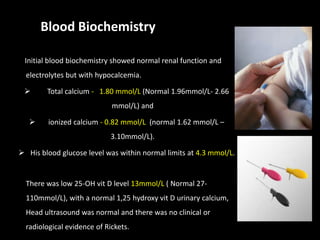
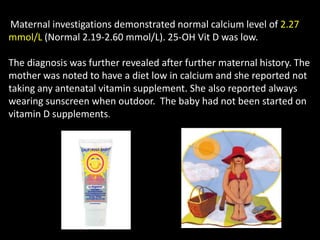
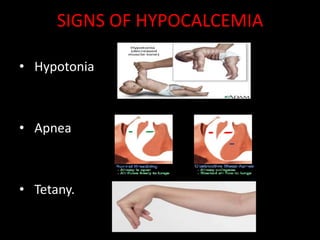
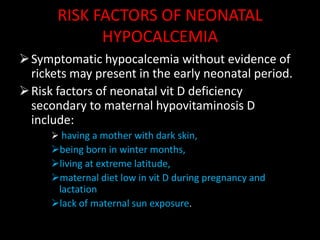
This case report describes a 10-day-old boy admitted with new onset convulsions. Initial blood tests showed hypocalcemia. The cause was found to be maternal hypovitaminosis D due to a diet low in calcium and no prenatal vitamin supplements. The mother also always wore sunscreen outdoors. The baby was treated with IV calcium supplementation and oral calcium and vitamin D, and his seizures resolved within 48 hours. This case highlights the risk of neonatal hypocalcemia and seizures due to maternal vitamin D deficiency during pregnancy.