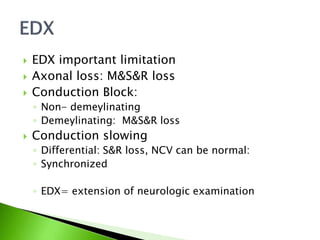
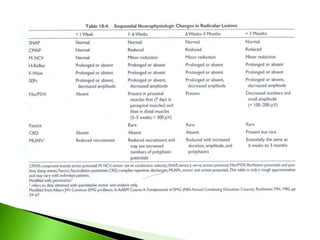
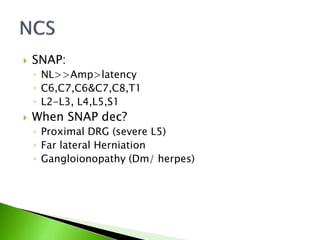
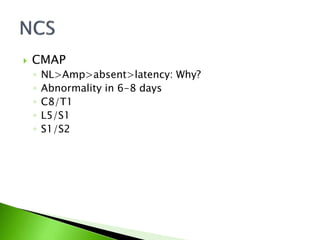
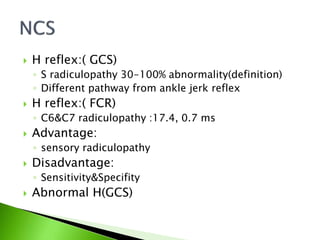
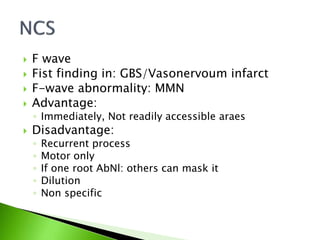
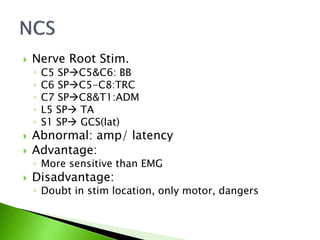
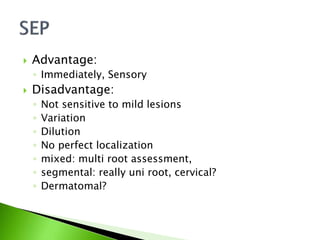
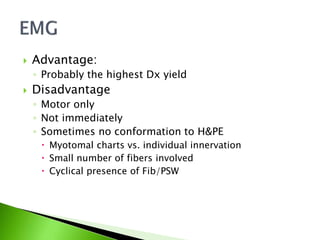
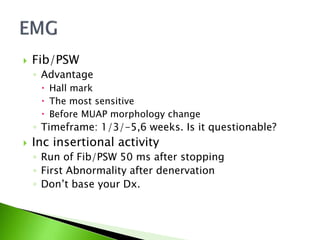
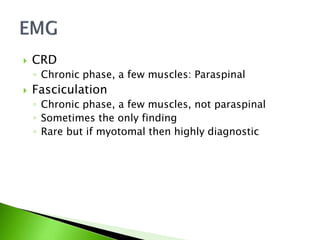
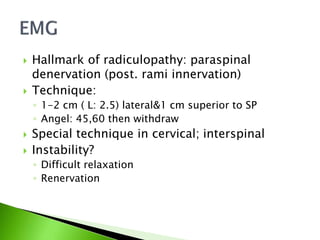
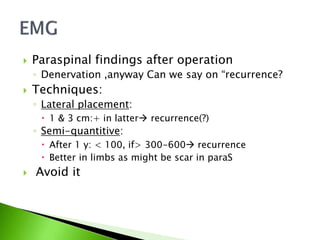
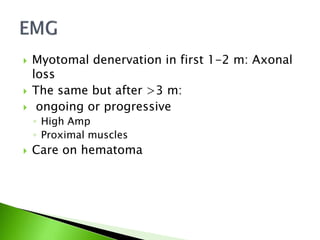
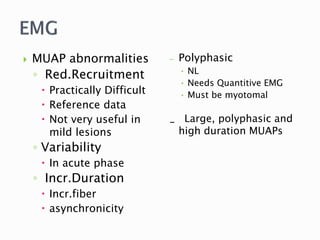
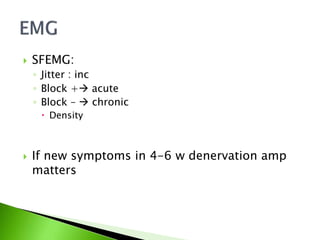
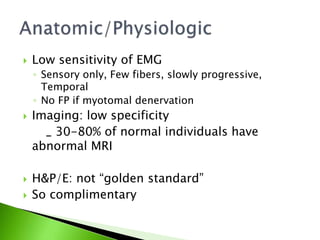
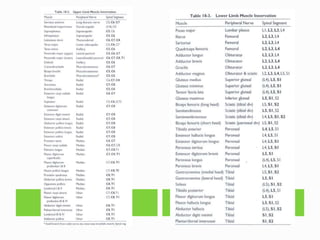
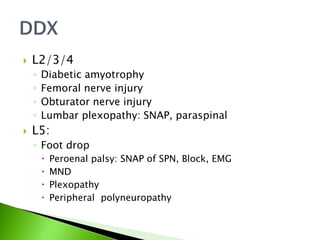
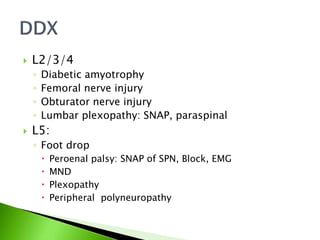
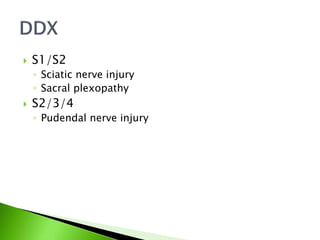
This document discusses electrodiagnostic techniques for evaluating radiculopathy. It covers nerve conduction studies including SNAPs, CMaps, H-reflexes and F-waves. It also discusses needle EMG findings including fibrillations, positive sharp waves and complex repetitive discharges. The advantages and disadvantages of each technique are provided for assessing different nerve roots involved in radiculopathy.