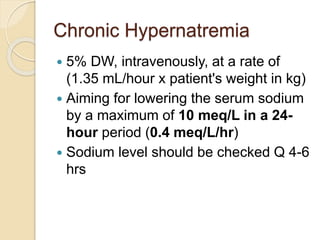
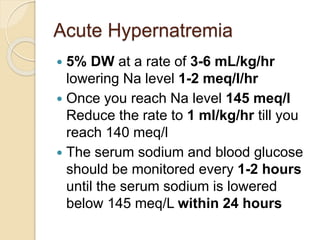
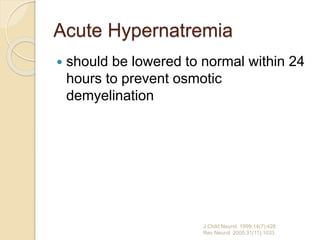
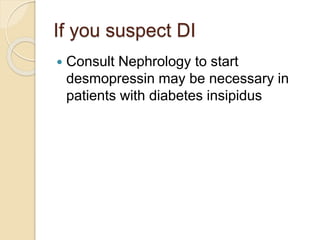
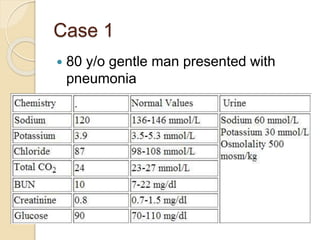
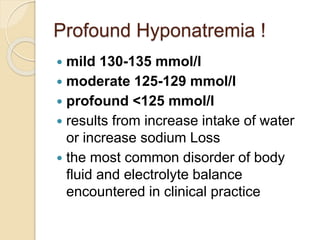
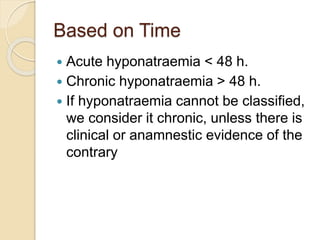
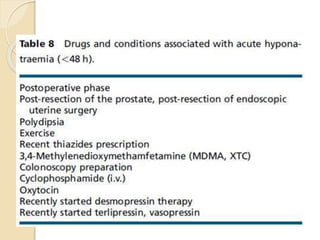
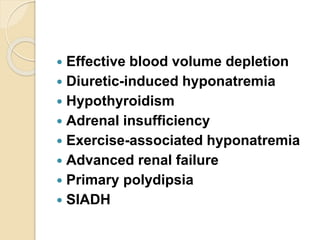
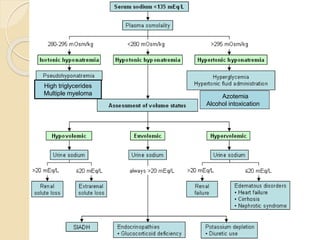
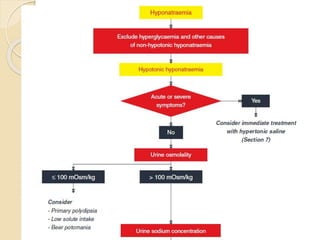
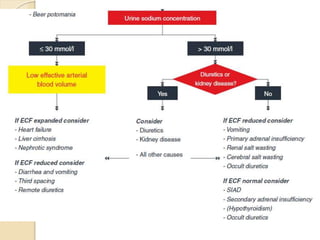
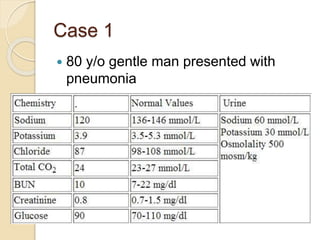
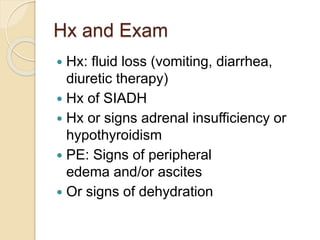
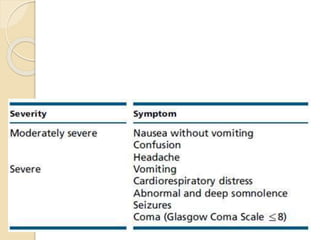
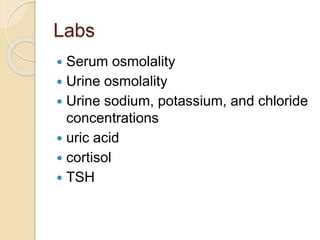
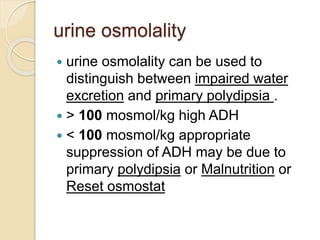
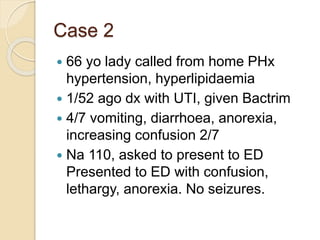
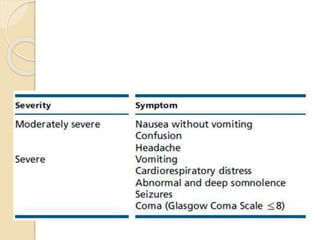
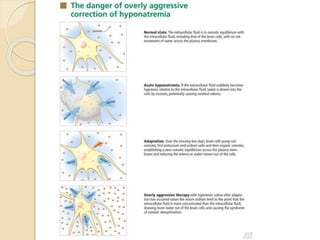
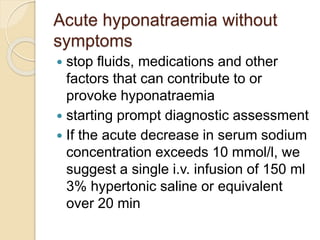
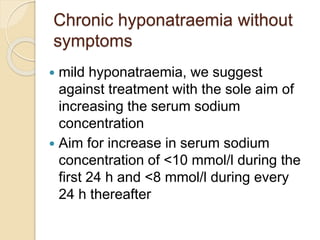
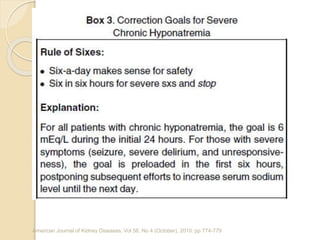
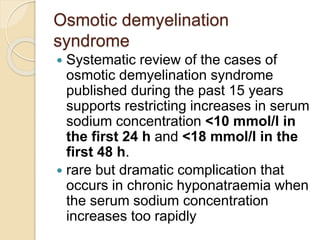
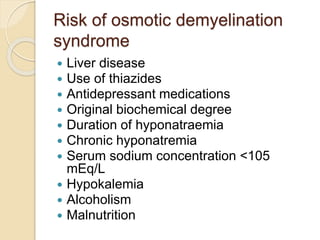
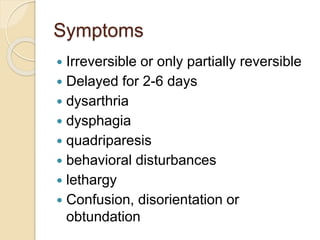
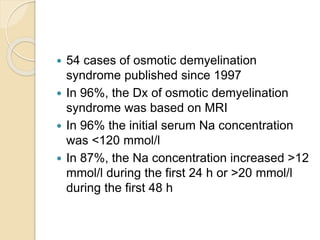
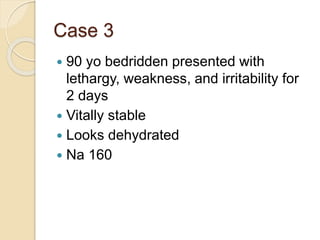
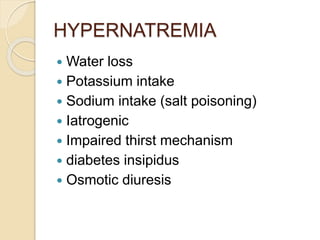
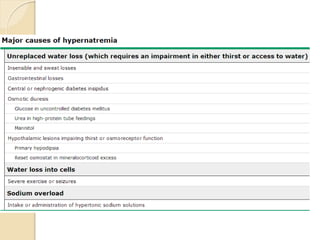
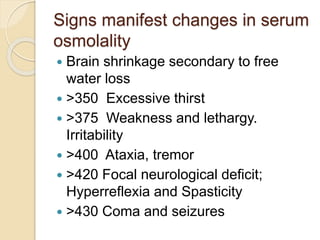
This document provides an overview of sodium disorders, including definitions, classifications, approaches, etiologies, and treatments. It discusses hyponatremia and hypernatremia. Hyponatremia is classified based on sodium level, onset, volume status, and osmolality. Treatment depends on factors like underlying cause, symptoms, and chronicity. Rapid correction of sodium levels can cause osmotic demyelination syndrome. Hypernatremia treatment involves slow correction based on calculated water deficit to avoid neurological issues. The document also presents three case studies and guidelines for evaluating and managing different sodium disorder presentations.

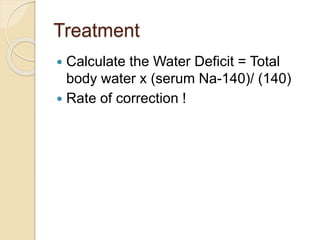
![Fast or slow correction in
elderlies with acute symptoms !
Correction of less than 6 meq/L per
day [<0.25 meq/L/hr] should be
avoided
slow rate of hypernatremia correction
during the first 24 hours were found to
be significant predictor of 30-day
patient mortality
Am J Med Sci. 2011 May;341(5):356-60](https://image.slidesharecdn.com/naandmgdisorders2-211214111959/85/Na-and-mg-disorders-2-62-320.jpg)