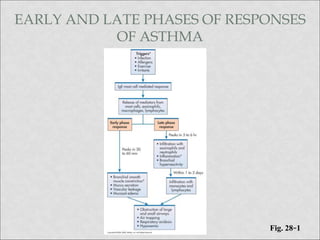
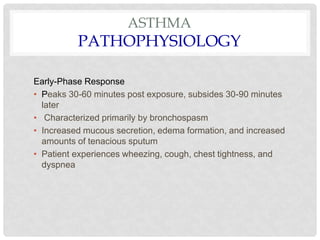
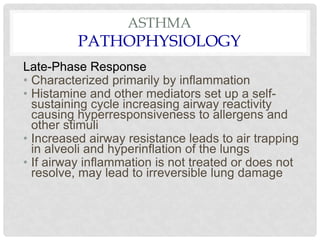
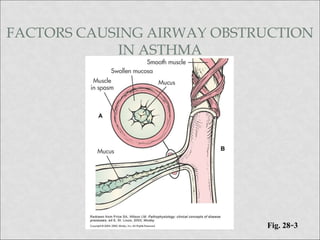
Asthma is a chronic inflammatory lung disease characterized by reversible airway obstruction. It is triggered by allergens, exercise, infections, and other factors. An asthma attack involves early and late phase responses, with bronchospasm and inflammation causing symptoms like wheezing and difficulty breathing. Nursing management of asthma focuses on monitoring the patient, administering medications to reverse bronchoconstriction and reduce inflammation, teaching self-management techniques, and helping the patient avoid triggers and maintain normal activity levels.
![BETA AGONISTS
• Bronchodilators
• -adrenergic agonists
(e.g., albuterol, salbutamol[Ventolin])
• Acts in minutes, lasts 4 to 8 hours
• Short-term relief of bronchoconstriction
• Treatment of choice in acute exacerbations](https://image.slidesharecdn.com/asthma-211214111932/85/Asthma-22-320.jpg)