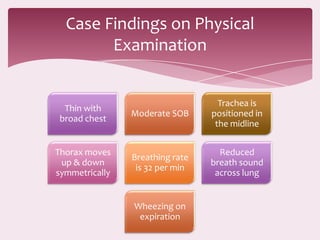
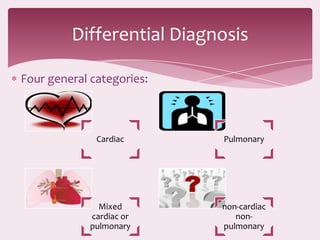
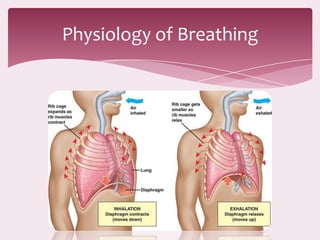
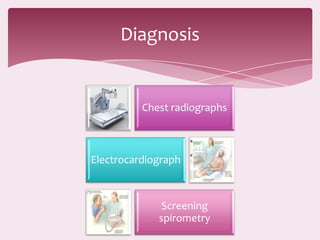
The patient is a 67-year-old male former smoker presenting with shortness of breath on exertion. Physical examination finds reduced breath sounds and wheezing. Tests show reduced lung function and oxygen levels. The differential diagnosis includes cardiac and pulmonary causes like COPD. Dyspnea is the medical term for shortness of breath and can result from various lung and heart conditions. Treatment focuses on the underlying cause, like using bronchodilators for COPD.