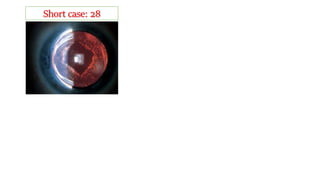
The document discusses neovascular glaucoma, noting the positive findings of neovascularization along the pupillary margin and diagnosing it as such. It states that the primary pathology is in the retina and lists common causes as ischemic central retinal vein occlusion, diabetes mellitus, central retinal artery occlusion, and ocular ischemic syndrome. The document advises that miotics should be avoided as medical treatment for neovascular glaucoma, instead recommending topical atropine, steroids if inflammation is present, and apraclonidine or oral acetazolamide.