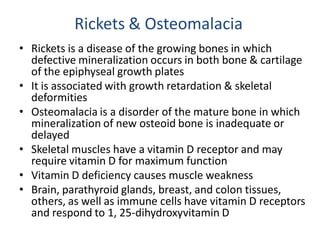
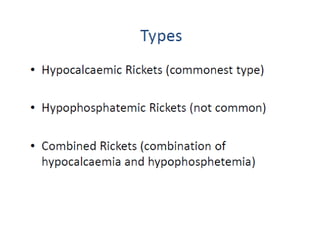
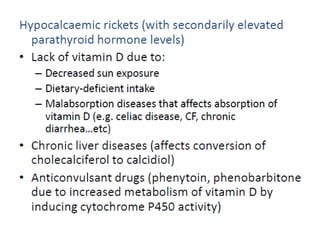
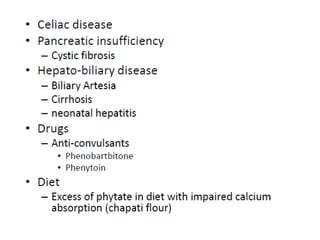
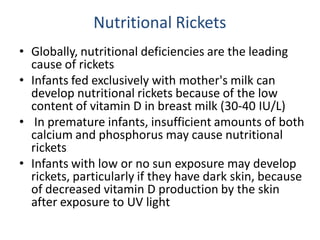
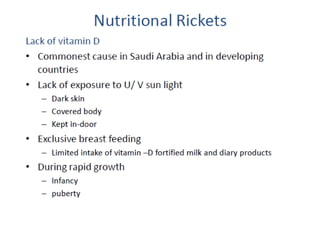
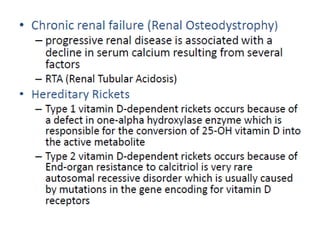
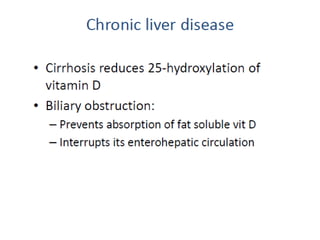
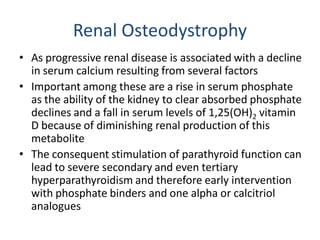
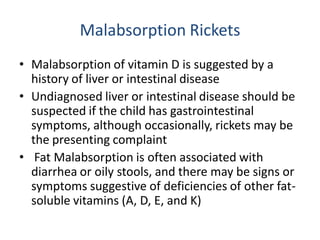
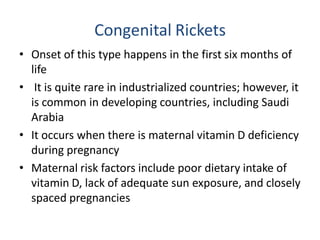
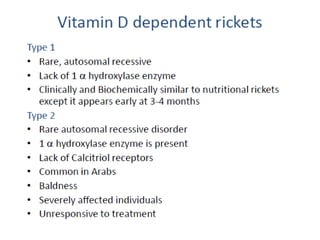
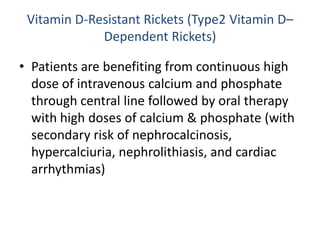
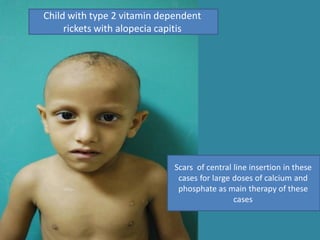
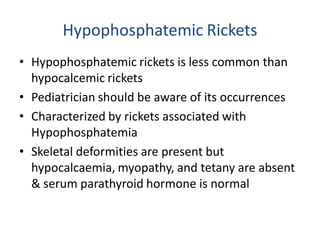
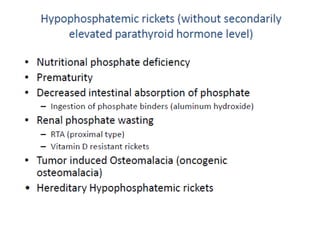
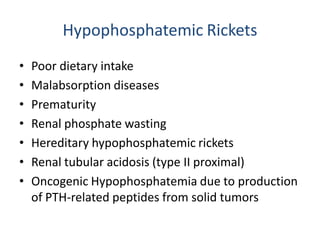
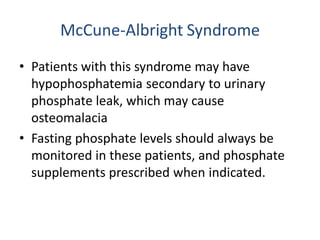
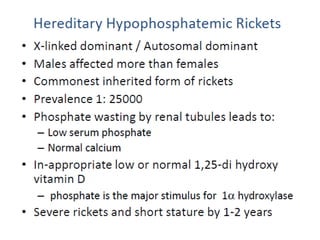
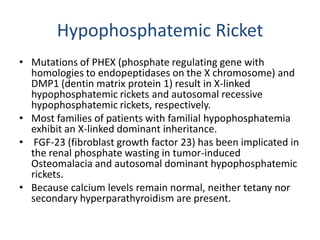
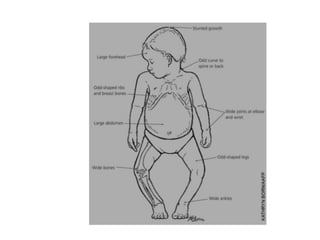
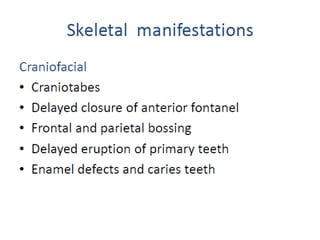
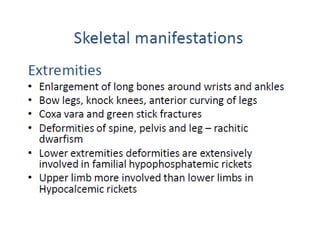
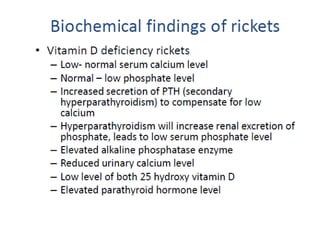
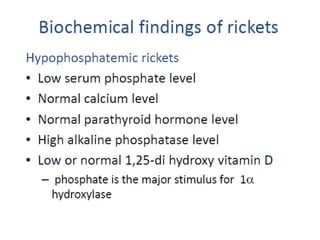
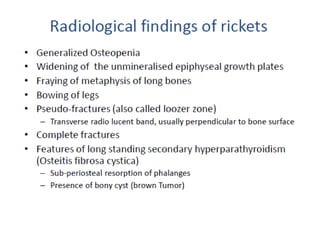
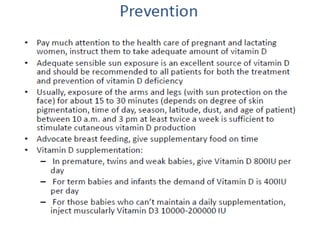
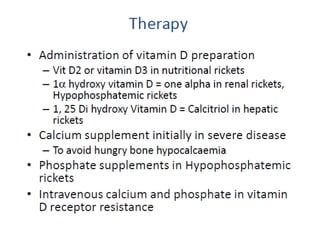
Rickets is a disease affecting bone mineralization in children. It causes skeletal deformities and stunted growth. The document discusses the different types of rickets including nutritional rickets due to vitamin D or calcium deficiency, renal rickets, and genetic forms. Symptoms, causes, treatments, and prevention strategies are covered for each type of rickets.