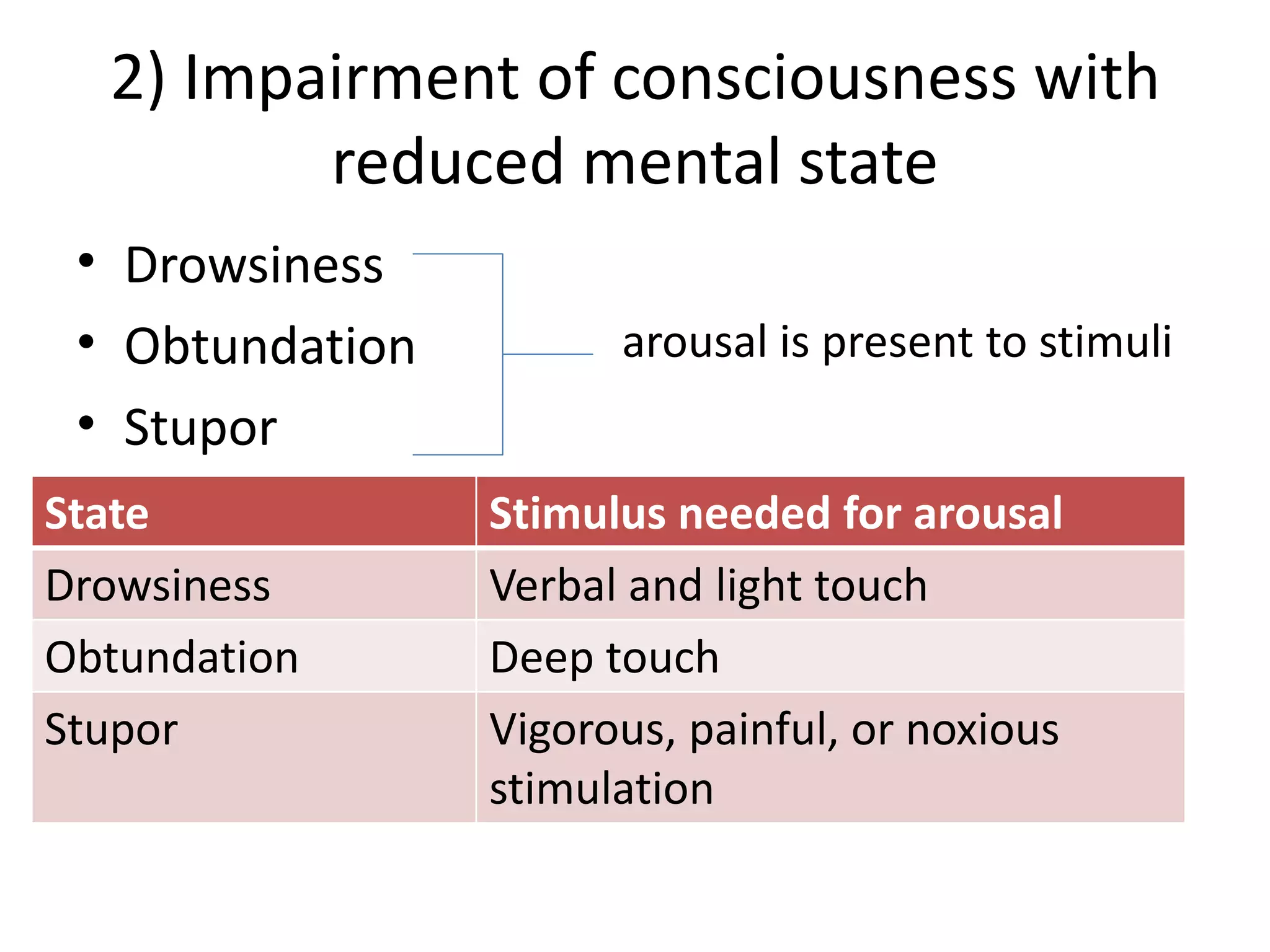
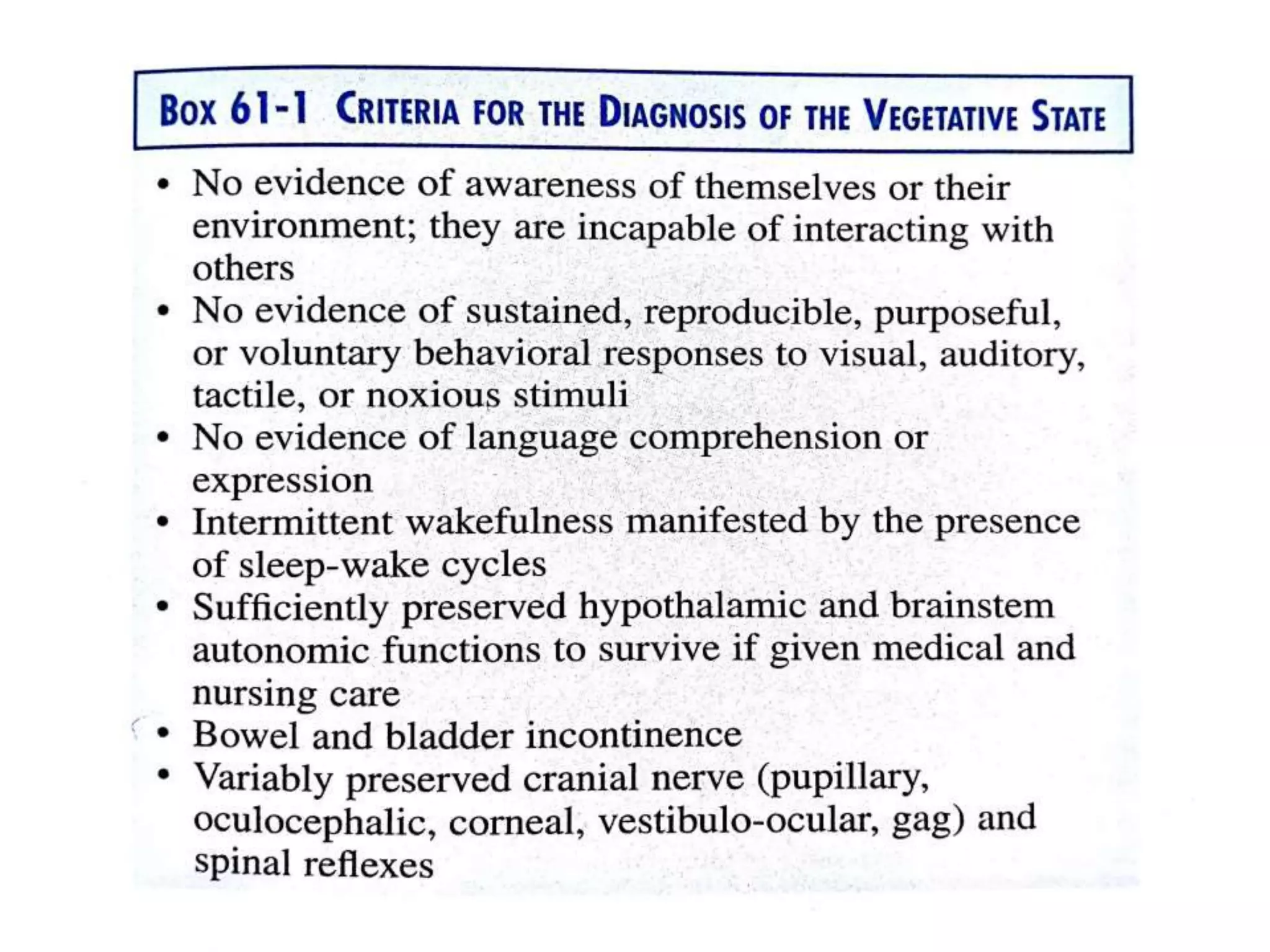
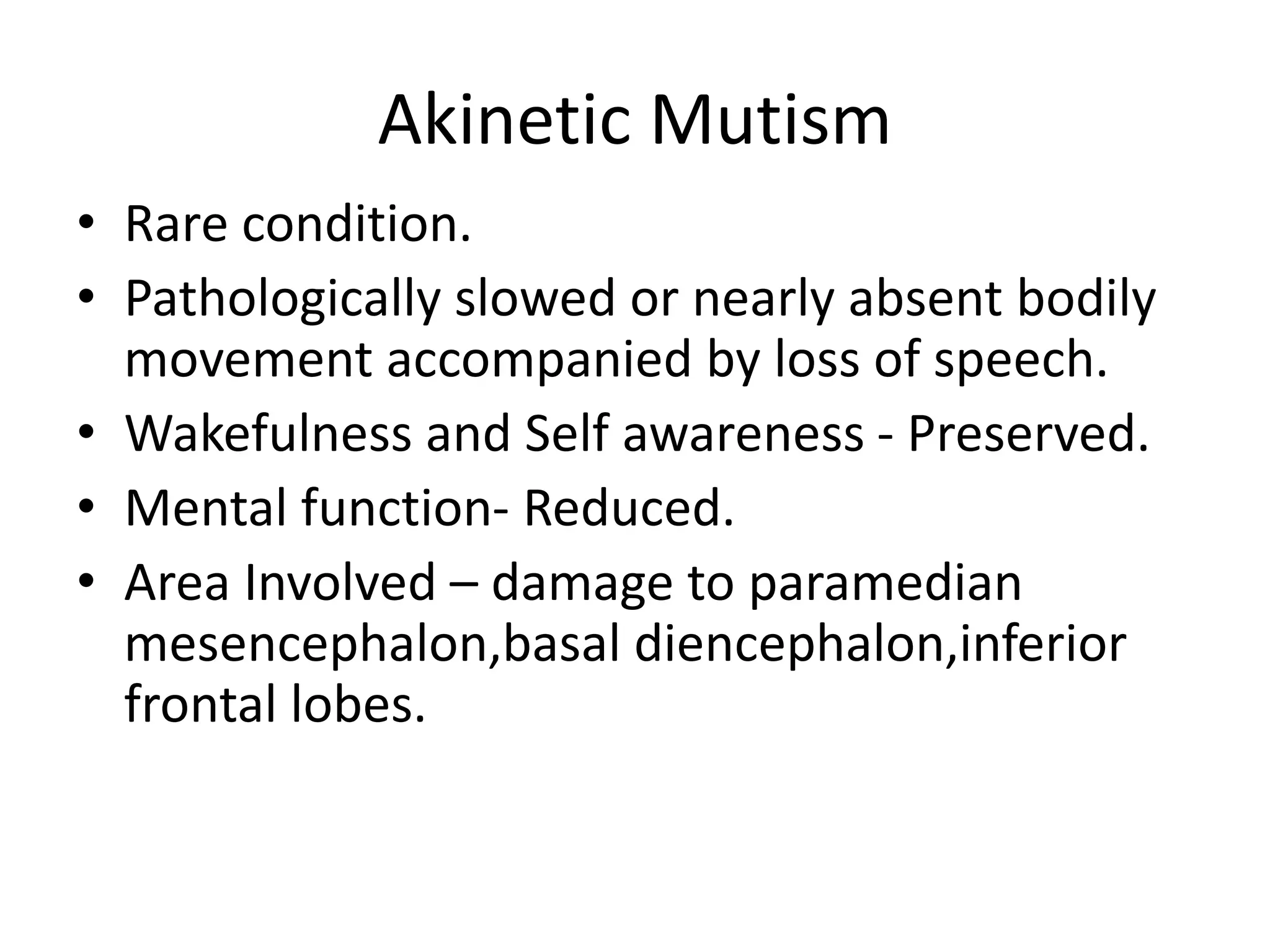
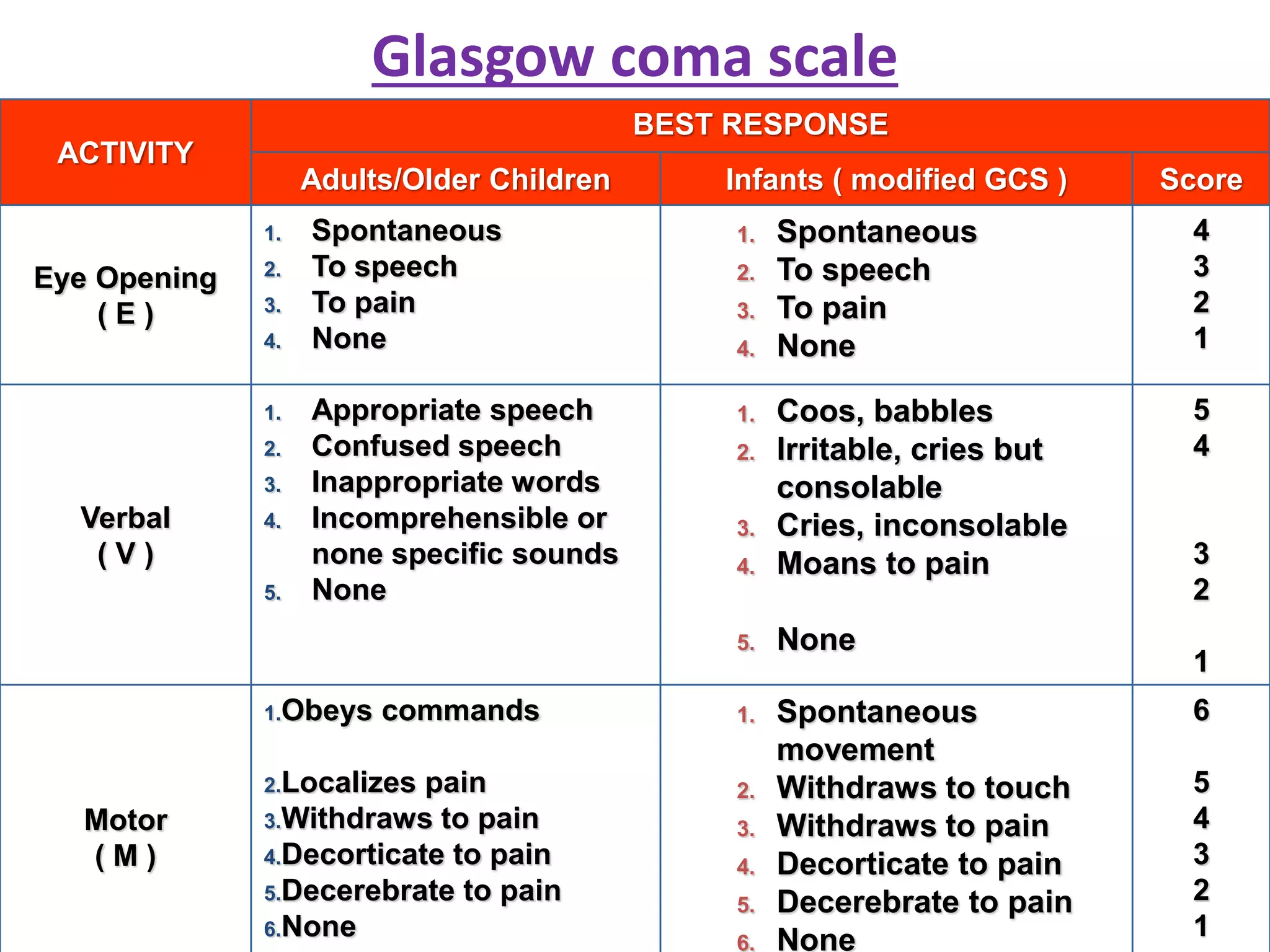
1) Disorders of consciousness range from mild impairment to coma and include conditions like confusion, delirium, vegetative state, and brain death.
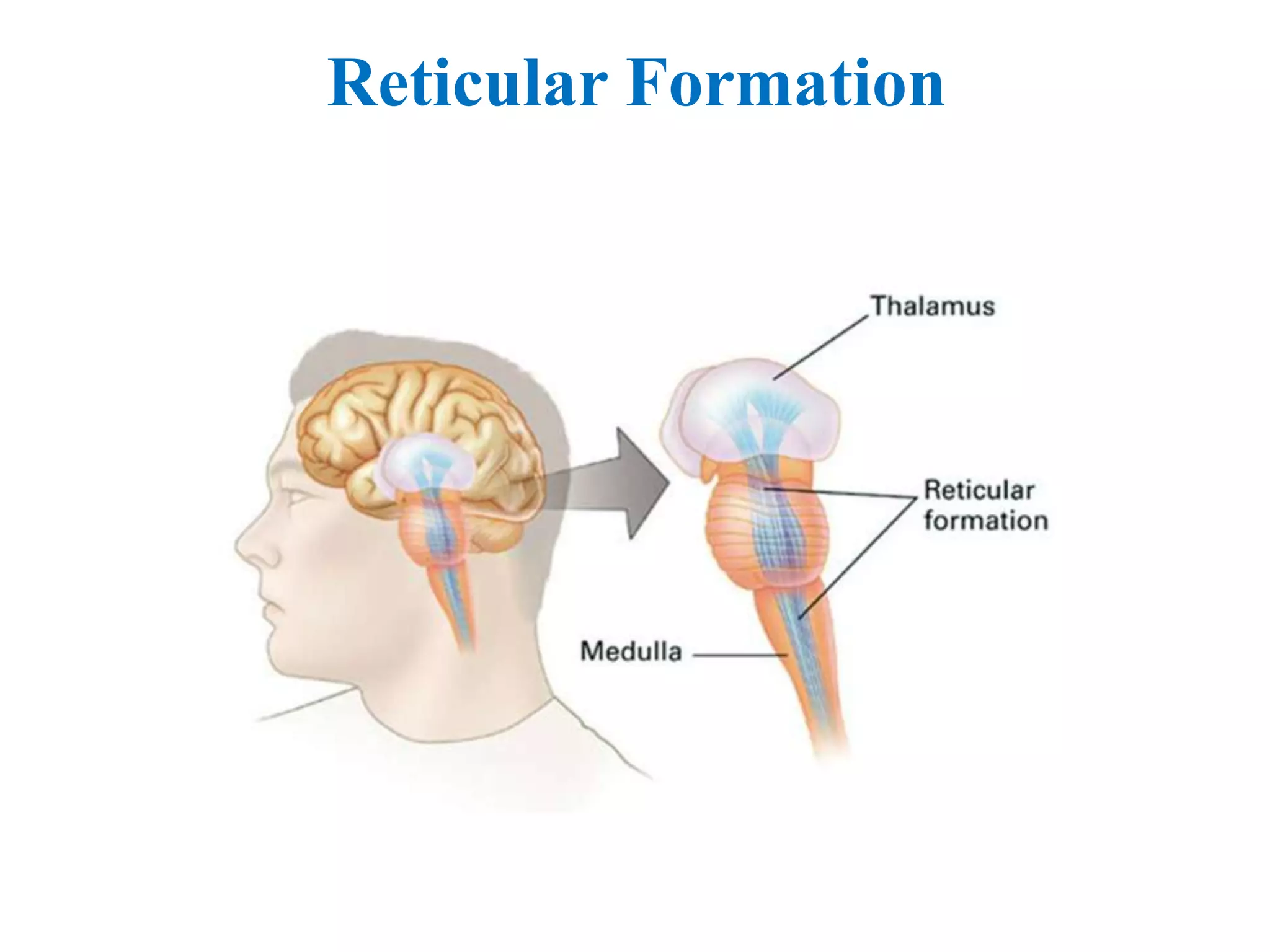
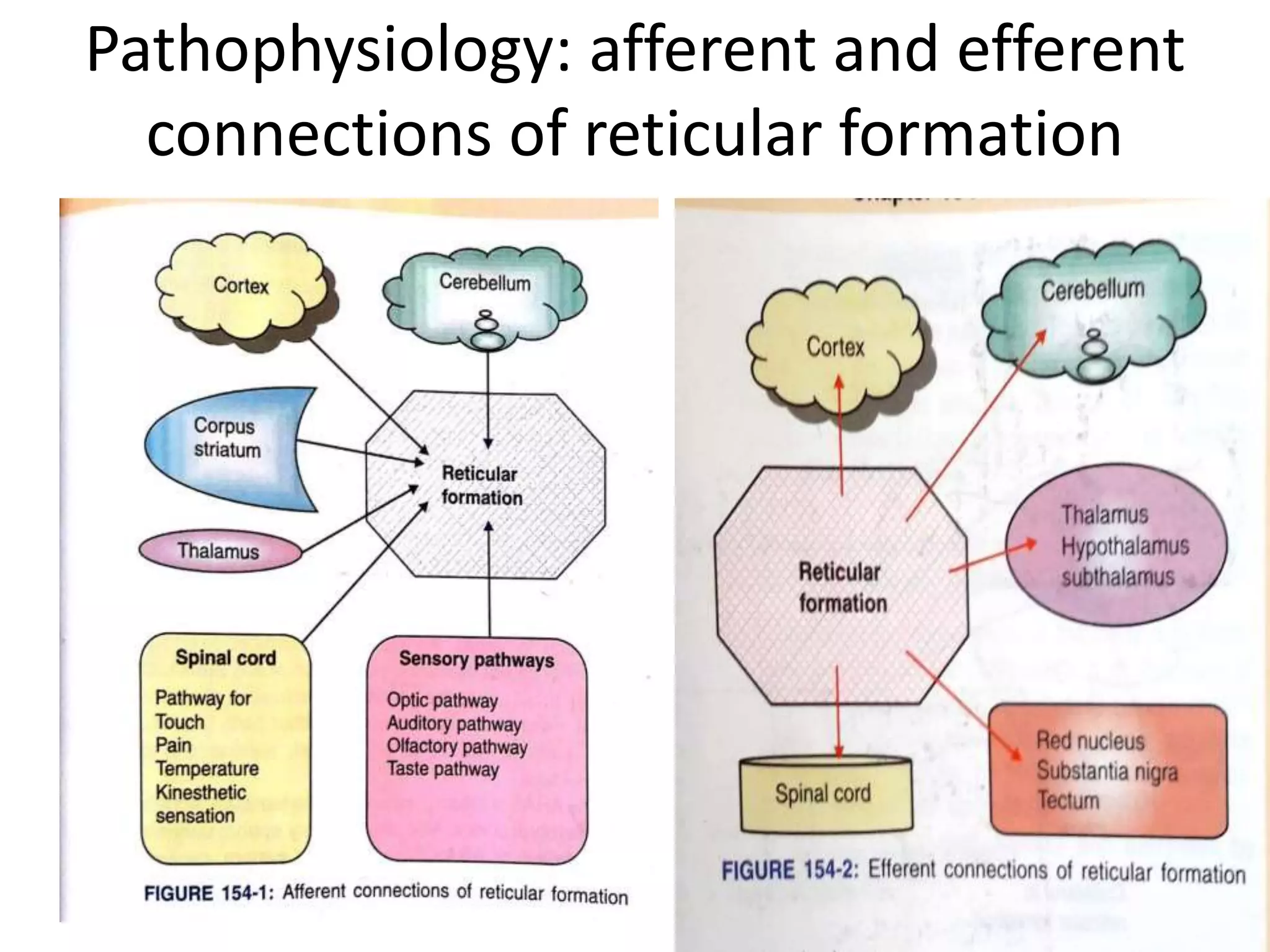
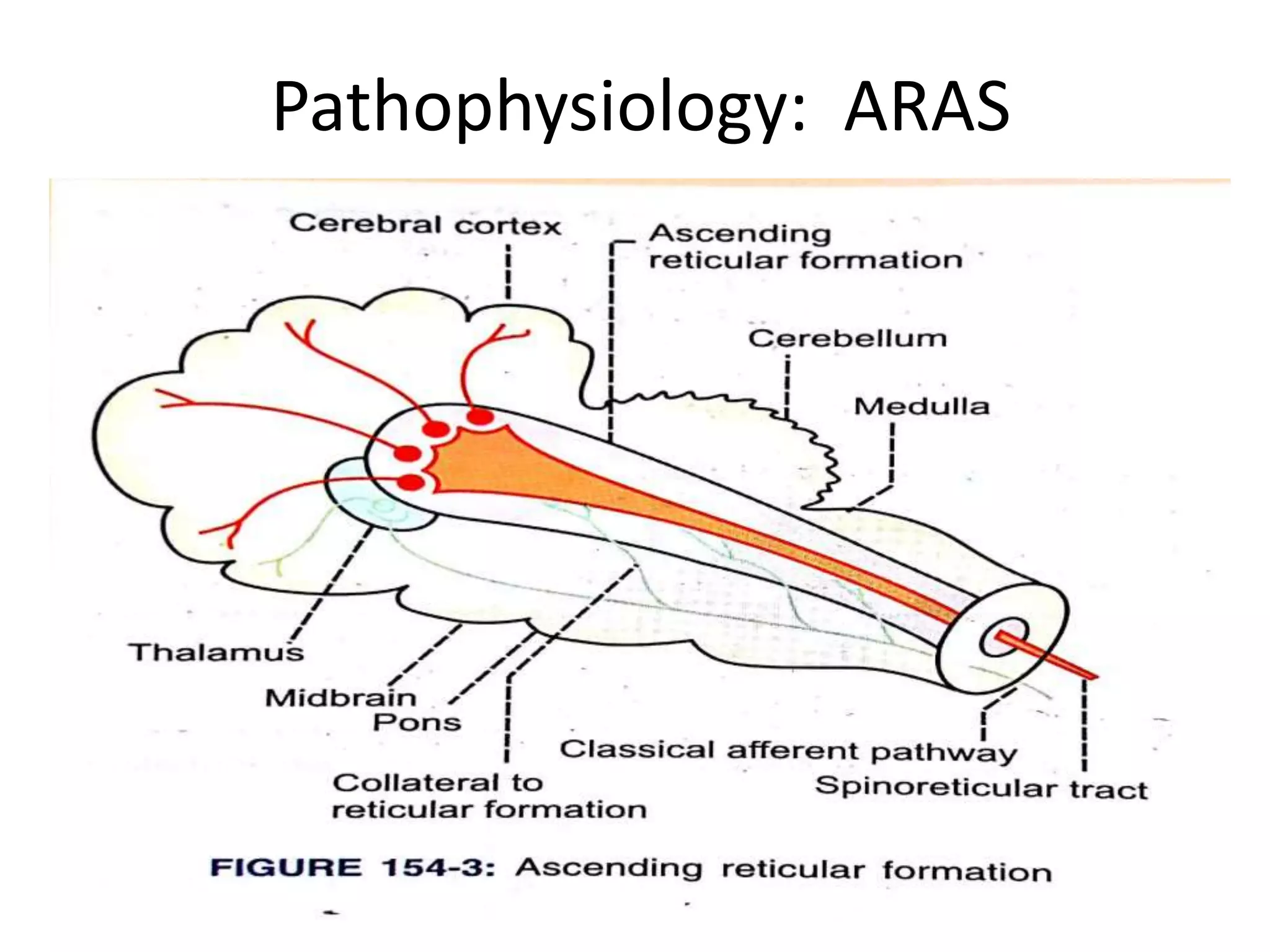
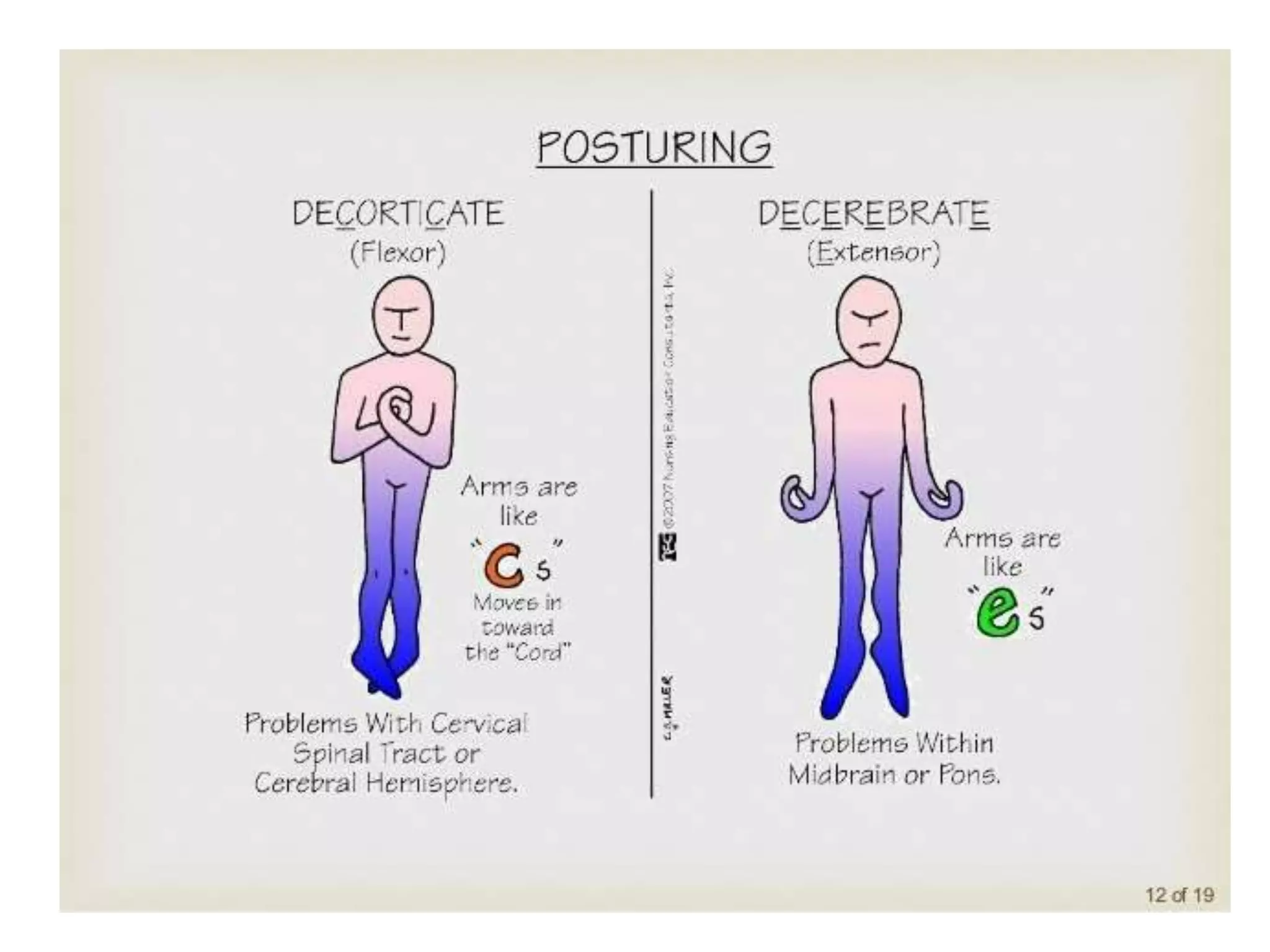
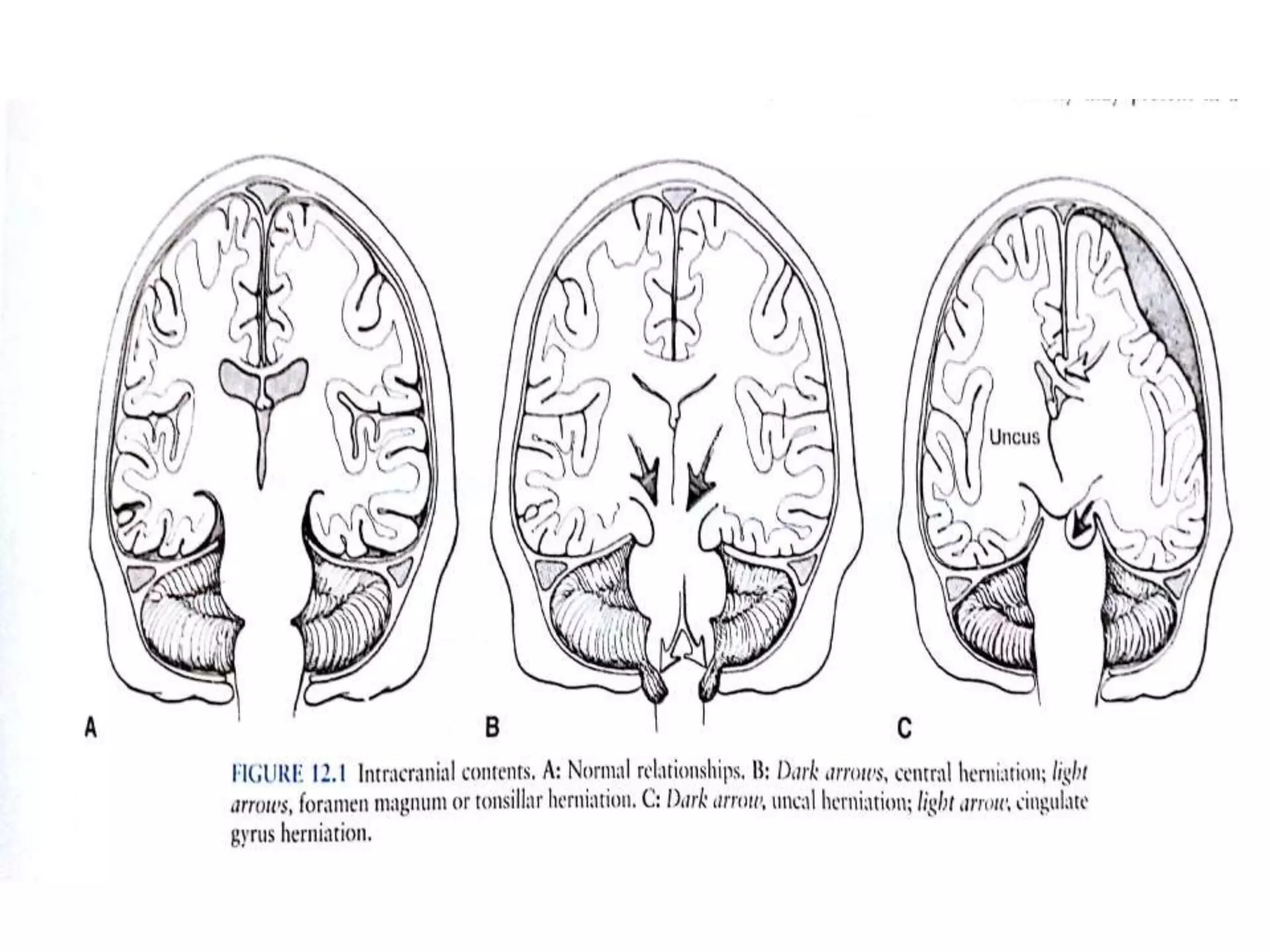
2) The pathophysiology of consciousness involves the ascending reticular activating system and connections between the brainstem and cortex. Loss of consciousness can result from disruption of these systems.
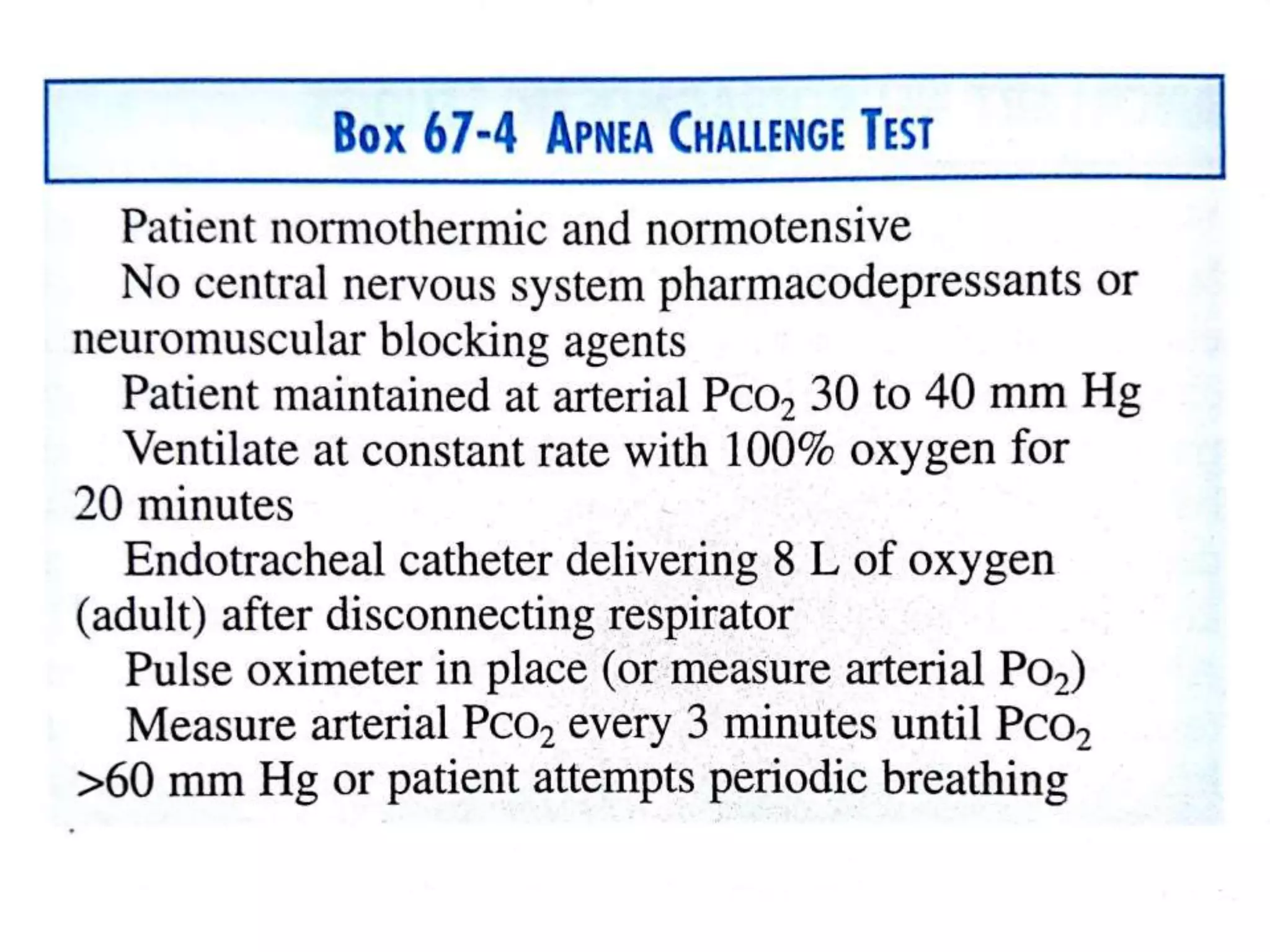
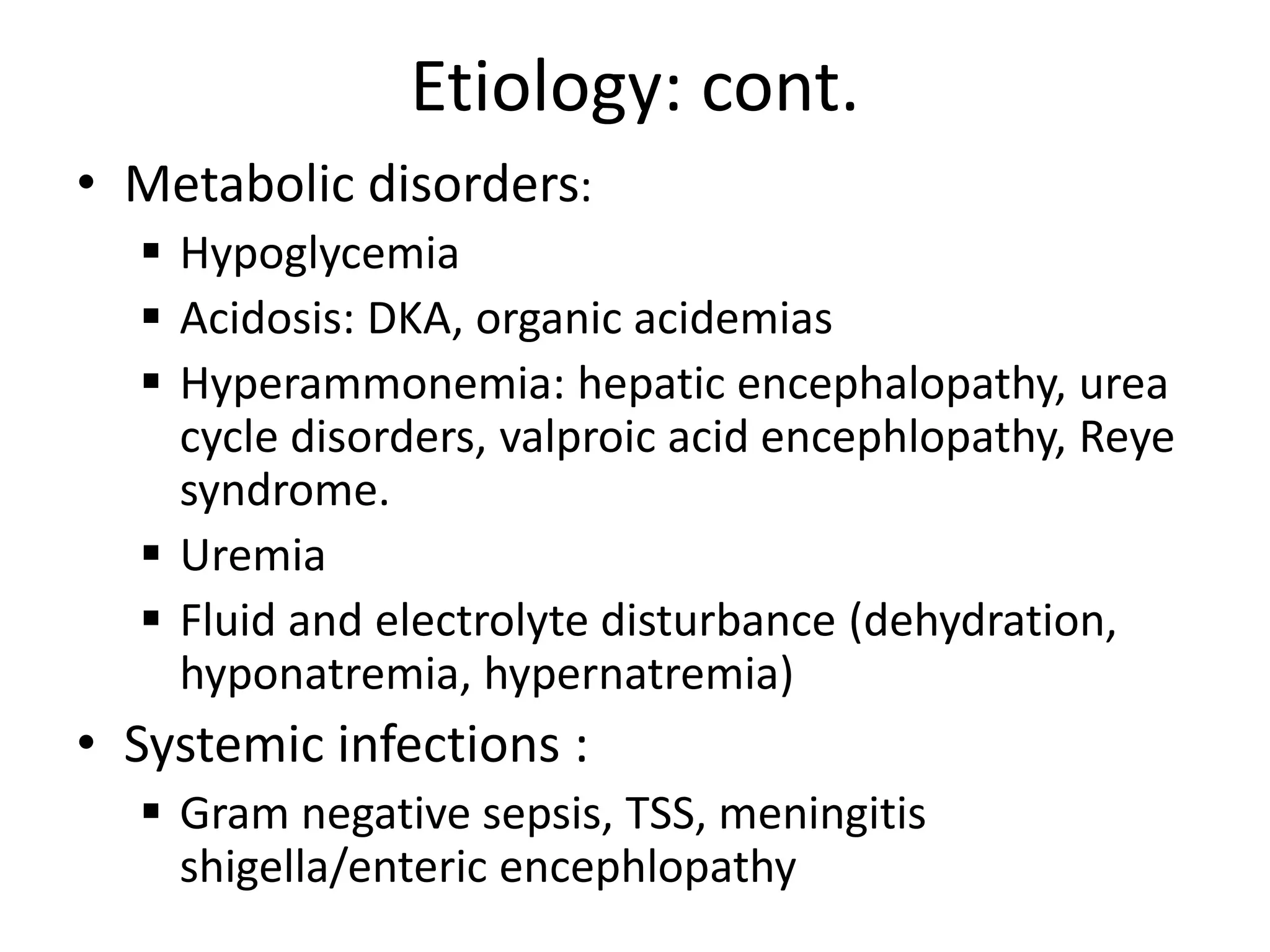
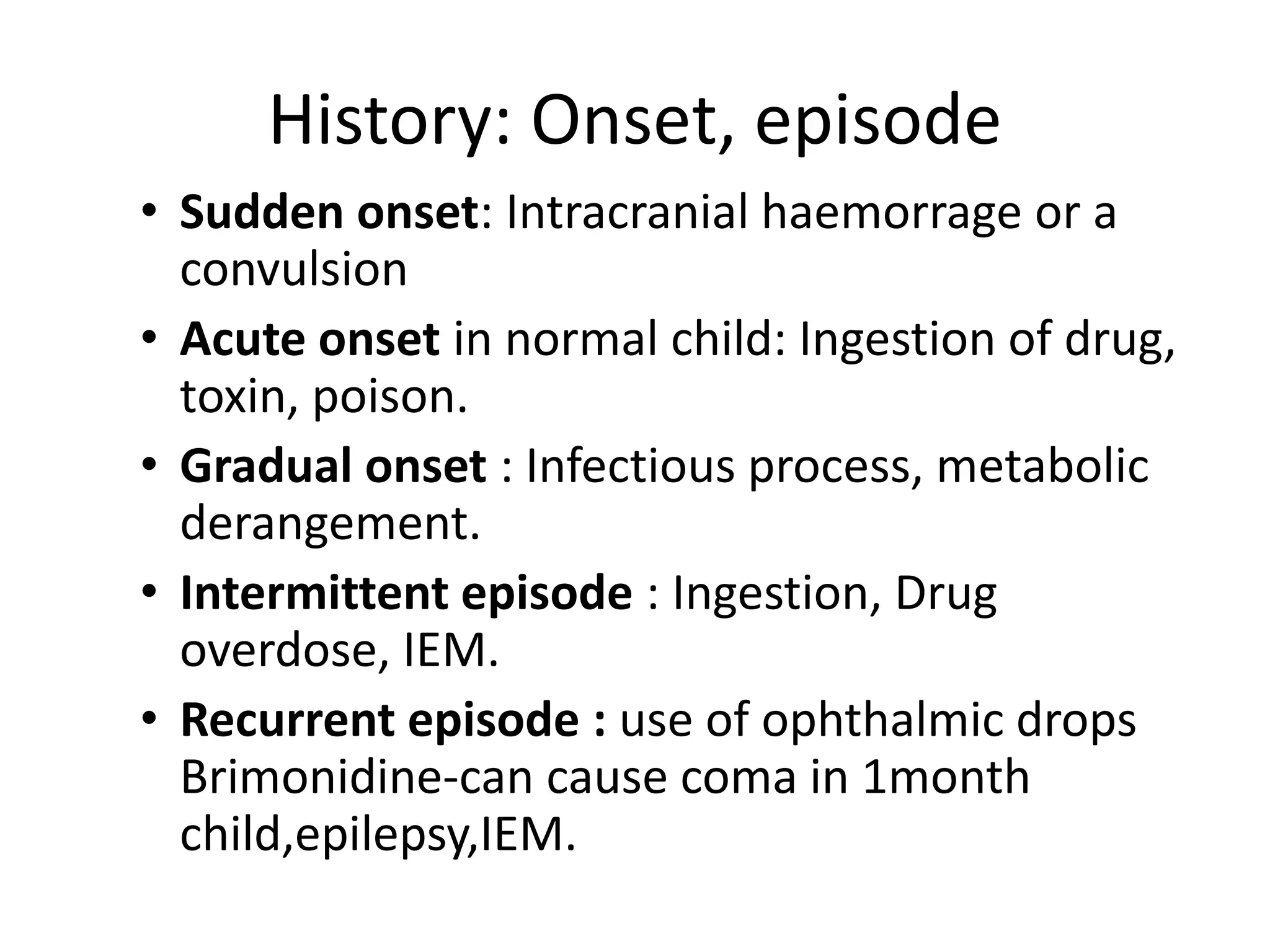
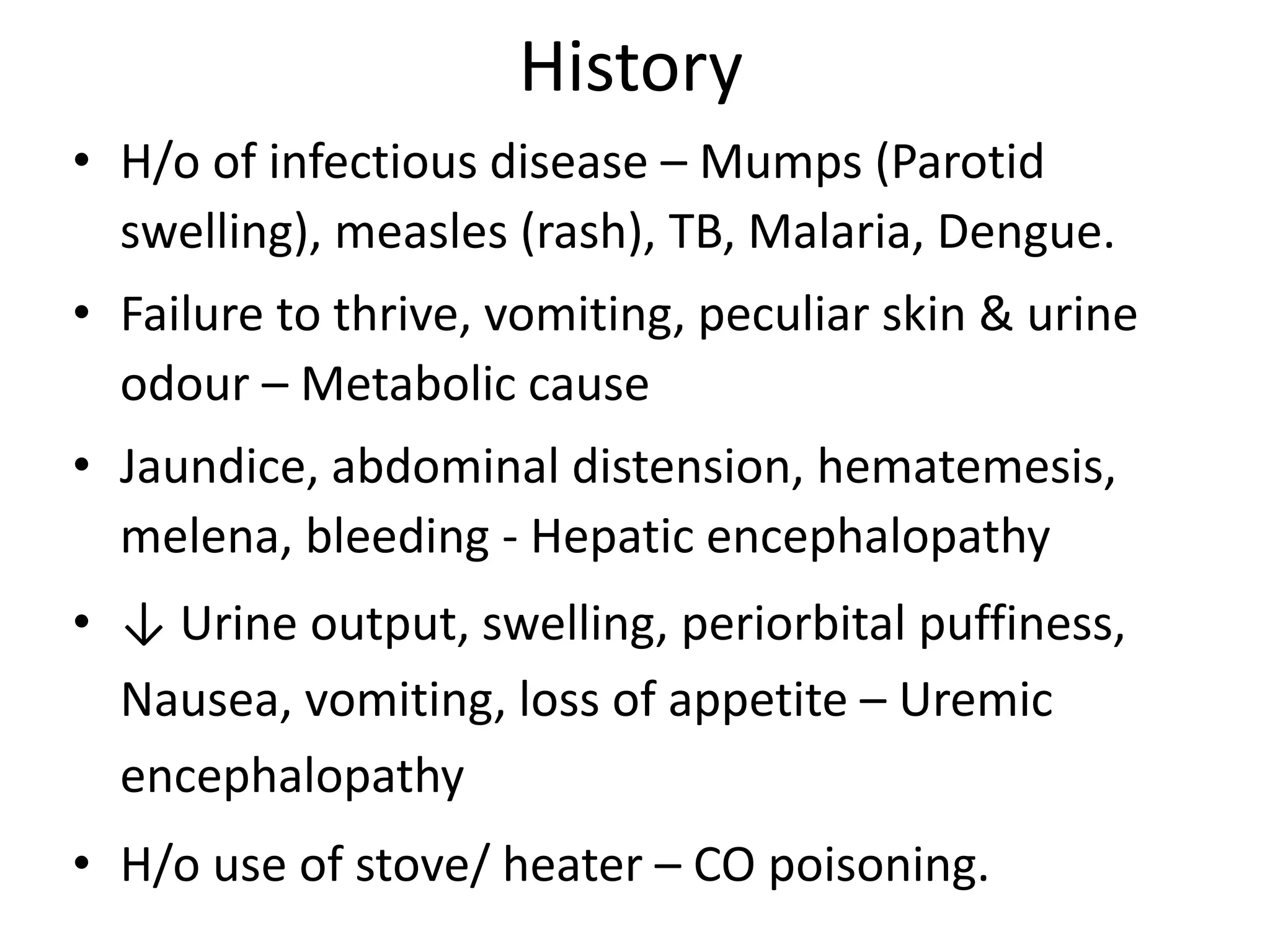
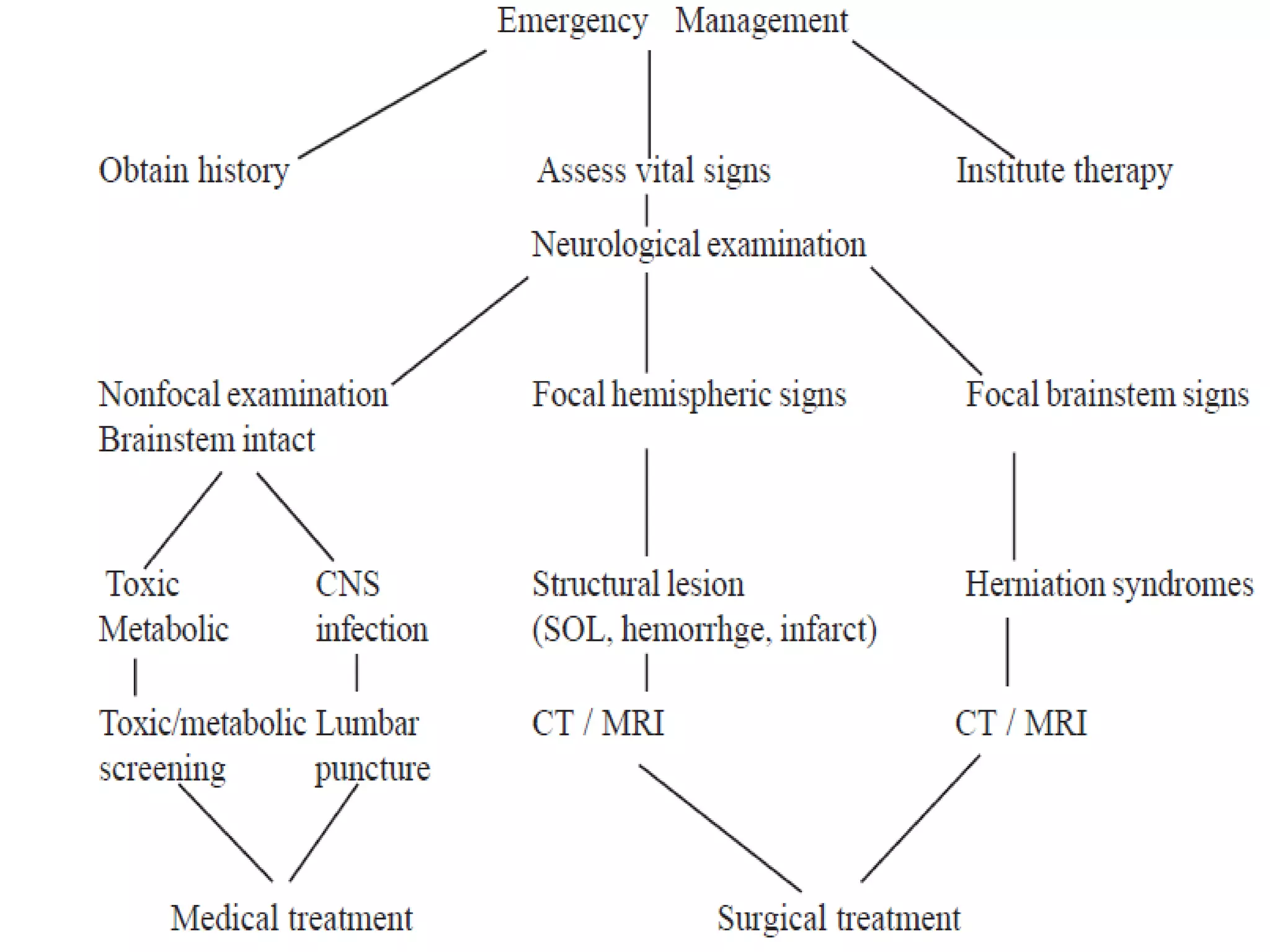
3) Etiologies of impaired consciousness and coma include infectious or inflammatory causes, structural abnormalities, and metabolic/toxic derangements. Common causes in children are infections, trauma, seizures, and metabolic disorders.