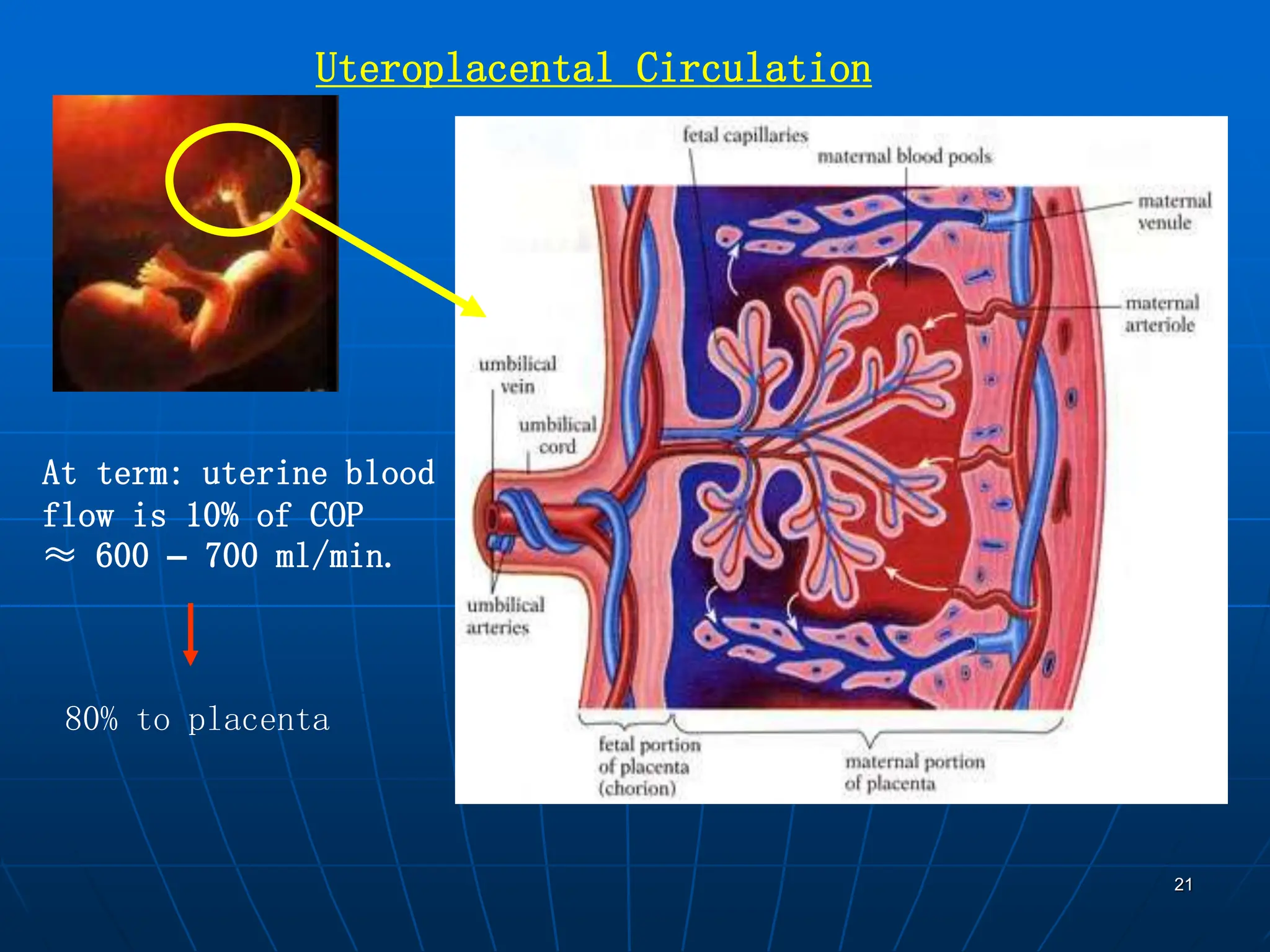
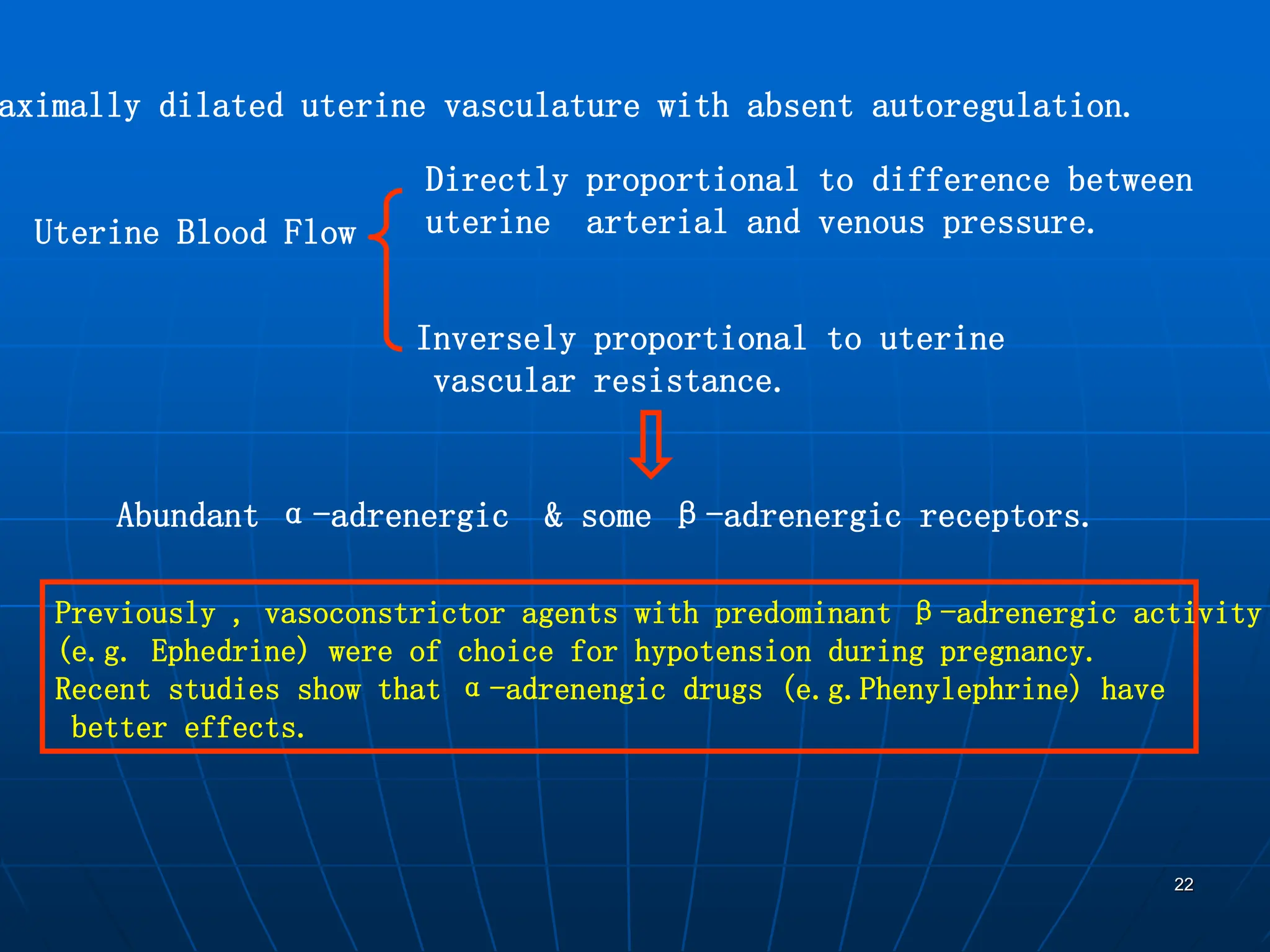
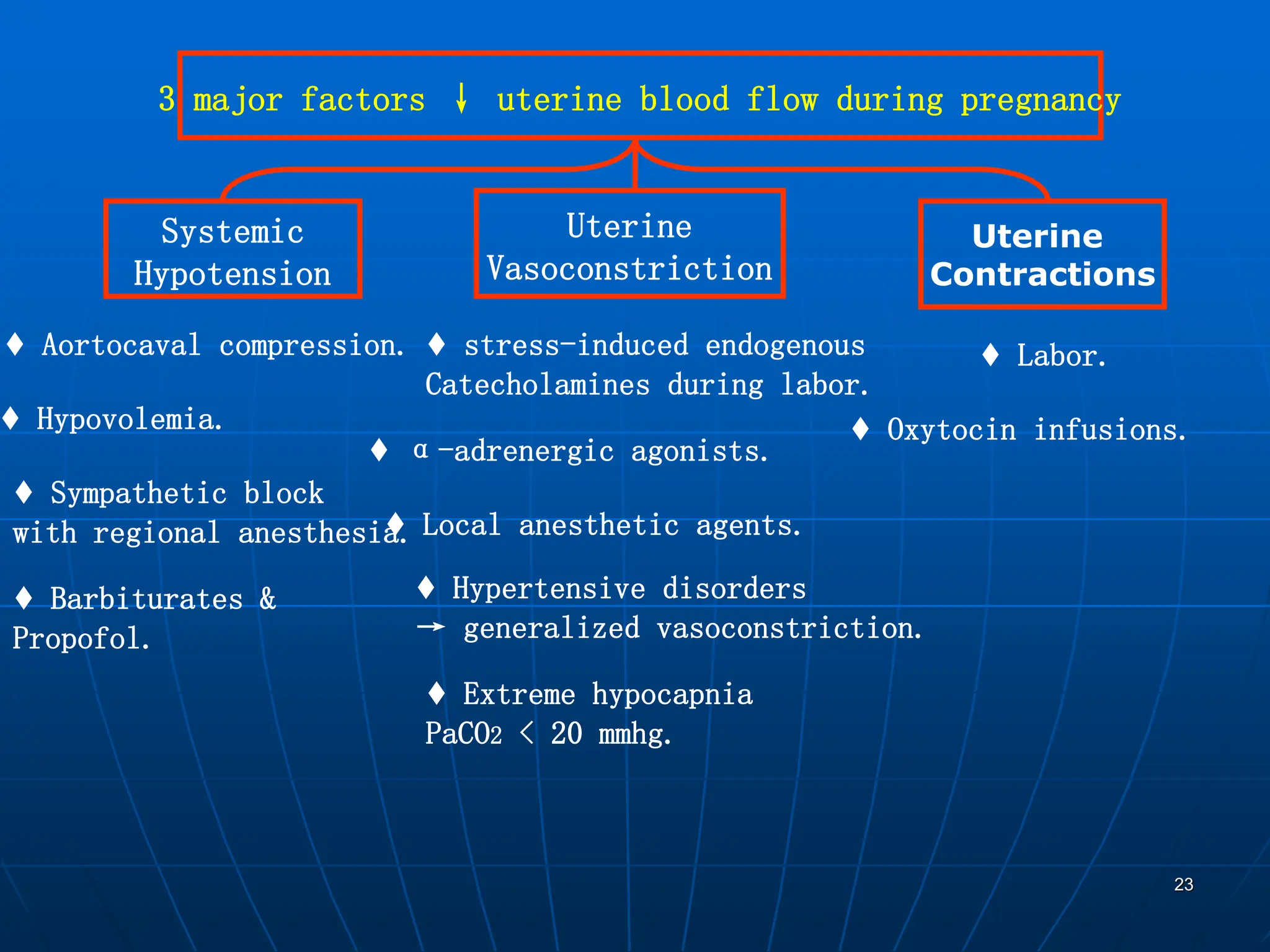
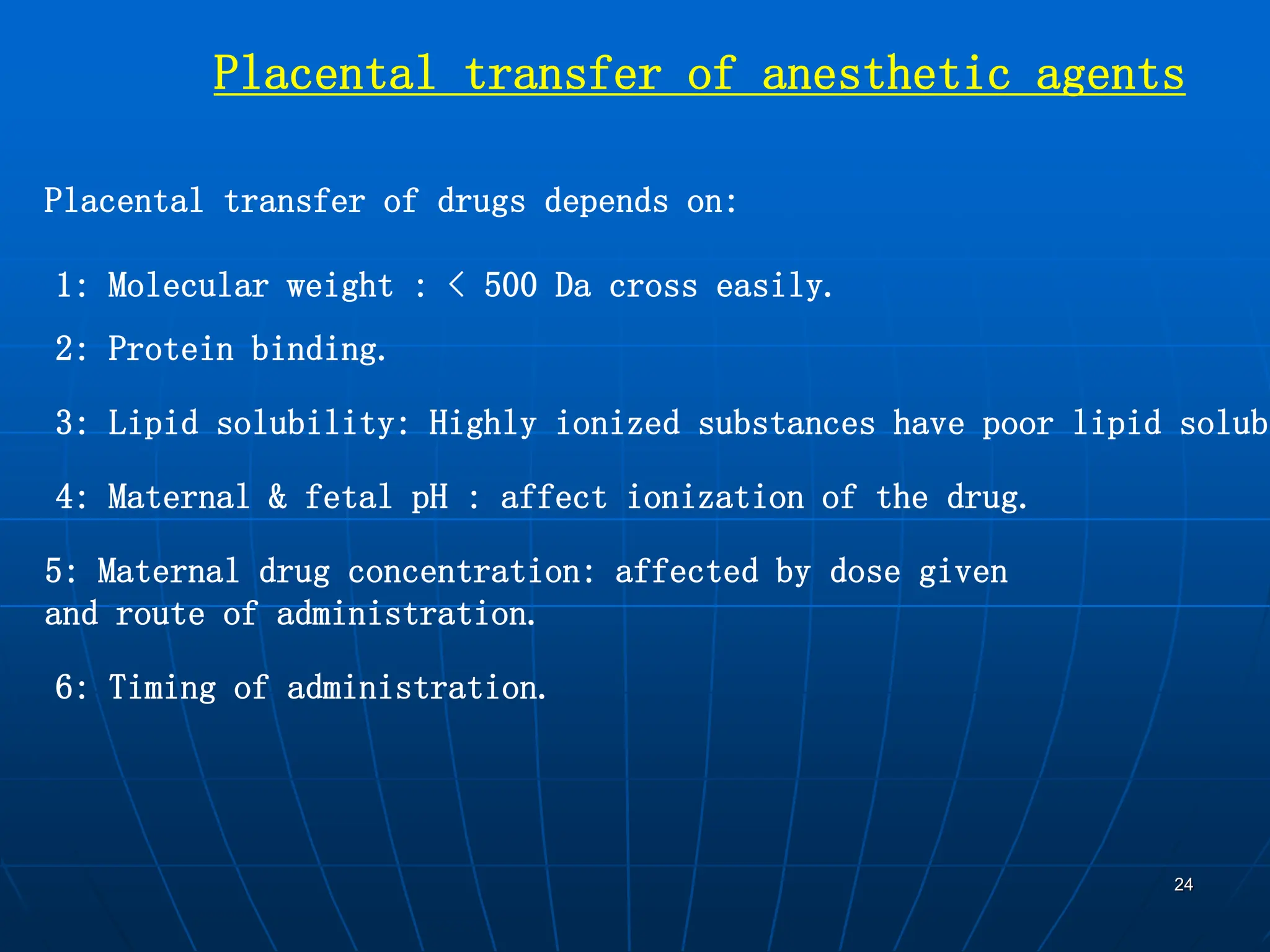
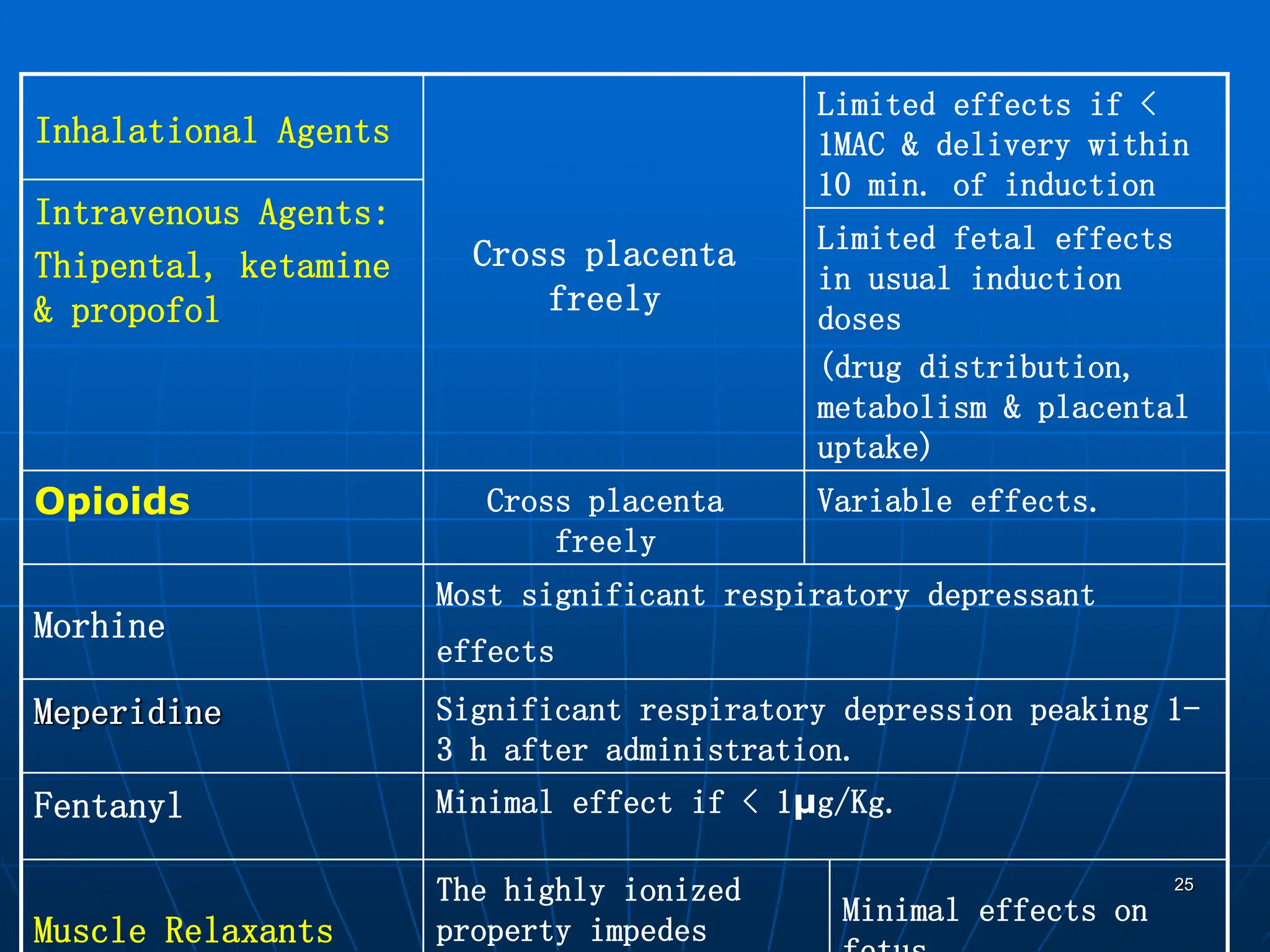
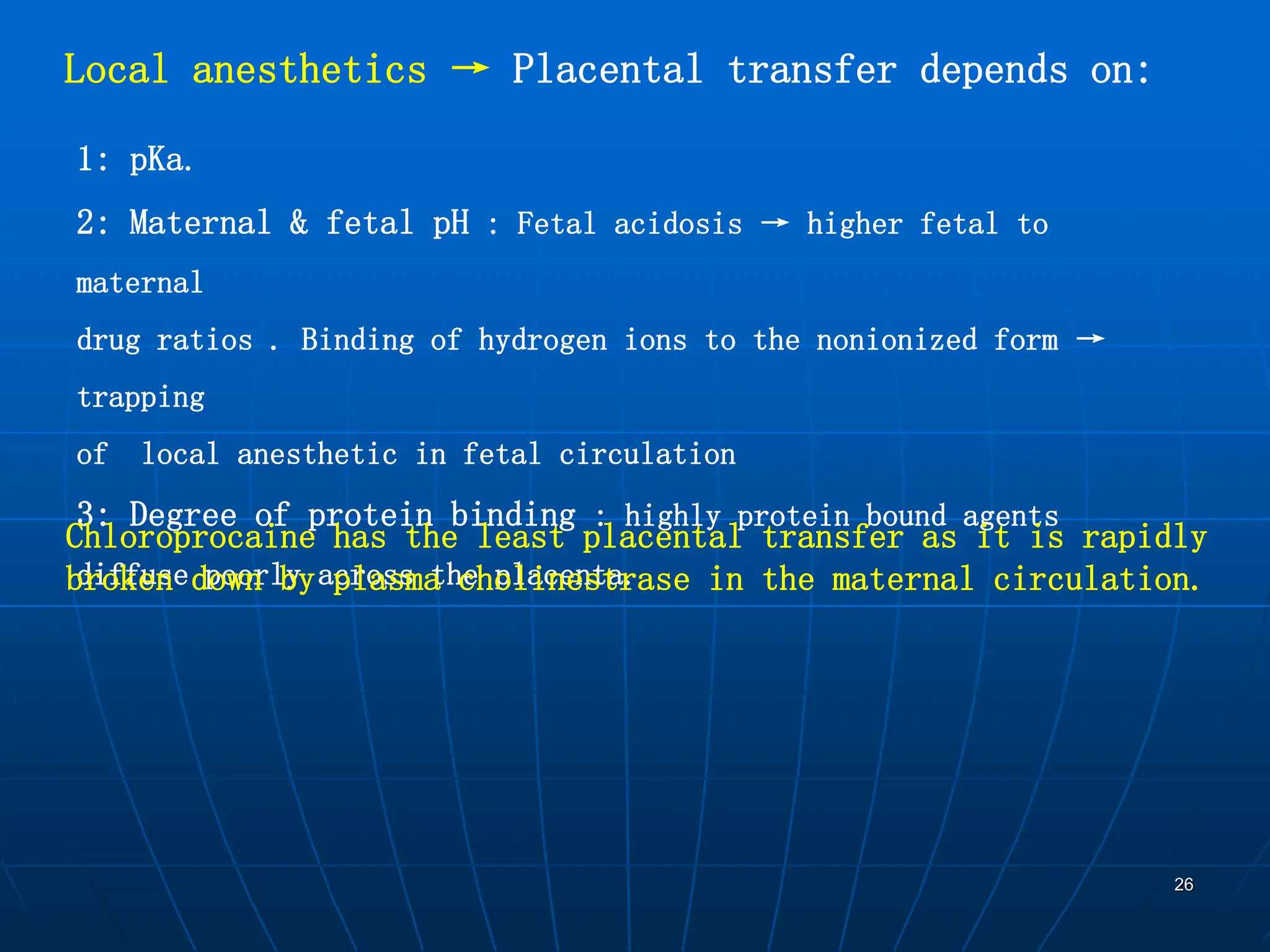
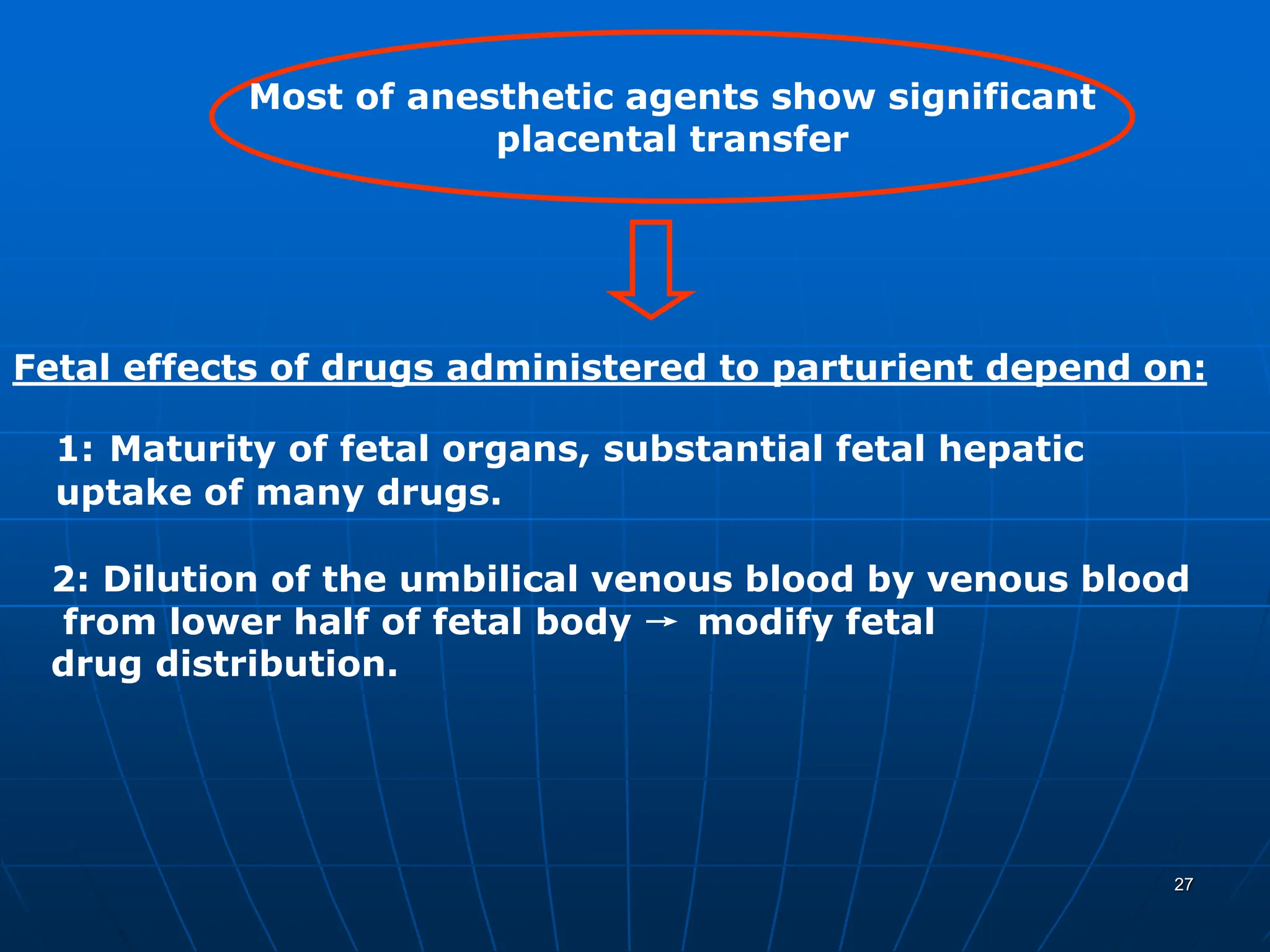
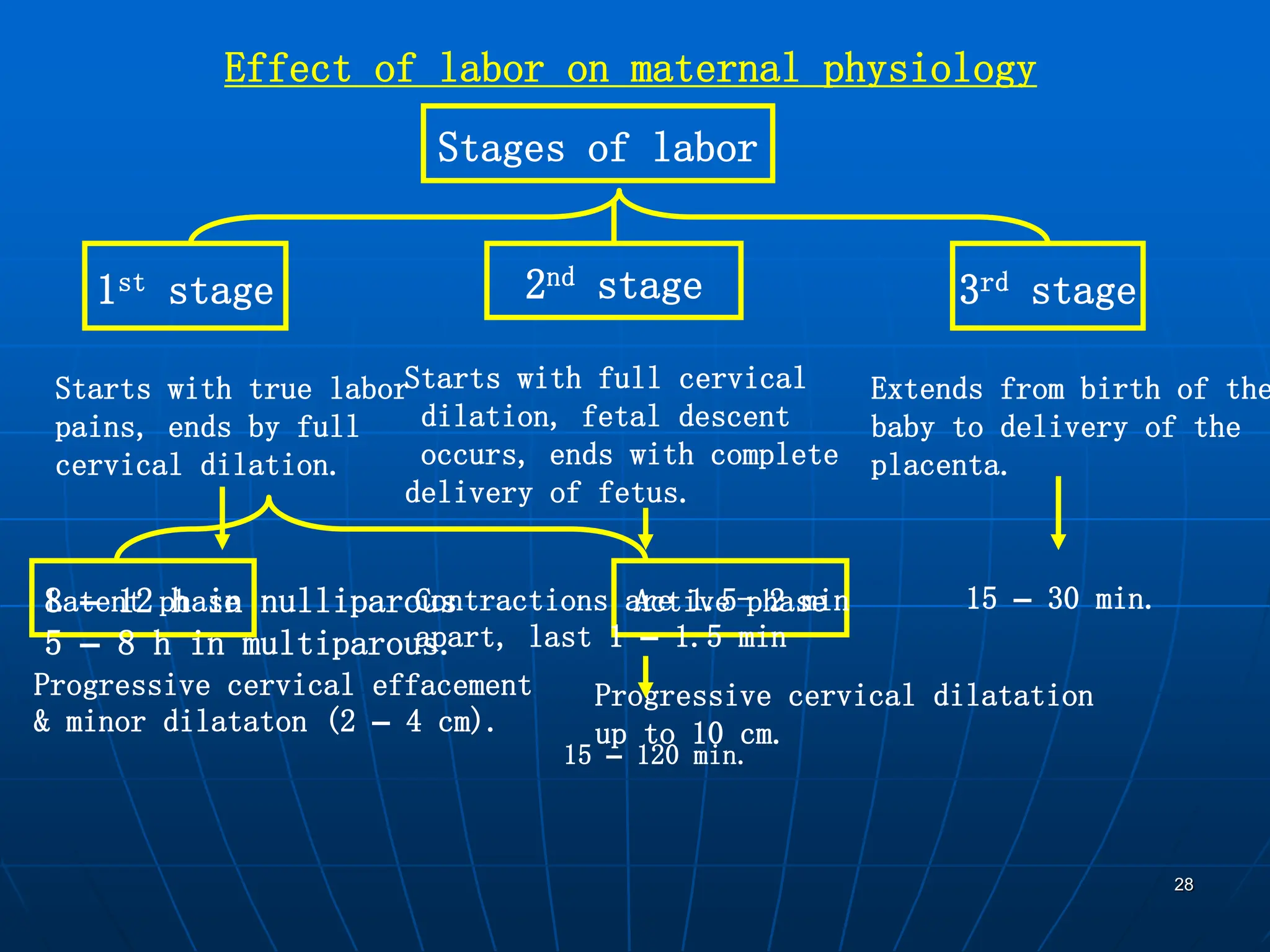
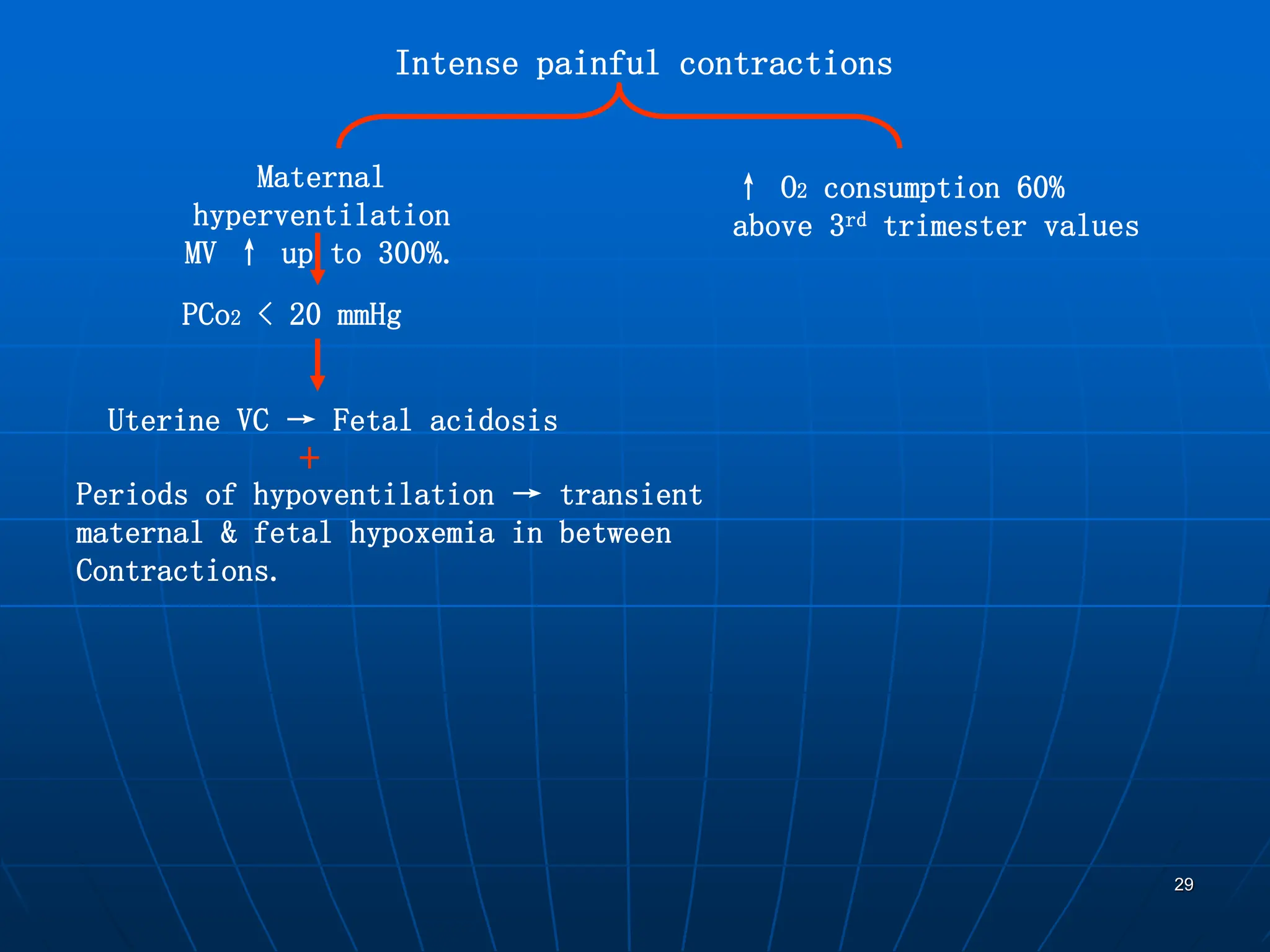
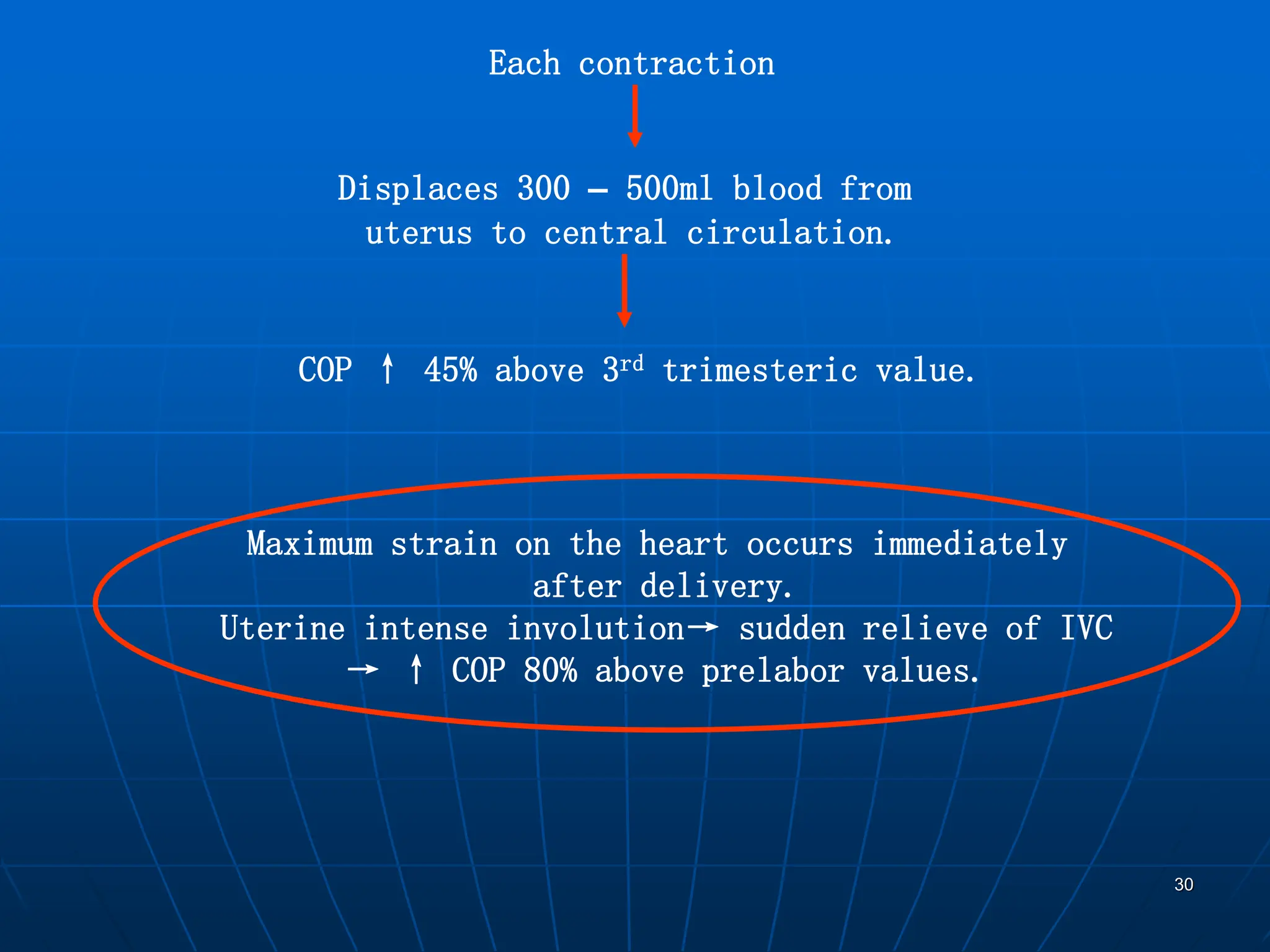
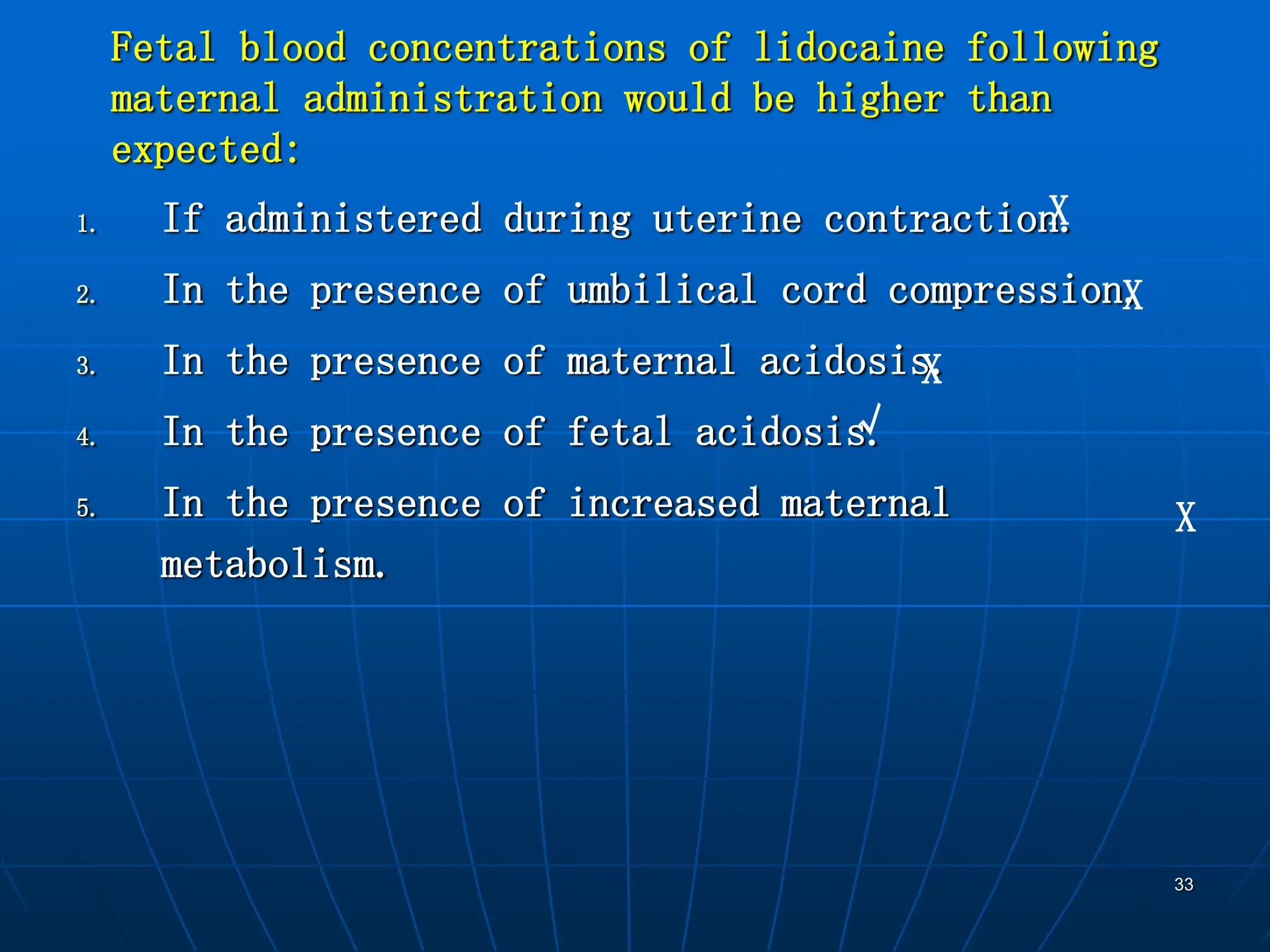
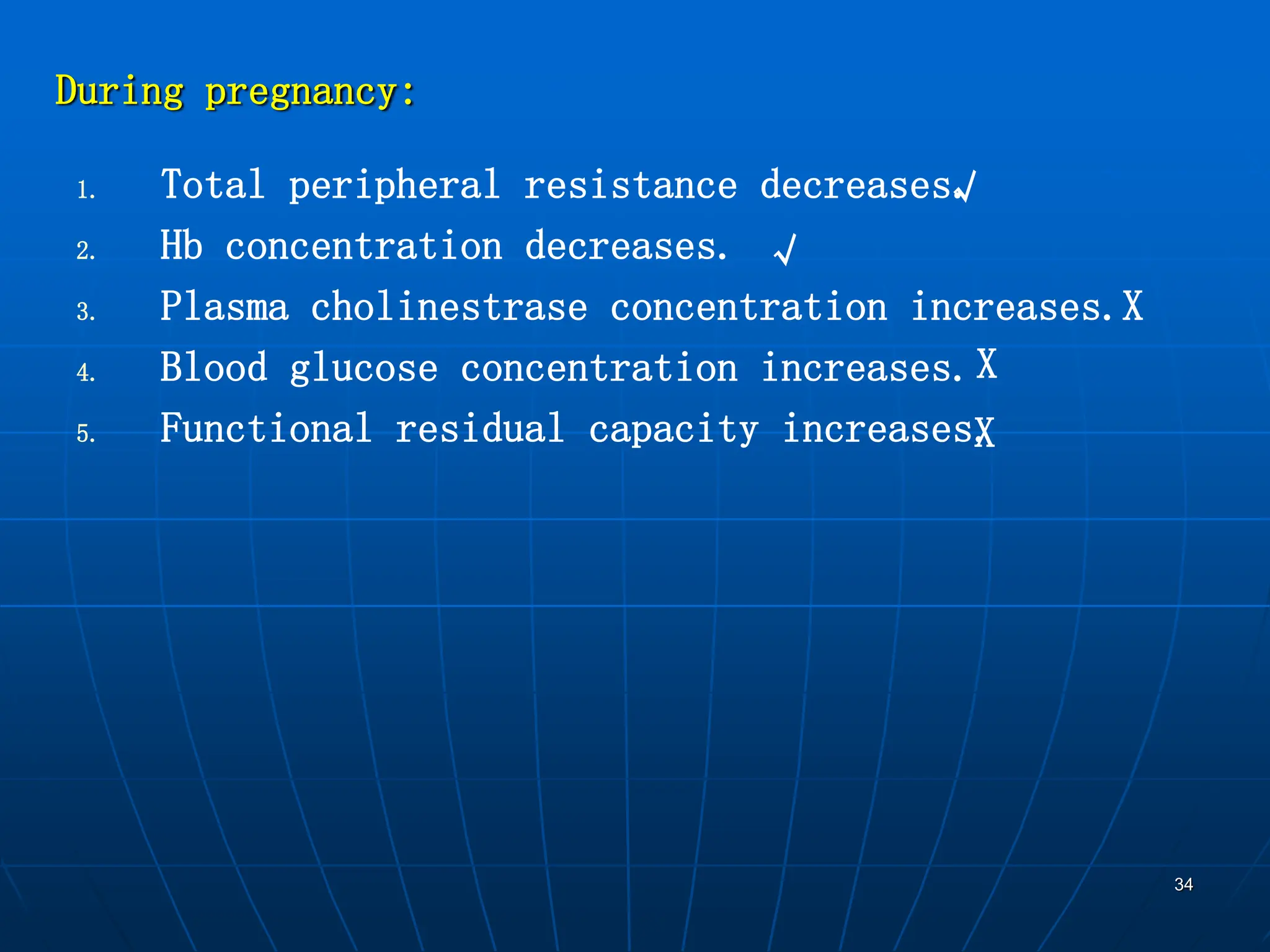
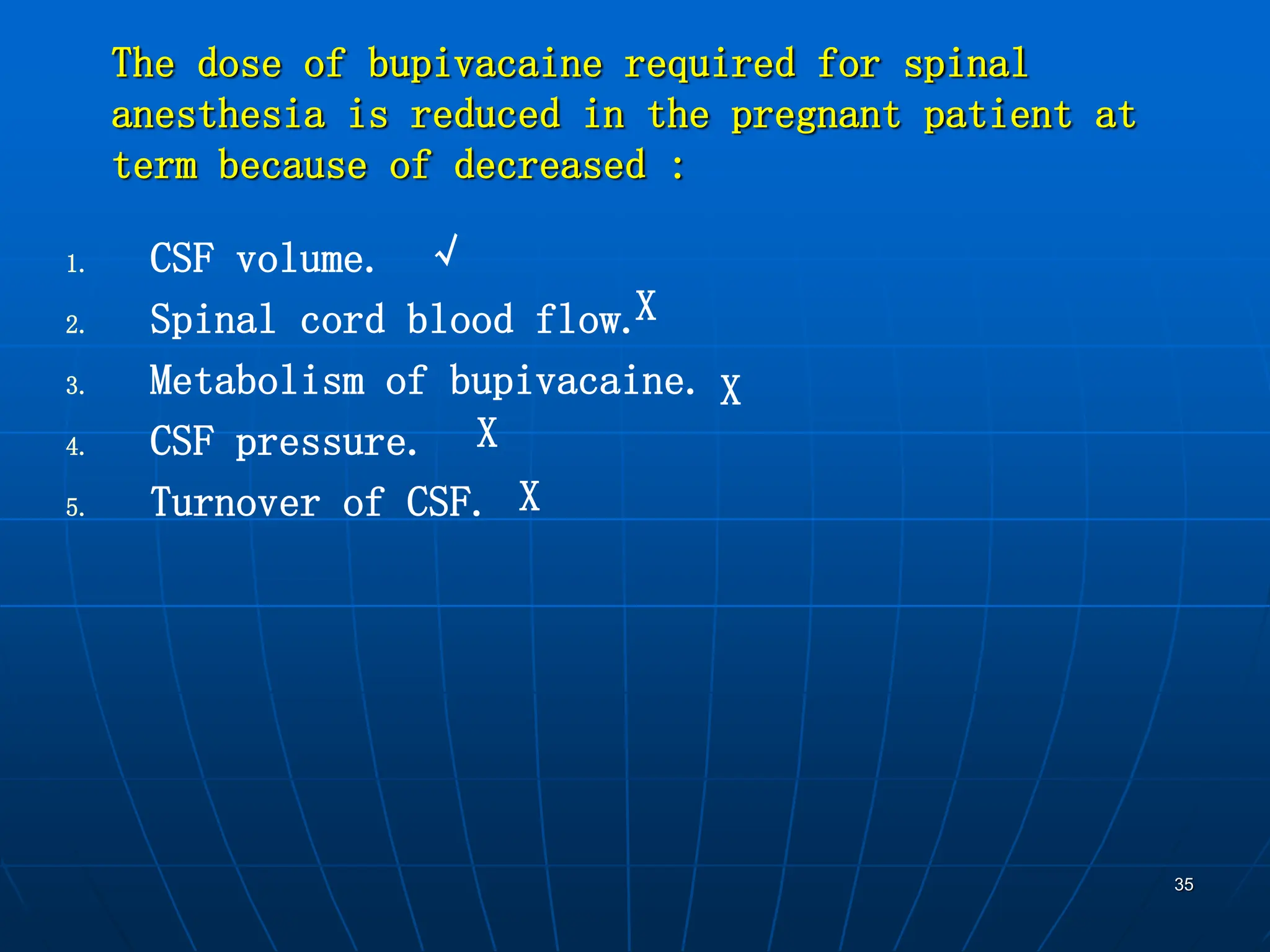
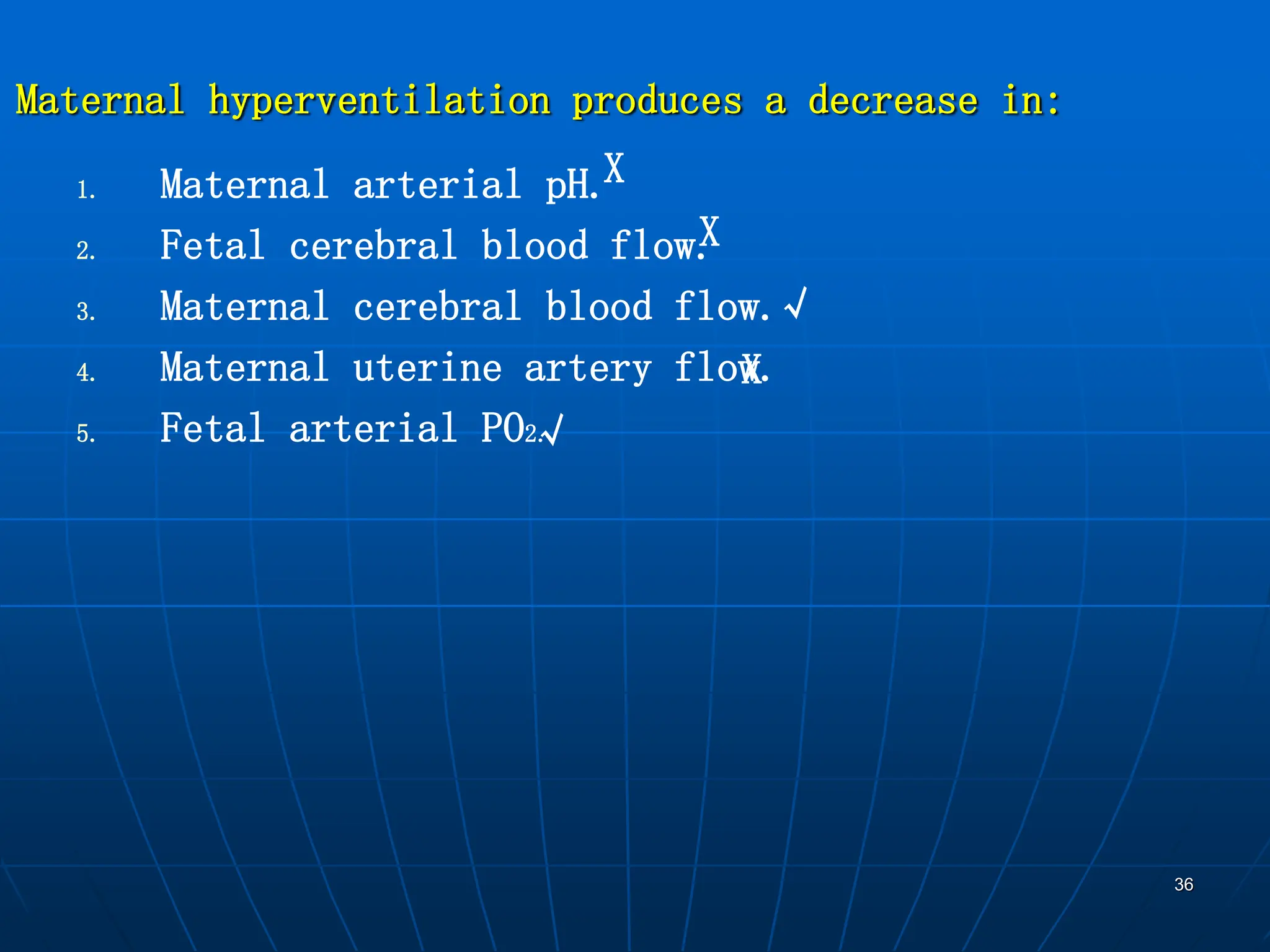
During pregnancy, physiological changes alter the response to anesthesia. The respiratory system adapts to increased oxygen consumption through higher minute ventilation and respiratory drive. Cardiovascular changes include increased blood volume, heart rate, and stroke volume. Supine hypotension can occur due to compression of the inferior vena cava. Anesthetic agents readily cross the placenta and can depress the fetus, so doses must be carefully titrated. Labor further increases oxygen demand and the risk of supine hypotension due to uterine contractions displacing blood from the uterus into central circulation.