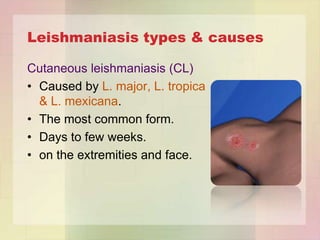
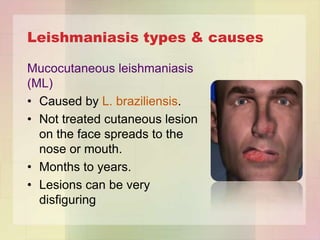
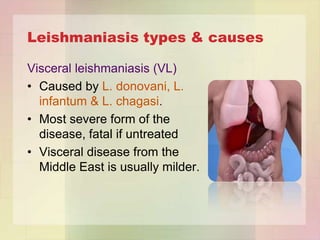
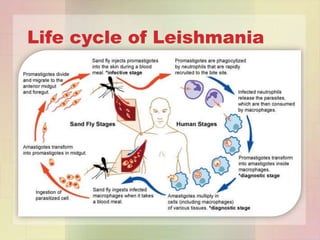
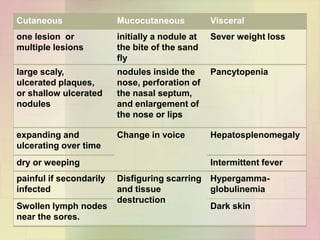
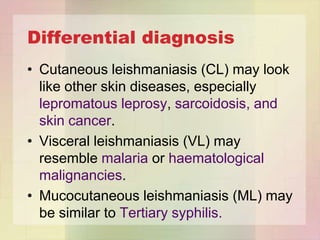
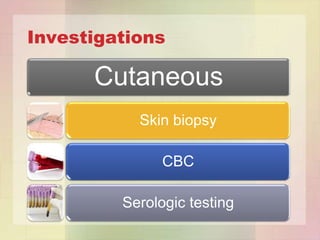
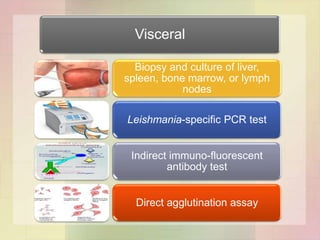
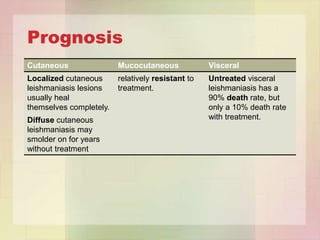
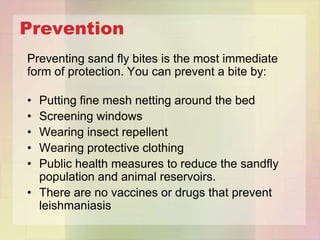
Leishmaniasis is caused by parasites of the genus Leishmania, which are transmitted via the bite of infected sand flies. There are three main clinical forms: cutaneous, mucocutaneous, and visceral leishmaniasis. Signs and symptoms vary depending on the type but can include skin lesions, facial disfigurement, fever, enlarged liver and spleen. Diagnosis involves microscopic examination, culture, serology or PCR on samples from lesions, blood or bone marrow. Treatment depends on the type but may include antimony-containing compounds or amphotericin B. Prevention focuses on avoiding sand fly bites through protective clothing and insect repellent.