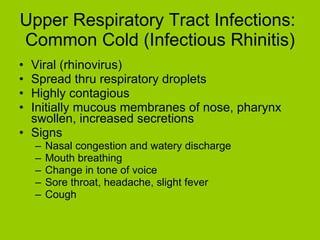
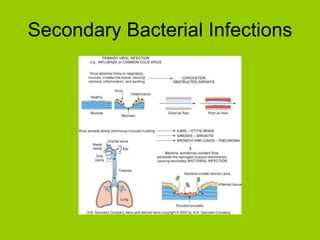
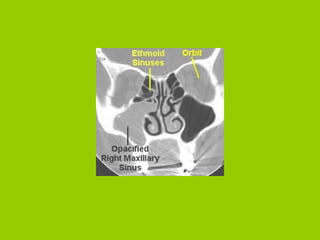
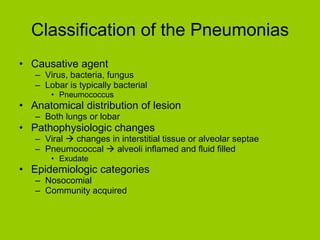
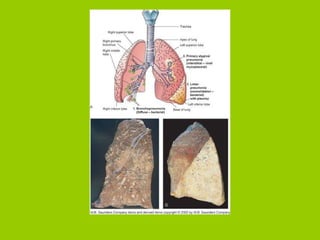
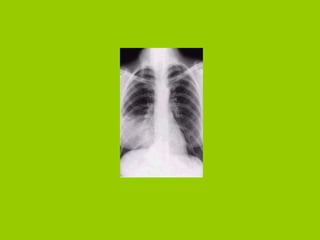
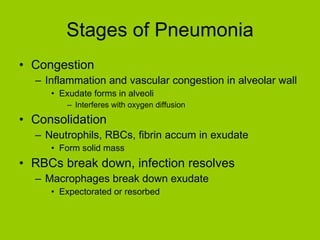
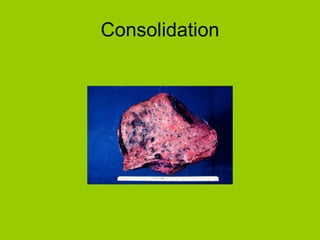
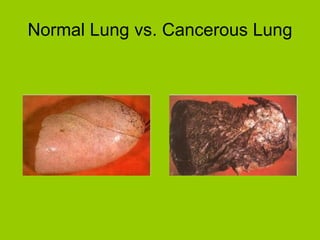
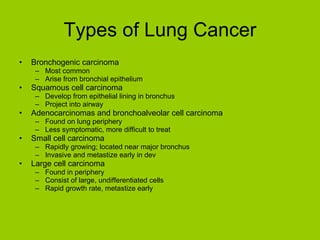
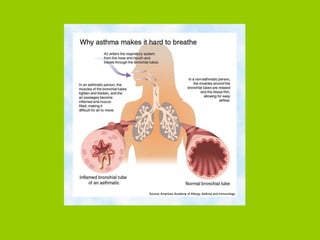
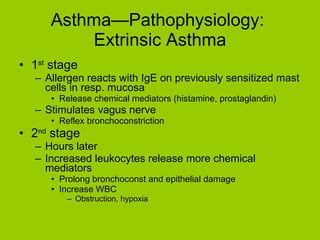
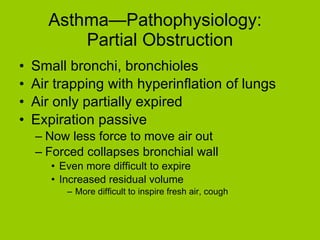
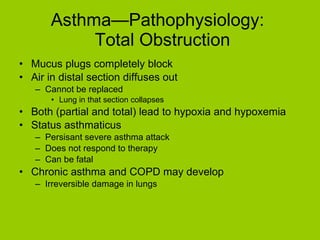
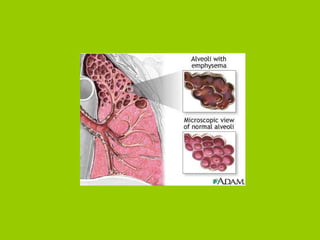
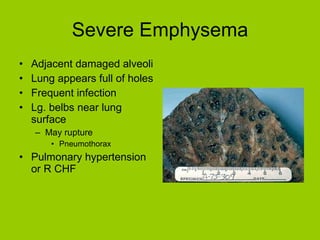
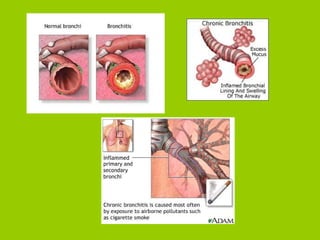
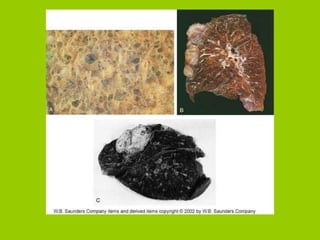
The document provides an overview of respiratory disorders and diseases. It discusses diagnostic tests for respiratory conditions like spirometry and blood gas tests. Common respiratory diseases covered include upper respiratory infections like the common cold, sinusitis, pneumonia, lung cancer, asthma, and chronic obstructive pulmonary disease (COPD). Specific conditions like emphysema and chronic bronchitis are also examined, outlining their pathophysiology, signs and symptoms, diagnosis, and treatment.