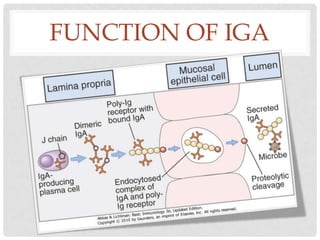
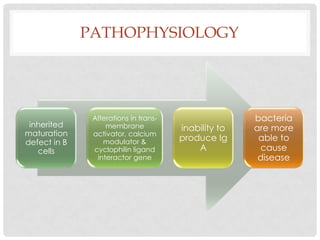
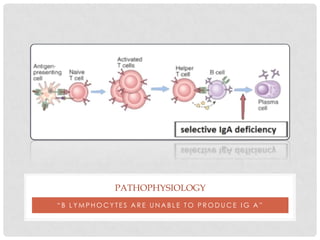
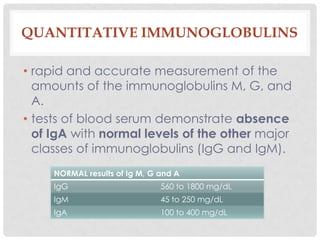
Selective IgA deficiency is the most common primary antibody deficiency, where there is an absence of IgA antibodies in the blood and secretions. IgA antibodies help protect mucosal surfaces from infection. While most people with selective IgA deficiency are asymptomatic, some experience recurrent sinopulmonary or gastrointestinal infections. The condition is diagnosed through blood tests showing low or absent IgA levels alongside normal levels of other antibodies. Treatment focuses on preventing infections and managing any associated conditions. The prognosis is generally good, though there is a small risk of developing other immune deficiencies.