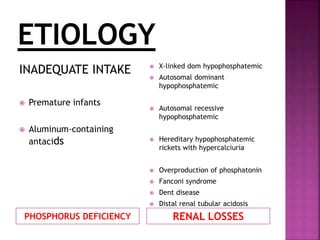
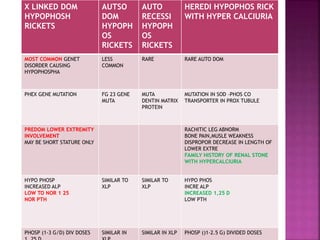
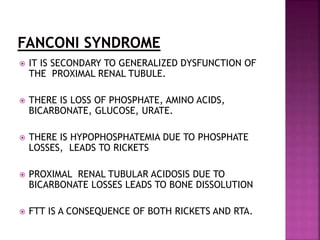
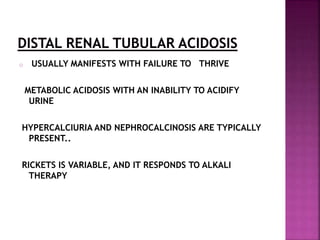
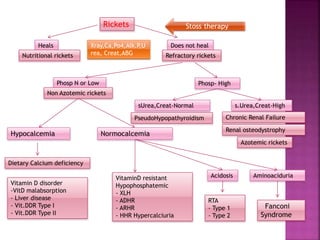
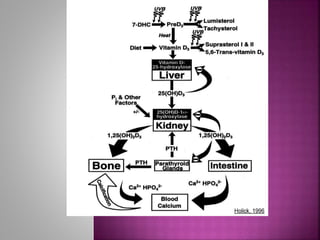
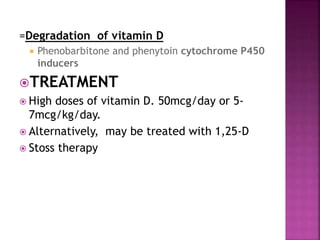
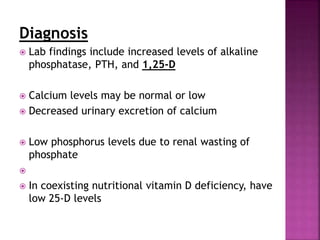
The document discusses rickets and osteomalacia, focusing on their causes, clinical features, diagnosis, and treatment. It highlights the role of vitamin D, calcium, and phosphate in bone mineralization, particularly in children, and outlines risk factors and laboratory findings associated with these deficiencies. Treatment strategies include vitamin D supplementation and dietary adjustments, as well as considerations for rare genetic disorders and their management.



























![ provide adequate calcium, dietary supplement
(doses of 700 [1-3 yr age]m/k/d
1000 (4-8)
1300(>8)
vitamin d supplementation
discouraging early cessation of breast-feeding.
increasing dietary sources of calcium.](https://image.slidesharecdn.com/rickets-150311100553-conversion-gate01/85/Rickets-a-brief-outlook-38-320.jpg)