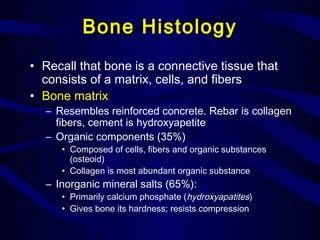
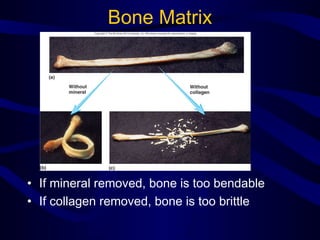
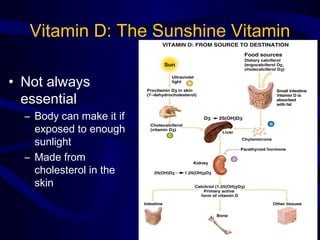
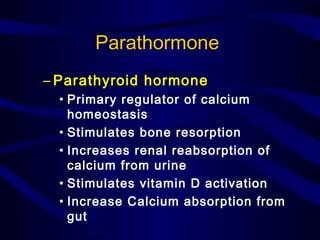
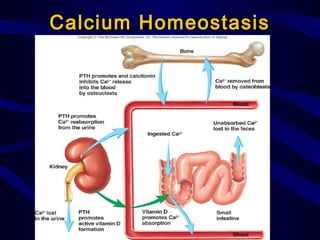
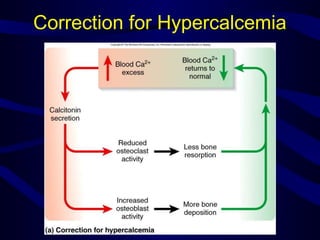
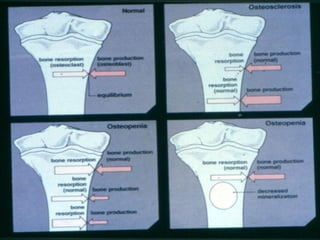
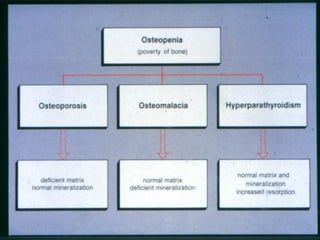
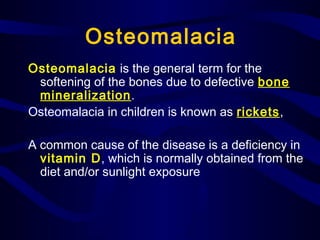
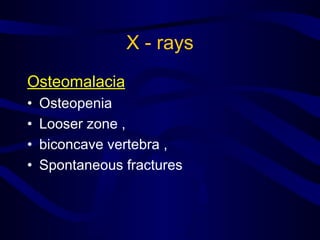
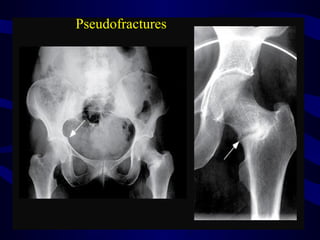
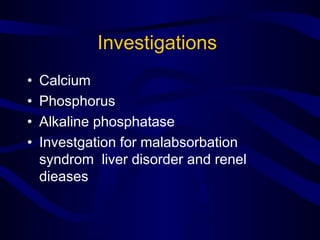
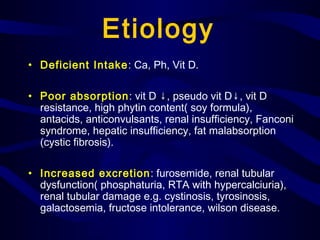
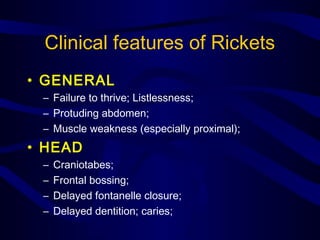
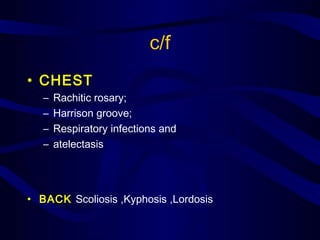
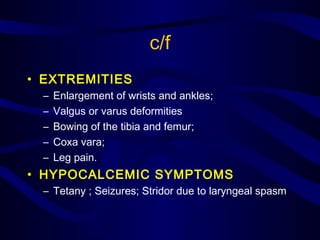
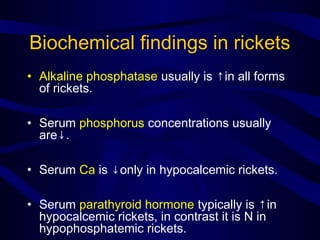
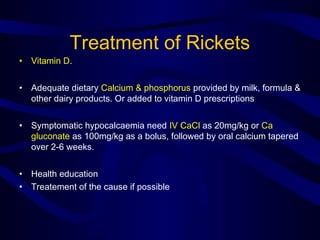
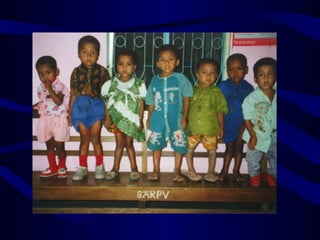
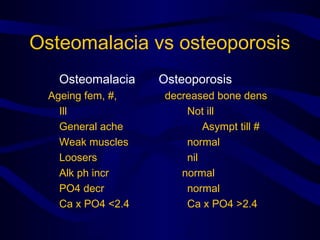
This document discusses metabolic bone diseases including osteomalacia and rickets. It provides details on bone histology, calcium homeostasis, vitamin D metabolism, and the roles of parathyroid hormone and calcitonin in regulating calcium levels. It describes the causes, clinical features, investigations and treatments of osteomalacia and rickets. Osteomalacia is characterized by softening of bones from defective mineralization in adults, while rickets causes softening of bones and growth plate abnormalities in children, often due to vitamin D or calcium deficiencies.