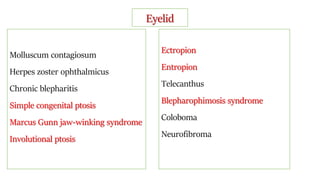
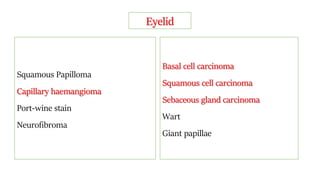
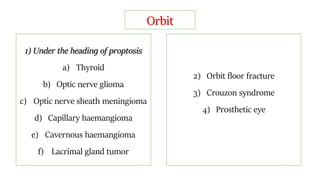
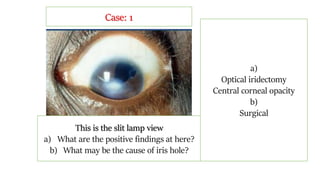
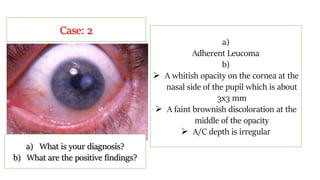
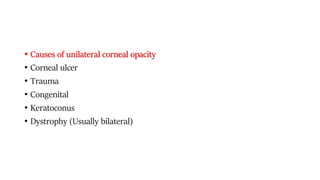
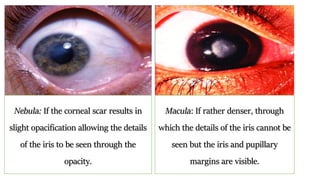
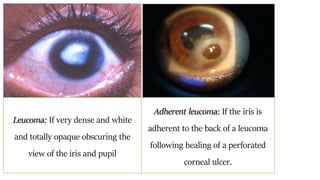
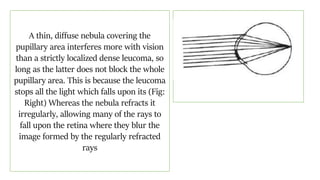
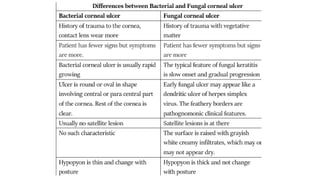
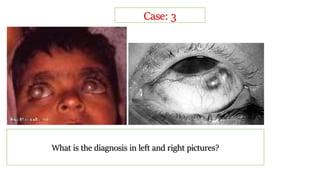
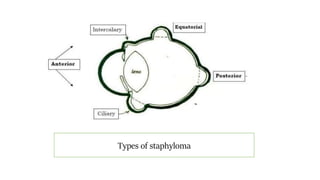
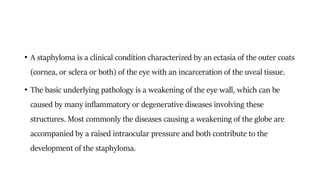
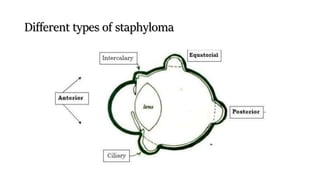
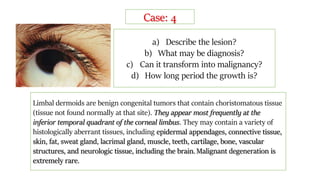
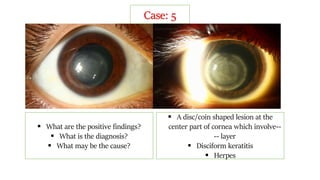
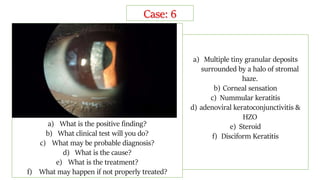
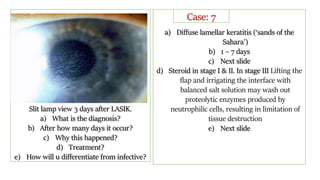
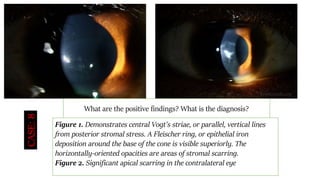
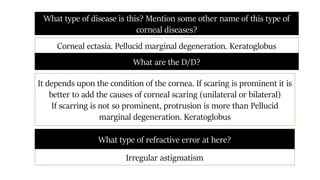
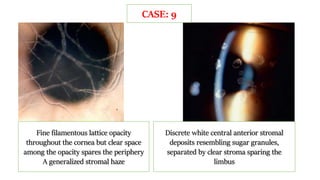
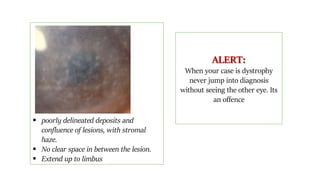
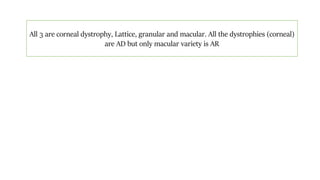
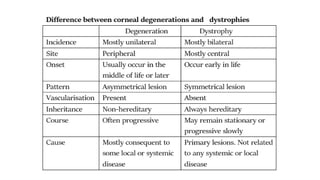
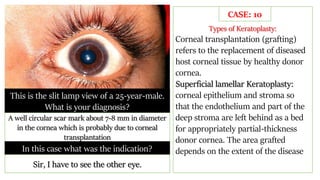
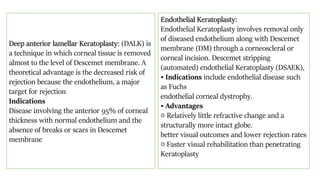
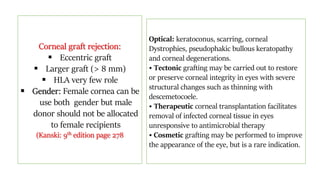
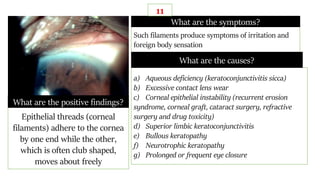
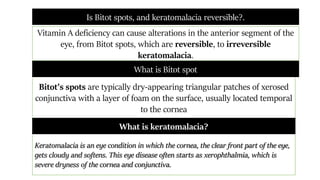
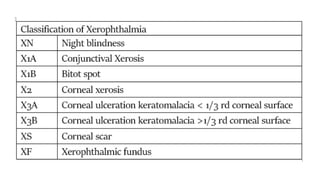
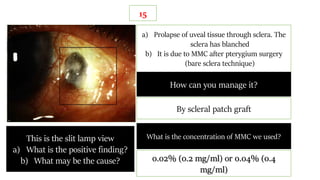
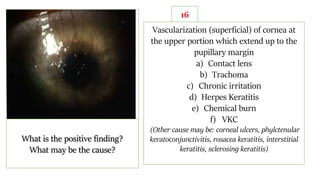
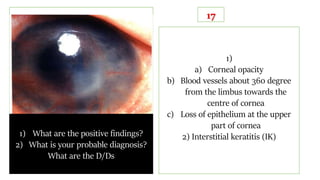
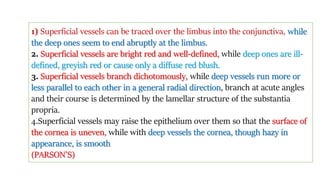
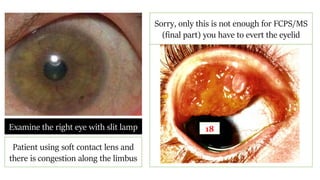
This document contains information about various eye conditions organized under headings for different structures of the eye including eyelid, orbit, cornea, complications of surgery, and miscellaneous conditions. Some specific conditions mentioned include molluscum contagiosum, blepharitis, ptosis, staphyloma, corneal opacity, disciform keratitis, nummular keratitis, diffuse lamellar keratitis, and keratoconus. Treatment options are provided for some conditions and include medications like steroids, surgical procedures like corneal transplantation, and nonsurgical approaches like rigid contact lenses. Differential diagnoses and distinguishing features between similar conditions are also outlined.