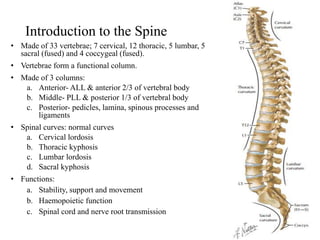
This document provides an overview of spinal disorders, including:
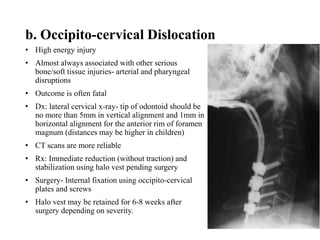
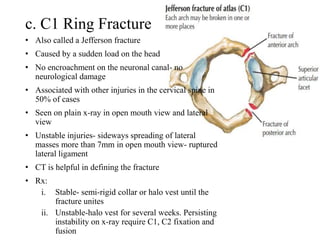
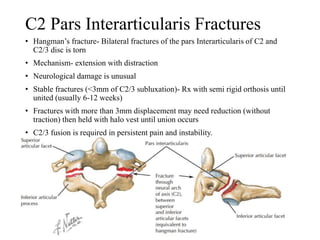
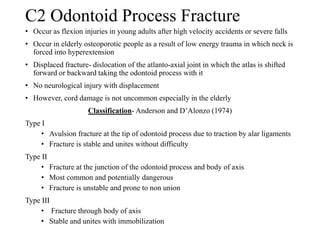
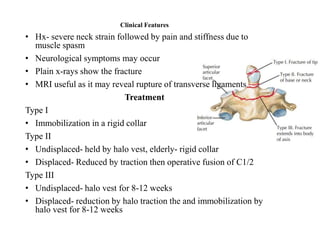
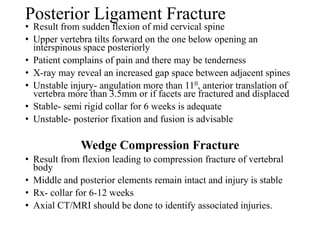
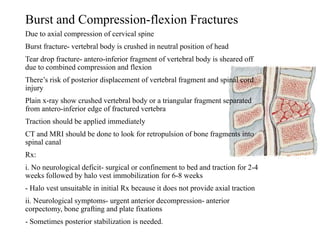
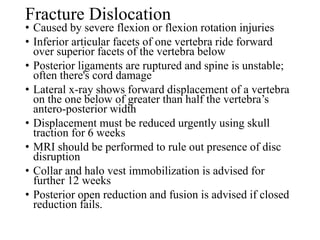
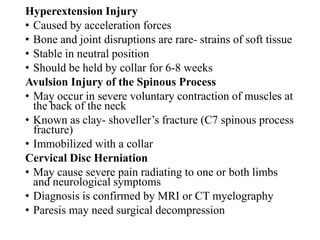
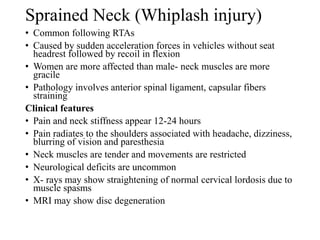
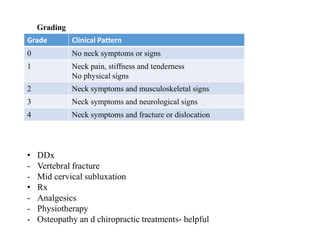
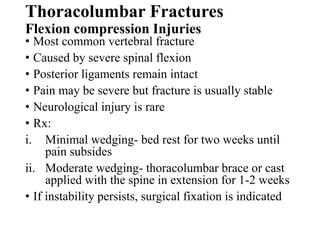
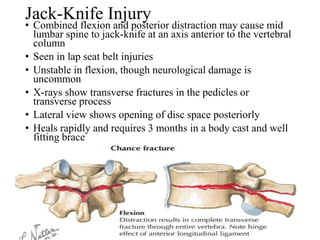
1. Traumatic spinal disorders like fractures of the cervical spine (C1-C2), thoracolumbar fractures from compression or flexion, and cervical disc herniations.
2. Treatment approaches depending on the stability and neurological involvement, ranging from immobilization to surgical fixation or decompression.
3. A classification system for cervical fractures like Anderson and D'Alonzo for odontoid fractures.
4. Details on mechanisms, clinical features, investigations, and management of specific fractures.