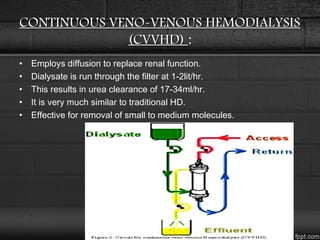
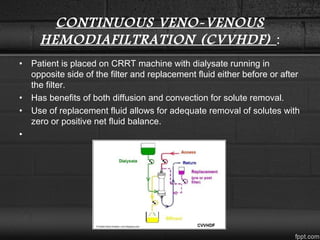
Renal replacement therapy encompasses life-supporting treatments for renal failure such as hemodialysis, peritoneal dialysis, and continuous renal replacement therapy. Hemodialysis uses diffusion and filtration across a semi-permeable membrane to remove waste and fluid. Peritoneal dialysis infuses dialysate into the peritoneal cavity. Continuous renal replacement therapy provides 24-hour treatment through diffusion, convection, or a combination. These therapies aim to replace normal kidney functions of waste removal and fluid balance.