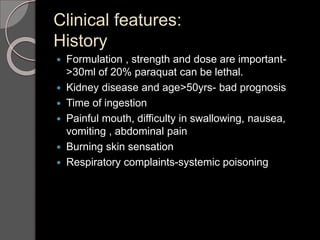
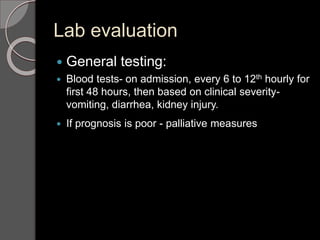
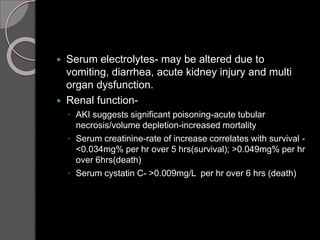
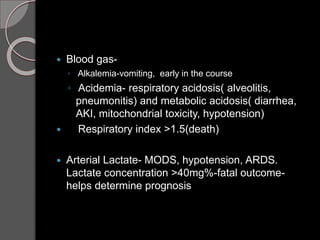
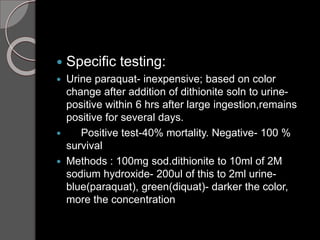
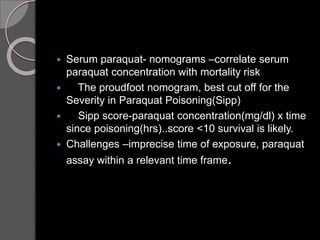
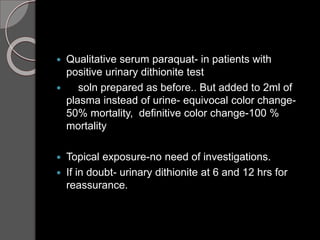
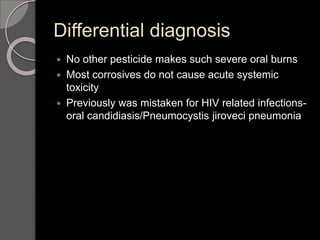
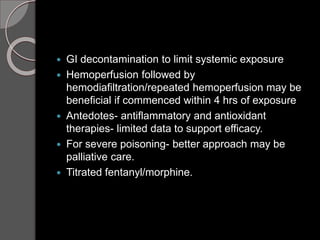
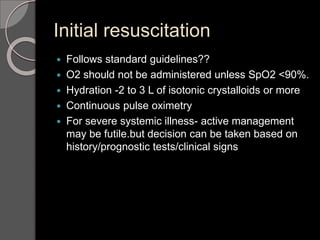
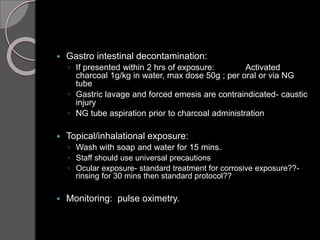
Paraquat poisoning causes severe oxidative stress and multi-organ failure. Ingestion has a high fatality rate. It is rapidly absorbed and concentrated in lungs, liver, and kidneys, causing cellular damage through redox cycling. Clinical features include oropharyngeal burns, respiratory distress, and acute kidney injury. Diagnosis is confirmed by positive urine dithionite test showing blue color change. Prognosis is poor for those with serum paraquat levels above the Sipp score threshold or rapidly increasing creatinine. Early extracorporeal removal within 4 hours may help severe cases, but long-term outcomes are generally poor with progressive lung fibrosis. Management focuses on supportive care, though antioxidants have been tried with