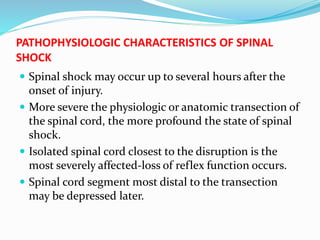
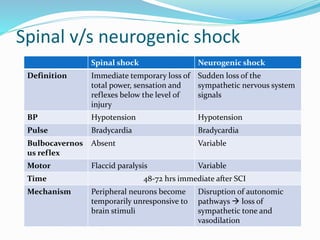
1. Spinal shock is a temporary loss of spinal reflex activity below the level of spinal cord injury that occurs immediately after severe spinal cord injury.
2. It is demonstrated by a loss of muscle tone, reflexes, and sensation below the level of injury and can last from hours to weeks depending on the severity and level of injury.
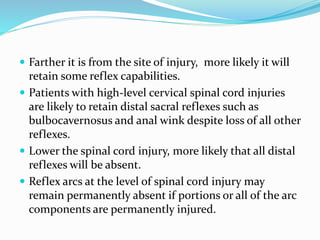
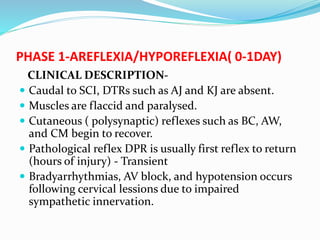
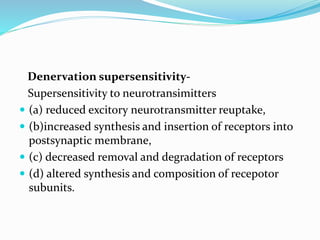
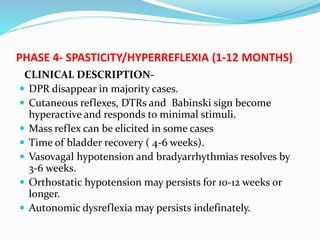
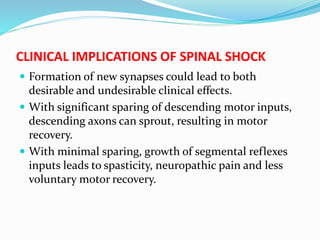
3. Spinal shock results from the loss of descending facilitation from the brain to the spinal cord below the level of injury and goes through phases of areflexia, initial reflex return, hyperreflexia, and eventually spasticity as the spinal cord recovers over time.