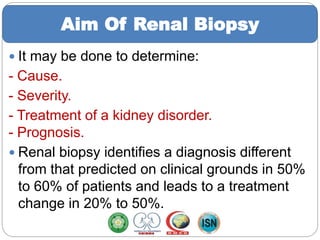
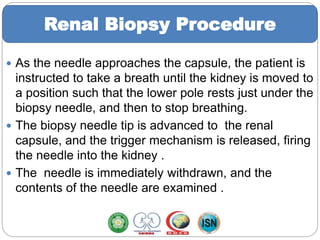
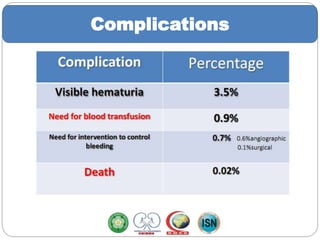
This document discusses renal biopsy procedures. It begins with definitions and history of renal biopsies. The aim is to determine the cause, severity, and treatment of kidney disorders and the procedure provides a diagnosis in over 95% of cases. Indications include nephrotic syndrome, atypical nephrotic features in children, acute or progressive renal failure, and transplant dysfunction. Contraindications include refusal, bleeding disorders, infections, and anatomical abnormalities. The procedure involves ultrasound-guided collection of tissue samples for analysis. Patients are monitored afterwards for pain and bleeding complications, which are usually minor.