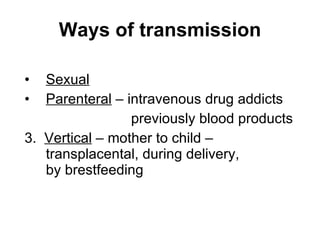
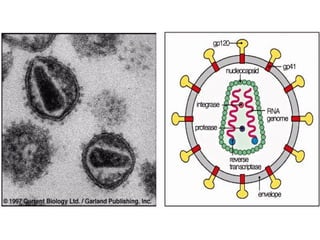
This document discusses various topics related to immunodeficiency and HIV/AIDS, including:
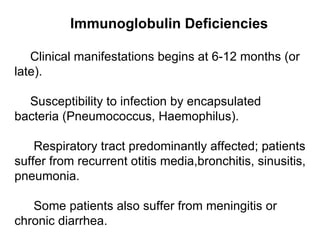
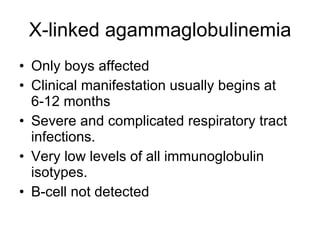
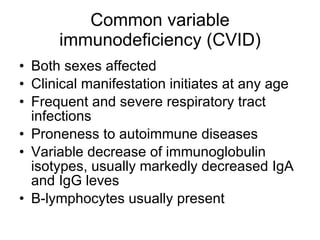
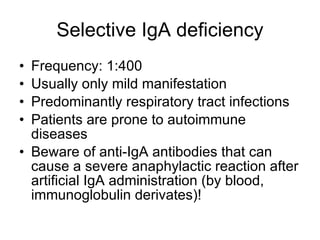
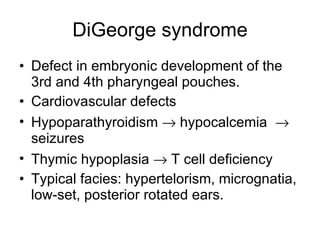
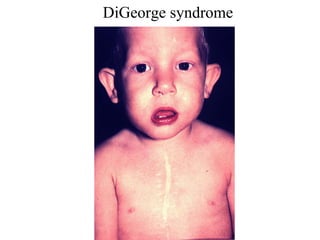
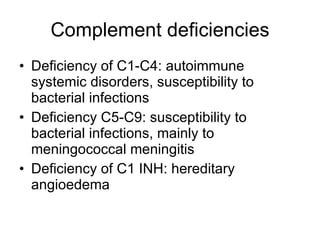
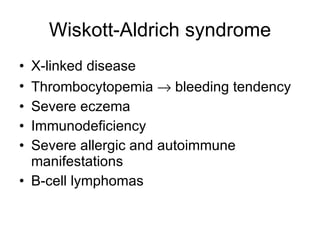
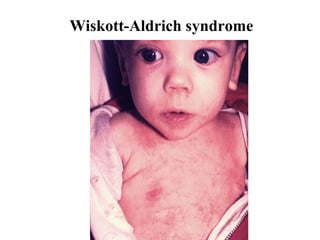
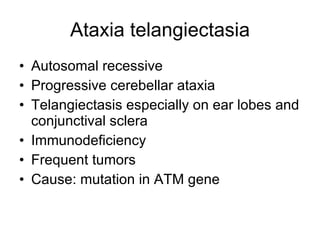
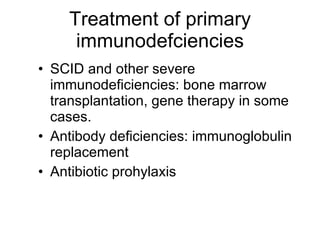
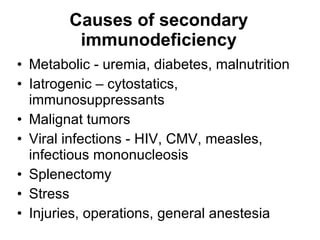
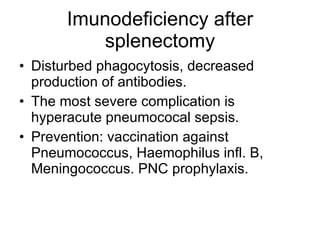
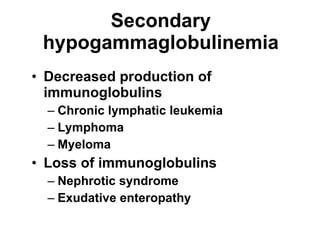
1) It describes primary and secondary immunodeficiencies, noting that primary deficiencies are caused by genetic defects while secondary deficiencies result from other diseases or environmental factors.
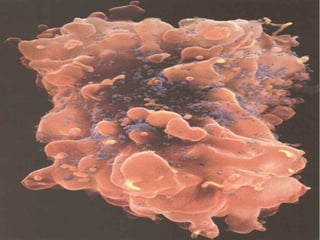
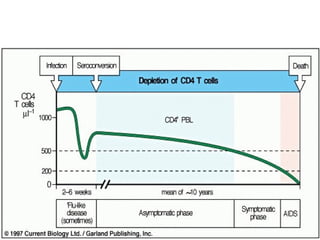
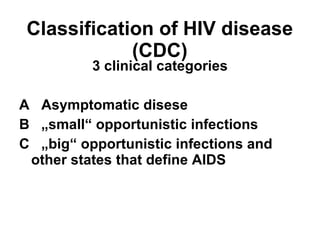
2) It provides an overview of opportunistic infections associated with AIDS, including Pneumocystis pneumonia and infections caused by toxoplasma, cytomegalovirus, and mycobacteria.
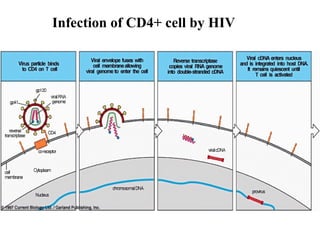
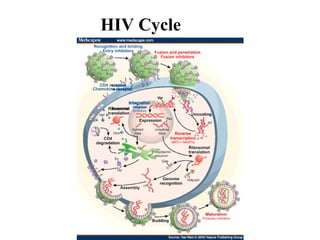
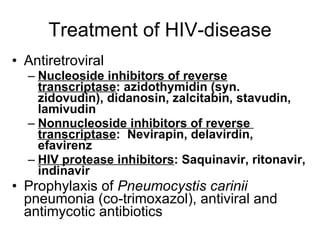
3) It discusses treatment for HIV/AIDS, including highly active antiretroviral therapy (HAART) and prophylaxis for opportunistic infections like Pneumocystis pneumonia.