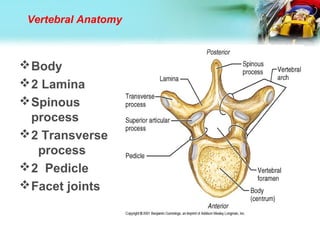
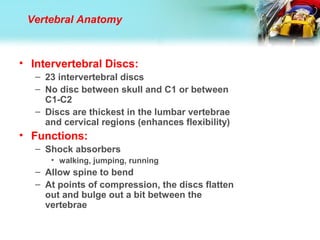
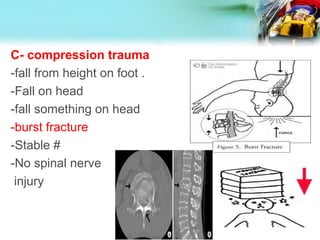
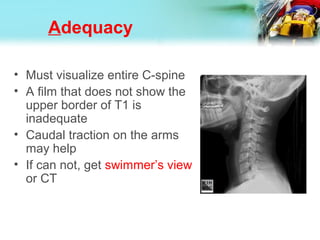
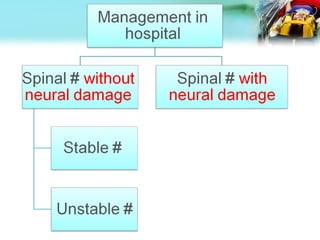
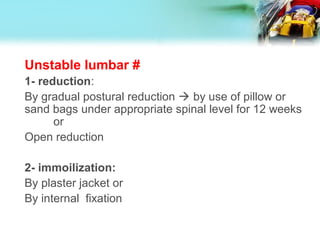
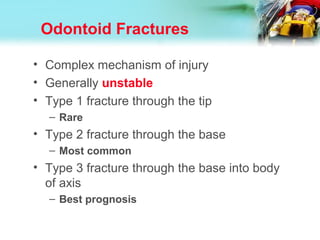
The document discusses the anatomy and clinical features of spinal fractures. It begins with the anatomy of the vertebral column and its supporting ligaments. It then discusses the classification, mechanisms of injury, and clinical features of spinal fractures. Diagnosis involves history, physical exam including neurological exam, and imaging studies like x-rays, CT scans, and MRI to identify fractures and spinal cord injuries. Management aims to prevent secondary injury through immobilization of the spine.