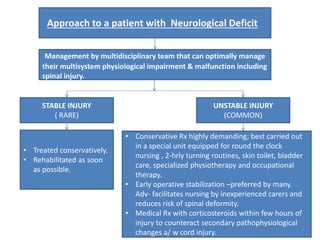
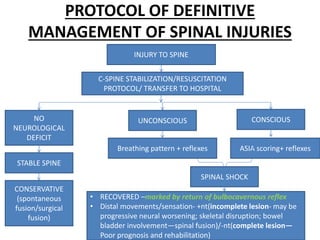
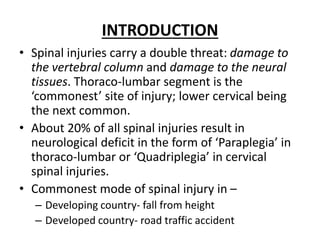
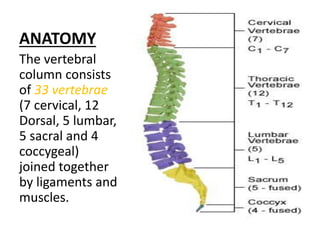
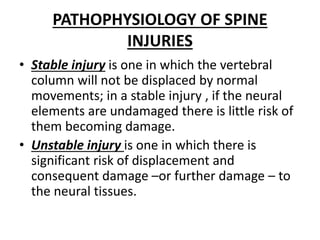
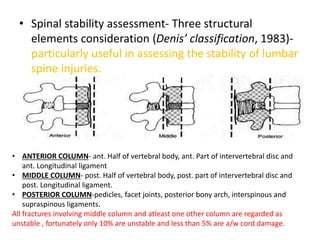
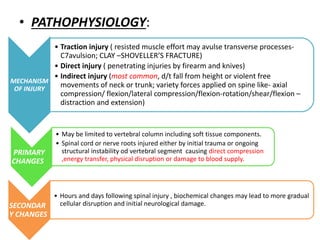
Spinal injuries, predominantly in the thoraco-lumbar and lower cervical regions, pose serious threats to both the vertebral column and neural tissues, leading to potential neurological deficits like paraplegia and quadriplegia. These injuries can stem from various mechanisms such as falls, road traffic accidents, or direct trauma, and can be classified into stable and unstable categories based on the risk of further damage to spinal stability. Management encompasses early resuscitation, immobilization, assessment of neurological status, and a multidisciplinary approach to treatment, which may include surgical intervention and rehabilitation to preserve function and enhance recovery.

![• The patient should be moved without flexion or
rotation of the thoracolumbar spine. A scoop
stretcher and spinal board are very useful for this.
• Logrolling technique used for:
– Placing patient on spinal board.
– Examining the back of patient.
• Medical therapy:
– Early treatment with high doses of corticosteroids
( methylprednisolone, 30 mg/kg , i.v. ; followed by
maintenance dose of 5.4 mg/kg/hr for 23 hours) may
improve neurological recovery if commenced within 8
hours following the injury; albeit the evidence is limited
and some neurosurgical guidelines do not recommend
their use. [Source- CMDT-2017]](https://image.slidesharecdn.com/spinalinjuries-180518121456/85/Spinal-injuries-20-320.jpg)