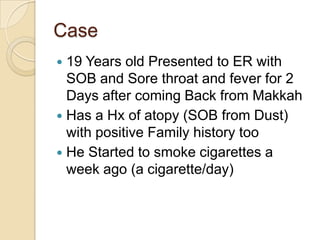
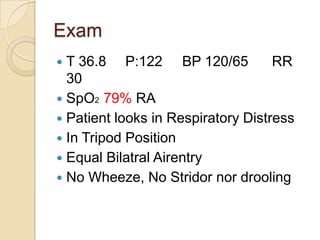
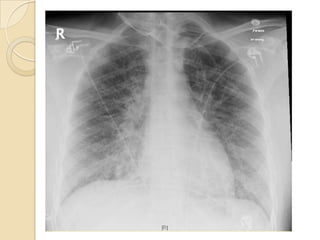
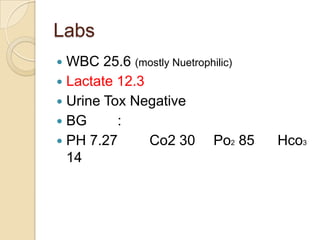
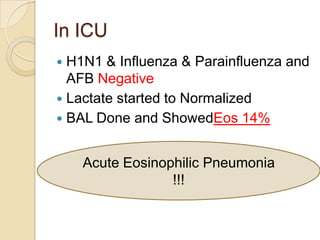
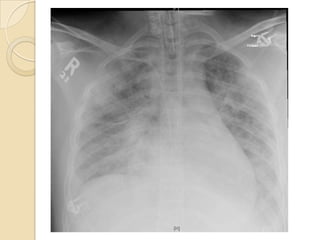
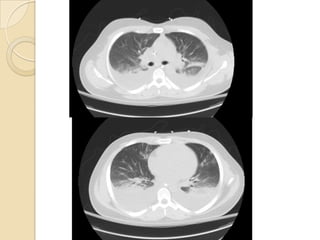
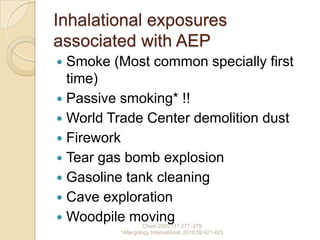
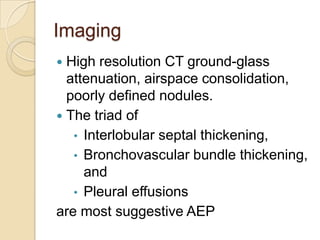
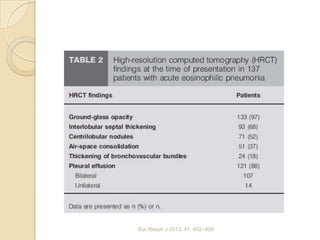
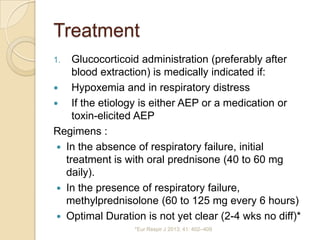
This document summarizes a case of acute eosinophilic pneumonia. A 19-year-old male presented with shortness of breath, sore throat, and fever after returning from Mecca. Exams found respiratory distress and hypoxemia. Tests showed elevated white blood cells and eosinophils in the lungs. Acute eosinophilic pneumonia was diagnosed based on lung biopsy findings and exclusion of other causes. The patient was treated with corticosteroids and supportive care and had an improvement in symptoms. Acute eosinophilic pneumonia is a rare lung disease characterized by lung tissue eosinophilia and often associated with smoking or other inhalational exposures.