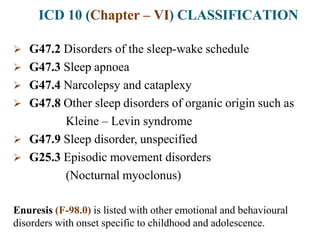
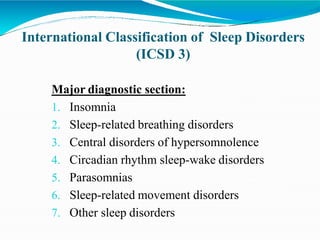
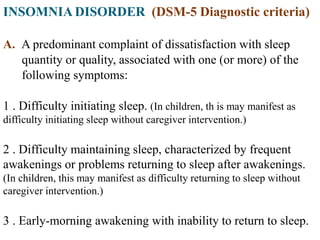
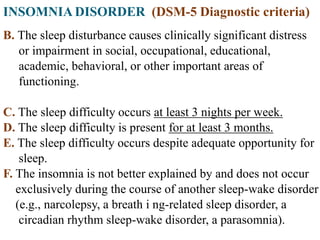
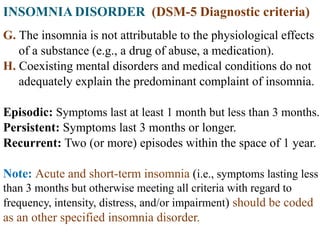
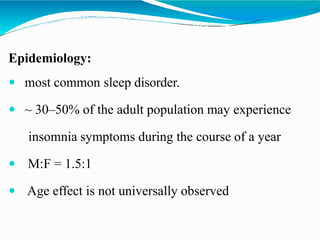
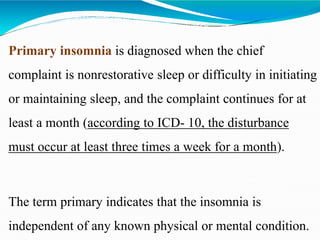
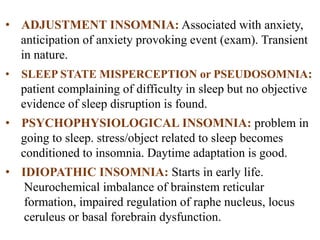
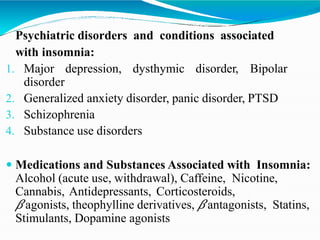
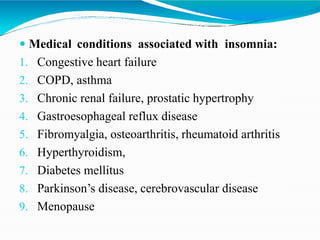
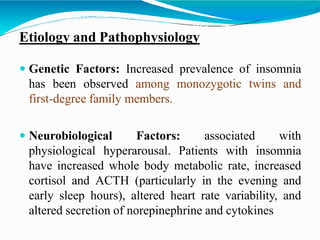
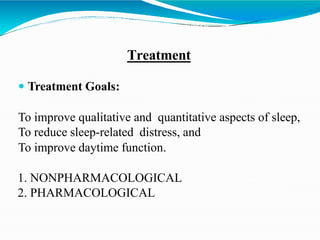
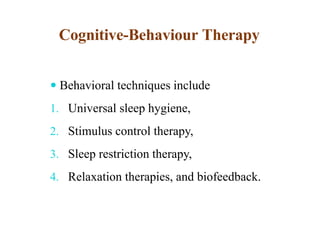
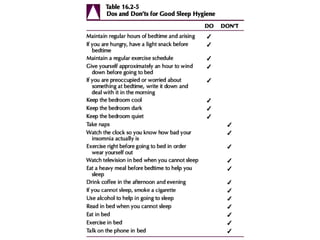
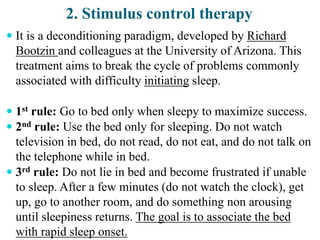
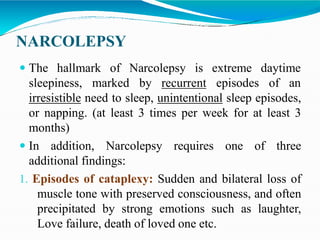
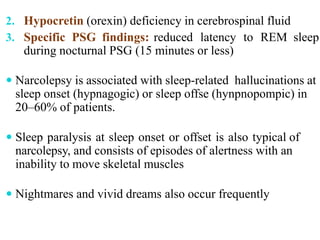
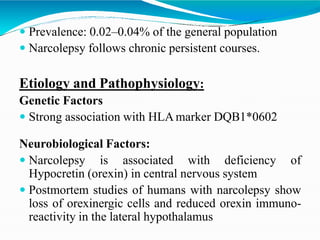
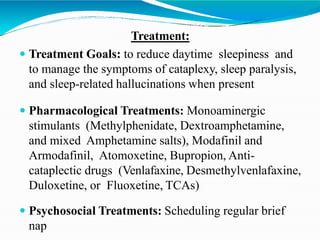
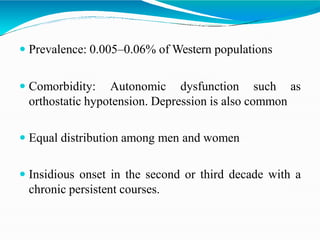
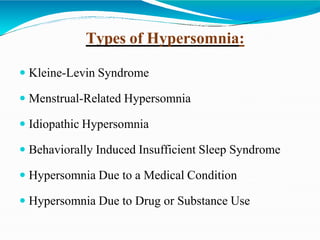
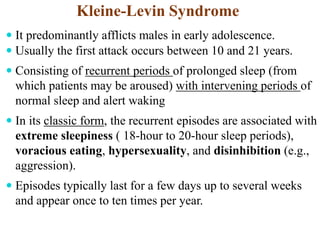
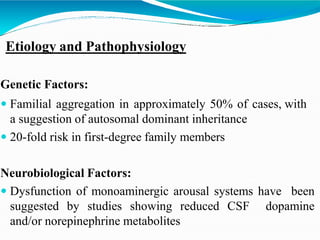
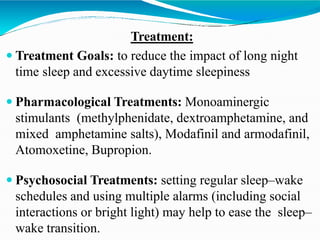
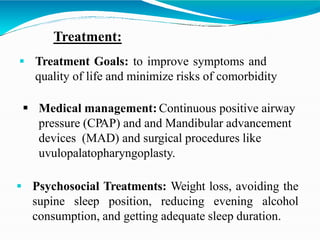
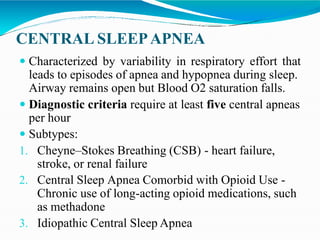
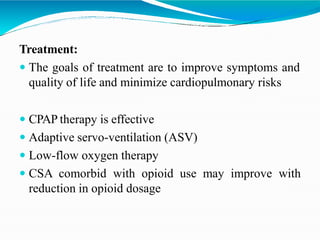
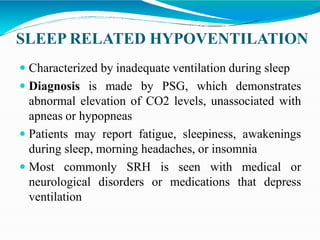
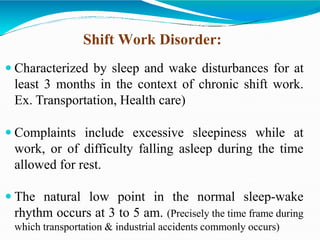
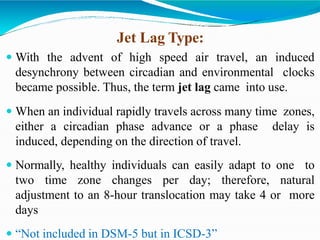
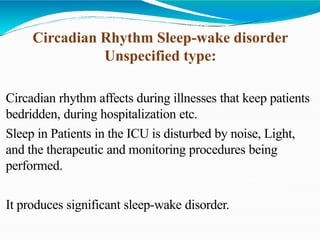
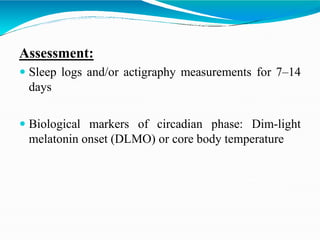
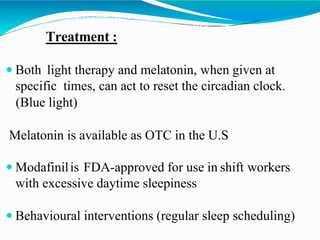
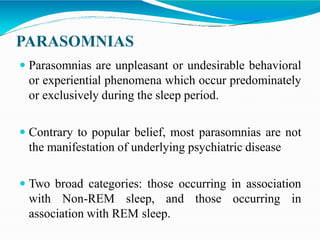
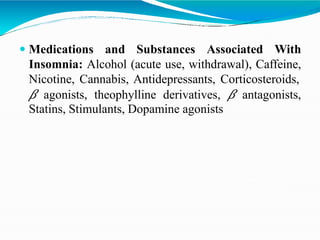
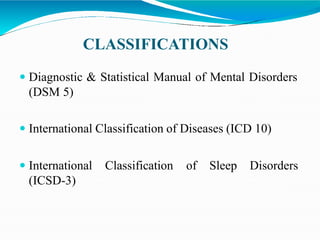
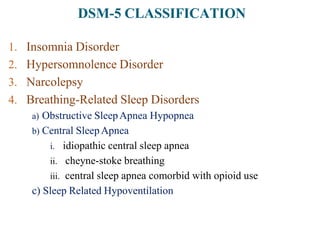
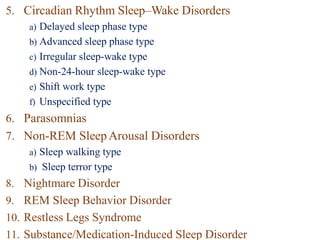
This document discusses classifications and types of sleep disorders according to diagnostic manuals like DSM-5 and ICD-10. It covers disorders like insomnia, hypersomnolence disorder, narcolepsy, breathing-related sleep disorders including obstructive sleep apnea, and circadian rhythm sleep-wake disorders. For each type of sleep disorder, it provides diagnostic criteria, epidemiology, etiology and pathophysiology, treatment approaches and specific subtypes or related conditions. The document aims to comprehensively describe the major sleep disorders recognized in clinical practice and research according to standardized diagnostic systems.
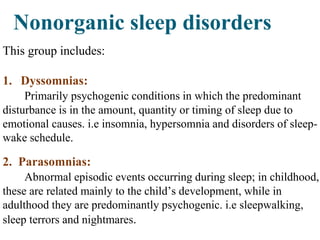
![ICD 10 (Chapter – V) CLASSIFICATION
F-51 Nonorganic Sleep disorders
F 51.0 Nonorganic insomina
F 51.1 Nonorganic hypersomina
F 51.2 Nonorganic Disorders of the sleep-wake
schedule
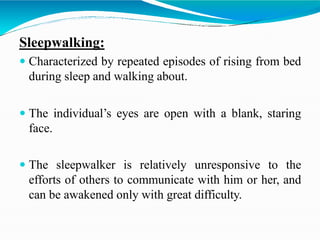
F 51.3 Sleep walking [somnambulism]
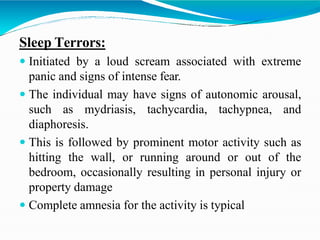
F 51.4 Sleep terrors [night terrors]
F 51.5 Nightmares
F 51.8 Other Nonorganic sleep disorders
F 51.9 Nonorganic Sleep disorder, unspecified
Includes: emotional sleep disorder NOS](https://image.slidesharecdn.com/sleepdisordersbydr-210317085636/85/Sleep-disorders-by-dr-rujul-modi-6-320.jpg)