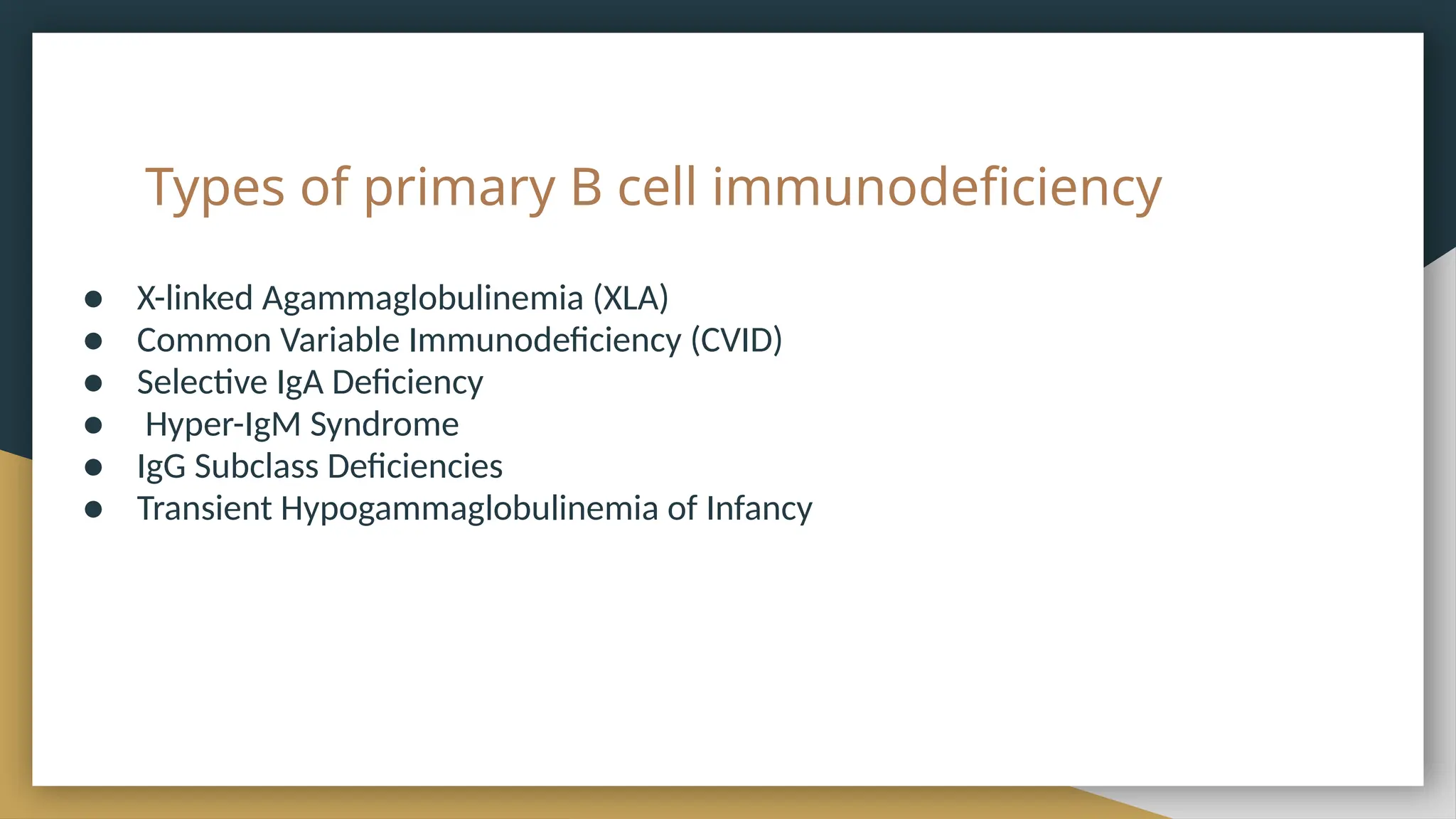
Immunodeficiency is a condition where the immune system is compromised, classified into primary (genetic) and secondary (acquired) disorders. Primary immunodeficiencies include various genetic disorders affecting B cells and antibodies, leading to increased susceptibility to infections, while secondary immunodeficiencies can arise from external factors like medications or infections. Treatment options vary, including immunoglobulin replacement, antibiotics, and in severe cases, bone marrow or stem cell transplants.