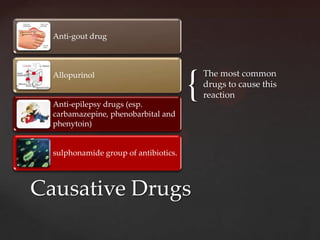
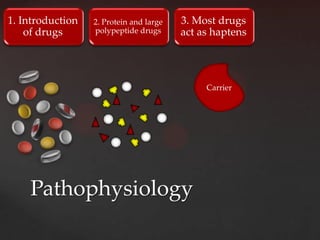
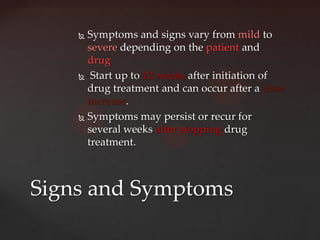
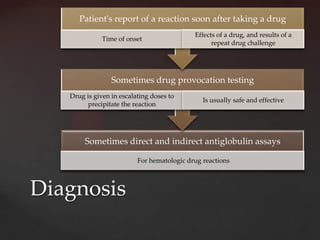
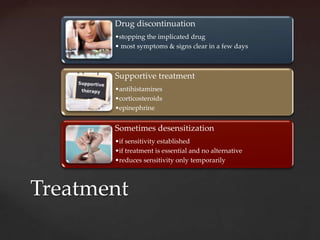
This document discusses DRESS syndrome, which stands for drug reaction with eosinophilia and systemic symptoms. It is a type of severe cutaneous adverse drug reaction characterized by a rash, fever, swelling of lymph nodes, and internal organ involvement. Common causes include certain anti-gout, anti-epilepsy, and antibiotic drugs. Signs and symptoms appear 2-8 weeks after starting the culprit drug and may persist after stopping treatment. Diagnosis involves identifying a temporal association with drug intake. Treatment involves discontinuing the drug, supportive care, and sometimes corticosteroids. Prognosis is generally good but mortality is estimated at around 8%.