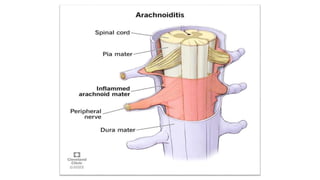
Arachnoiditis is a chronic pain disorder caused by inflammation of the arachnoid membrane surrounding the spinal cord and nerves. Symptoms vary but commonly include severe shooting or electric shock-like pain. It is often caused by complications from spinal surgery or lumbar punctures. Diagnosis involves MRI, CT myelogram, or lumbar puncture to identify signs of nerve thickening or clumping. While there is no cure, treatment focuses on pain management through medications, hydrotherapy, massage, and range of motion exercises to improve quality of life.