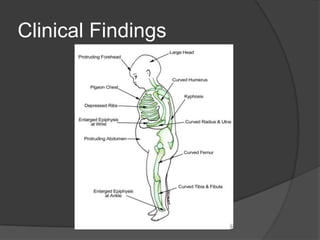
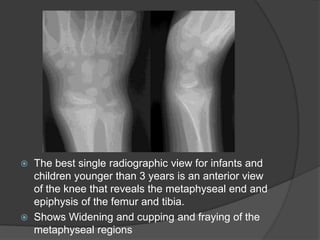
Rickets is a disease of growing bones caused by lack of vitamin D and calcium. It most commonly affects children aged 6 months to 2 years who are breastfed but not supplemented. Symptoms include bone pain, bowed legs, and fractures. Diagnosis involves blood tests showing low calcium and vitamin D levels and characteristic bone changes on x-rays. Treatment involves high dose vitamin D and calcium supplementation. Long term consequences can include permanent bone deformities if left untreated.


![epidemiologyIn developed countries, rickets is a rare disease incidence of less than 1 in 200,000In saudiarabia[1]retrospective study at King Abdulaziz Medical City-King Fahad National Guard Hospital in Riyadh, Saudi Arabia 2009196 infants (70%) were exclusively on breast-feeding (127 males, 69 females) with no supplementationThe records of Saudi infants and children under the age of 14 months over a 10-year period (between January 1990 and January 2000) were reviewed.283 infants were studied.Epidemiology of nutritional rickets in children.Al-Atawi MS, Al-Alwan IA, Al-Mutair AN, Tamim HM, Al-Jurayyan NA.Department of Pediatric, National Guard Health Affairs, King Abdulaziz Medical City, Riyadh, Saudi Arabia](https://image.slidesharecdn.com/rickets-101227064437-phpapp02/85/Rickets-4-320.jpg)
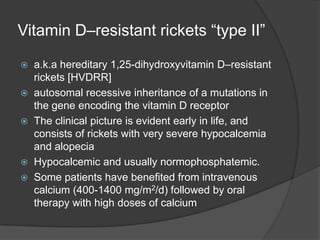


![Vitamin D–resistant rickets “type II”a.k.a hereditary 1,25-dihydroxyvitamin D–resistant rickets [HVDRR]autosomal recessive inheritance of a mutations in the gene encoding the vitamin D receptorThe clinical picture is evident early in life, and consists of rickets with very severe hypocalcemia and alopeciaHypocalcemic and usually normophosphatemic. Some patients have benefited from intravenous calcium (400-1400 mg/m2/d) followed by oral therapy with high doses of calcium](https://image.slidesharecdn.com/rickets-101227064437-phpapp02/85/Rickets-32-320.jpg)