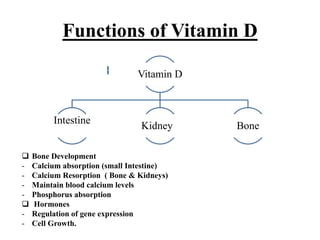
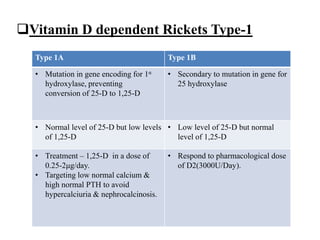
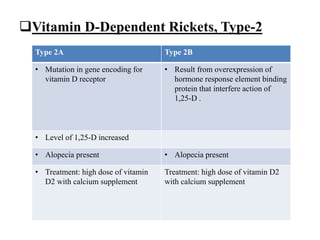
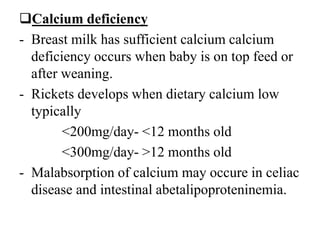
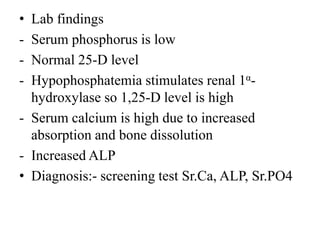
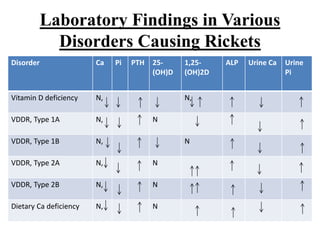
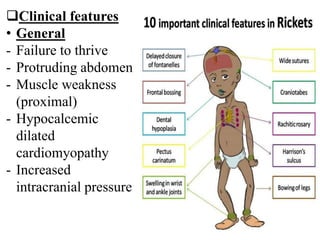
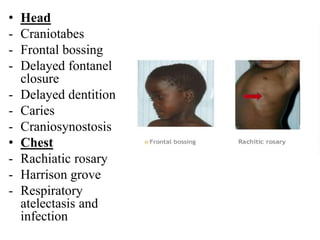
The document discusses rickets, a condition affecting bone development in children caused by vitamin D deficiency, leading to weak bones and deformities. It outlines the causes, diagnostic approach, and treatment options for rickets and related conditions, emphasizing the importance of appropriate vitamin D, calcium, and phosphorus levels in prevention and management. Clinical features and laboratory findings associated with rickets are also detailed, including nutritional deficiencies and various forms of vitamin D-dependent rickets.