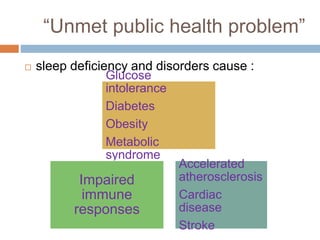
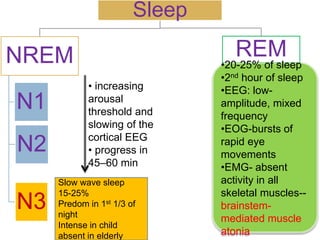
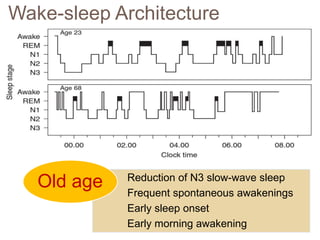
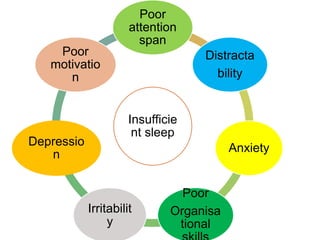
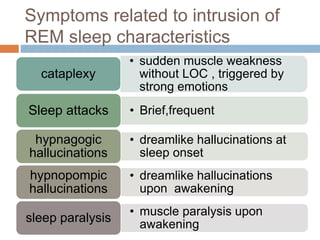
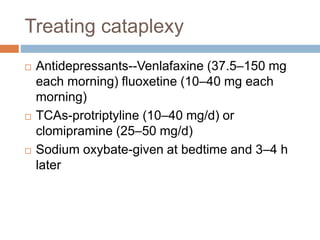
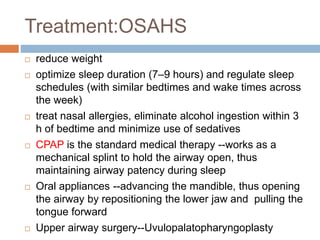
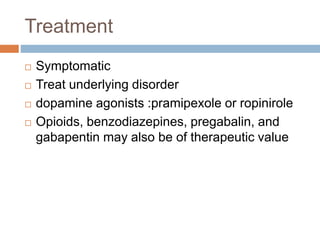
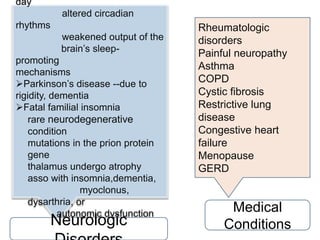
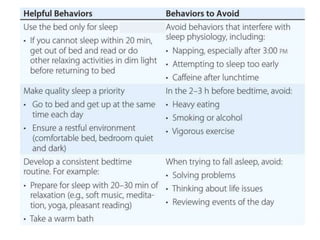
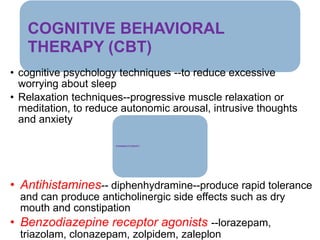
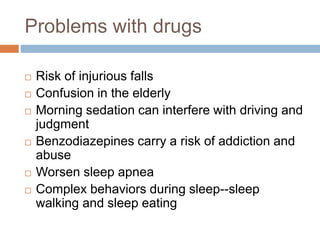
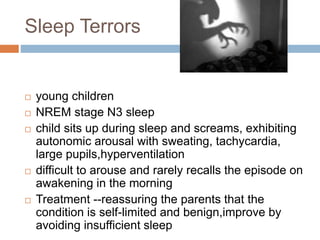
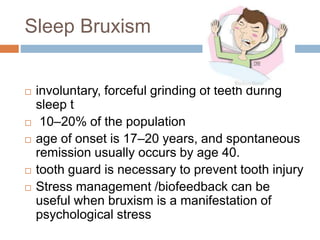
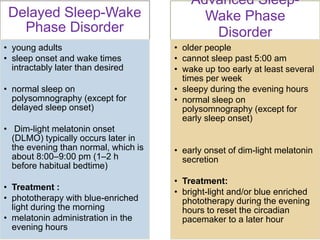
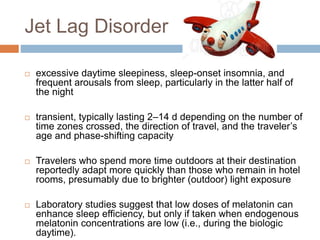
This document discusses various sleep disorders and approaches to evaluating and treating patients with sleep problems. It covers topics like insomnia, obstructive sleep apnea, narcolepsy, restless leg syndrome, circadian rhythm disorders, and parasomnias. The key points are obtaining a thorough patient history, performing tests like polysomnography and multiple sleep latency tests to diagnose the underlying cause, and treating the specific disorder through lifestyle changes, medications, CPAP, or other therapies.