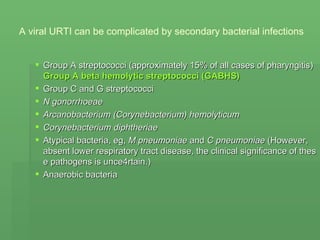
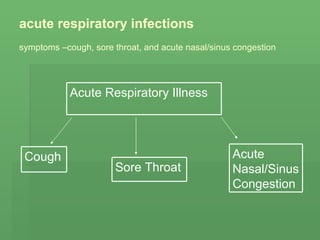
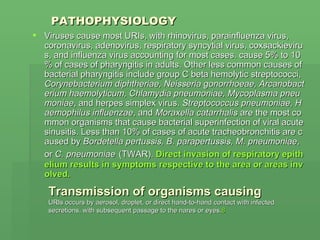
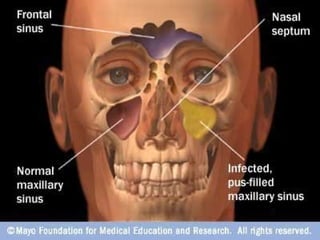
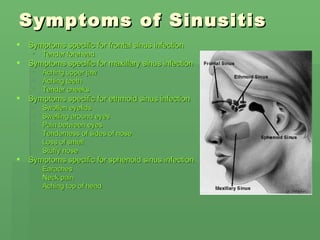
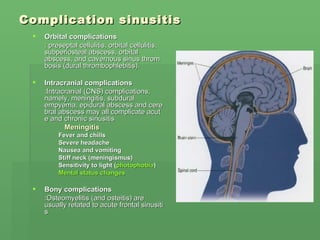
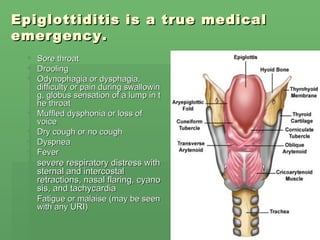
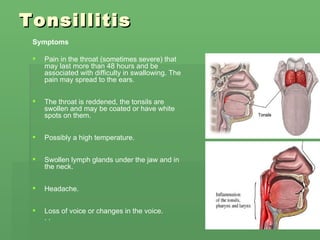
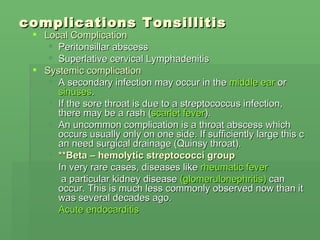
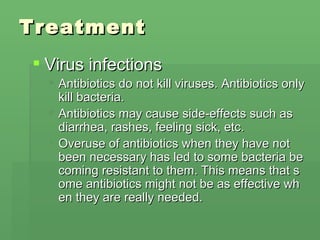
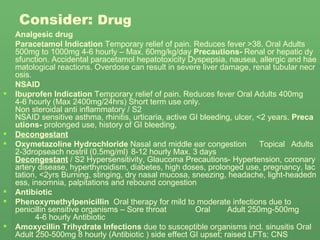
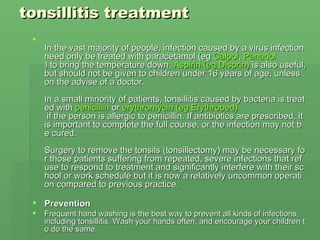
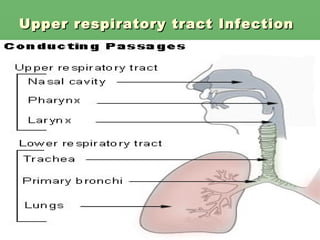
Upper respiratory tract infections are mostly caused by viruses, especially rhinoviruses, coronaviruses, adenoviruses, and influenza viruses. Bacteria can sometimes cause secondary infections. Common symptoms include cough, sore throat, nasal congestion, and sinus pain/pressure. Treatment focuses on relieving symptoms with medications like paracetamol and ibuprofen. Antibiotics are only used if bacteria are confirmed to be causing the infection. Complications can potentially involve the sinuses, ears, or in rare cases, more serious conditions.
![Causes: Most URIs are viral in origin. More than 200 different viruses are known to cause the common cold. Most viral agents that cause Rhinoviruses cause approximately 30-50% of colds in adults. They grow optimally at temperatures near 32.8°C (91°F), which is the temperature inside the human nares. Coronaviruses are a significant cause of colds. However, exact case numbers are difficult to determine, because unlike rhinoviruses, coronaviruses are difficult to culture in the laboratory. Enteroviruses, including coxsackieviruses, echoviruses, and others, are also leading causes of common colds. Adenoviruses , orthomyxoviruses (including influenza A and B viruses), paramyxoviruses (eg, parainfluenza [PIV]), RSV, EBV, and hMPV account for many URIs. Varicella, rubella, and rubeola infections may manifest as a nasopharyngitis before other classic signs and symptoms](https://image.slidesharecdn.com/upperrespiratorytractinfection-091130204516-phpapp01/85/Upper-Respiratory-Tract-Infection-3-320.jpg)