This document provides an overview of degenerative changes that can occur in the conjunctiva, cornea, and sclera. It describes age-related changes such as thinning and loss of transparency in the conjunctiva. Specific conditions discussed include pinguecula, pterygium, conjunctival concretions, and conjunctivochalasis. Corneal degenerations covered include Coats white ring, spheroidal degeneration, iron deposition, and calcific band keratopathy. The document also briefly outlines degenerations of the sclera and endothelium and their causes, signs, and treatments.








![16
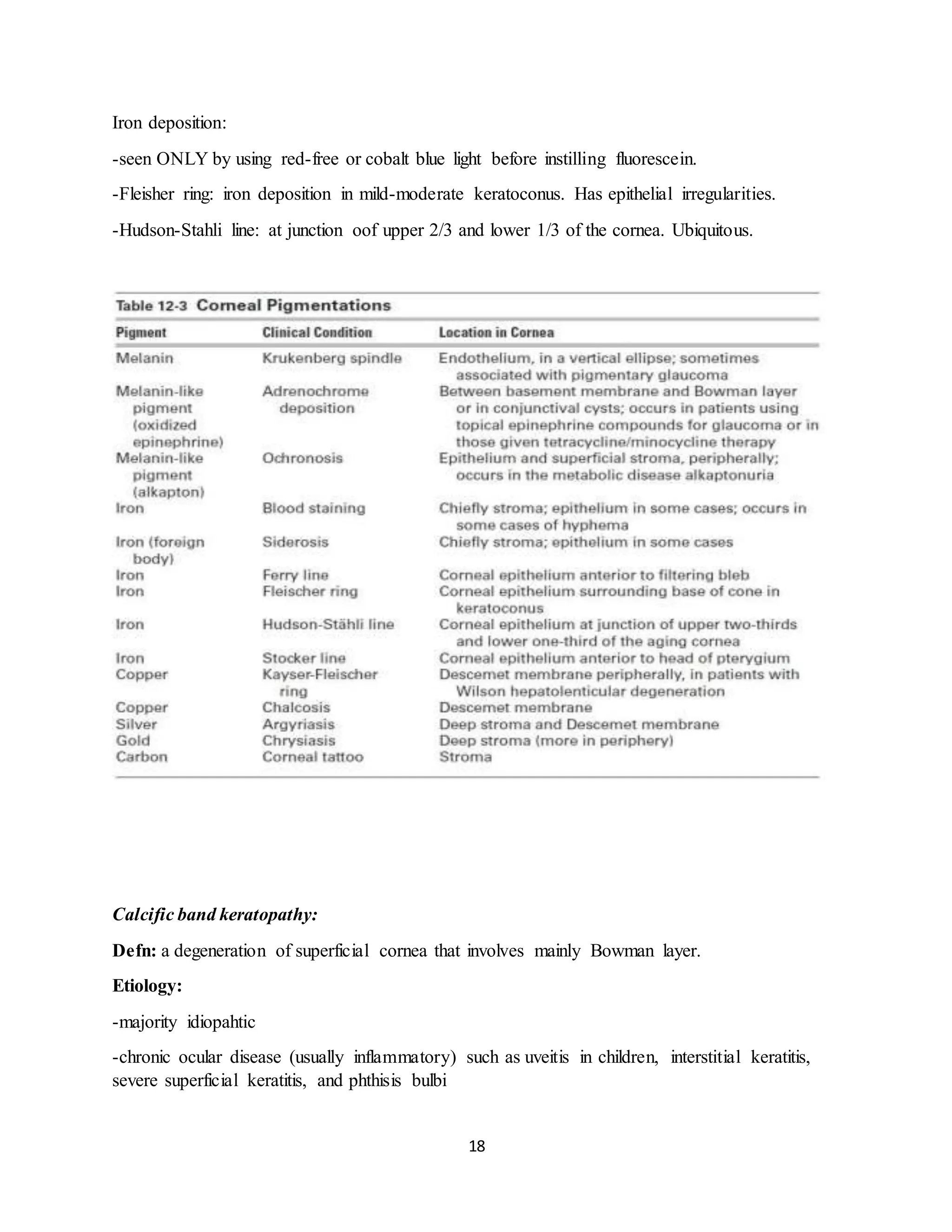
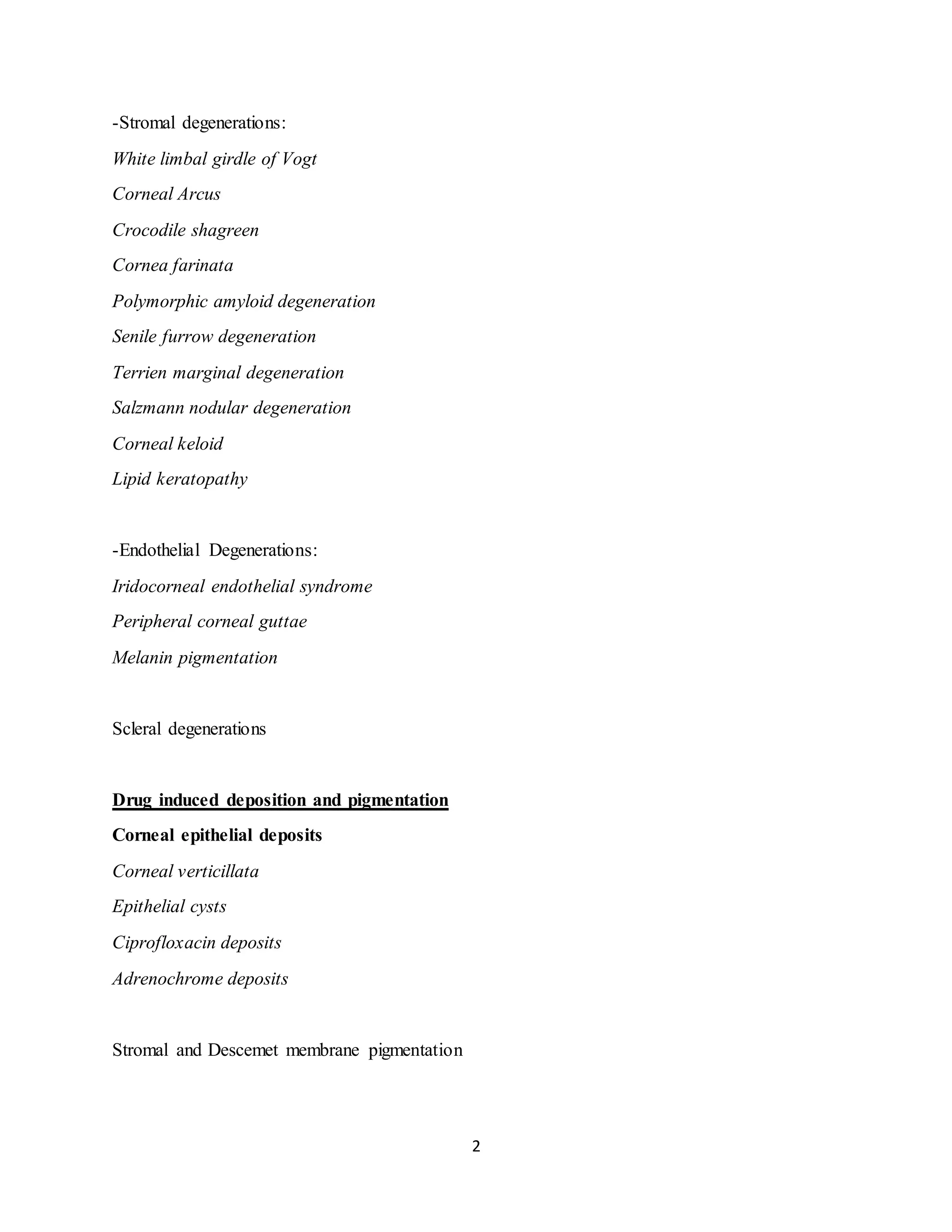
Another classification:
[A] Depending upon location
I. Axial corneal degenerations
1. Fatty degeneration
2. Hyaline degeneration
3. Amyloidosis
4. Calcific degeneration (Band keratopathy)
5. Salzmann's nodular degeneration.
II. Peripheral degenerations
1. Arcus senilis
2. Vogt's white limbal girdle
3. Hassal-Henle bodies
4. Terrien's marginal degeneration
5. Mooren's ulcer
6. Pellucid marginal degeneration
7. Furrow degeneration (senile marginal degeneration).
[B] Depending upon etiology
I. Age related degenerations. Arcus senilis, Vogt's white limbal girdle, Hassal-Henle bodies,
Mosaic degeneration.
II. Pathological degenerations: Fatty degeneration, amyloidosis, calcific degeneration,
Salzmann's nodular degeneration, Furrow degeneration, spheroidal degeneration, Pellucid
marginal degeneration, Terrien's marginal degeneration, Mooren's ulcer.](https://image.slidesharecdn.com/depositionsanddegenerationsofconjuctivaandcornea-220330173447/75/Depositions-and-Degenerations-of-Conjuctiva-and-Cornea-docx-16-2048.jpg)