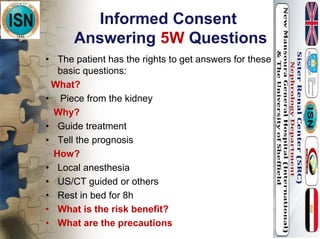
Renal biopsy is a procedure used to obtain a small piece of kidney tissue to examine under a microscope in order to diagnose the specific cause of kidney disease or damage. Some key points:
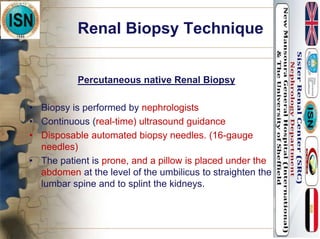
- Renal biopsy has been performed since the 1930s and modern techniques now use real-time ultrasound guidance.
- Indications for renal biopsy include nephrotic syndrome, acute kidney injury, unexplained chronic kidney disease, and renal transplant dysfunction.
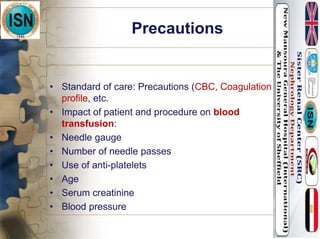
- Complications can include bleeding, but are usually minor. The patient must follow post-biopsy monitoring and restrictions like bed rest to reduce risks.