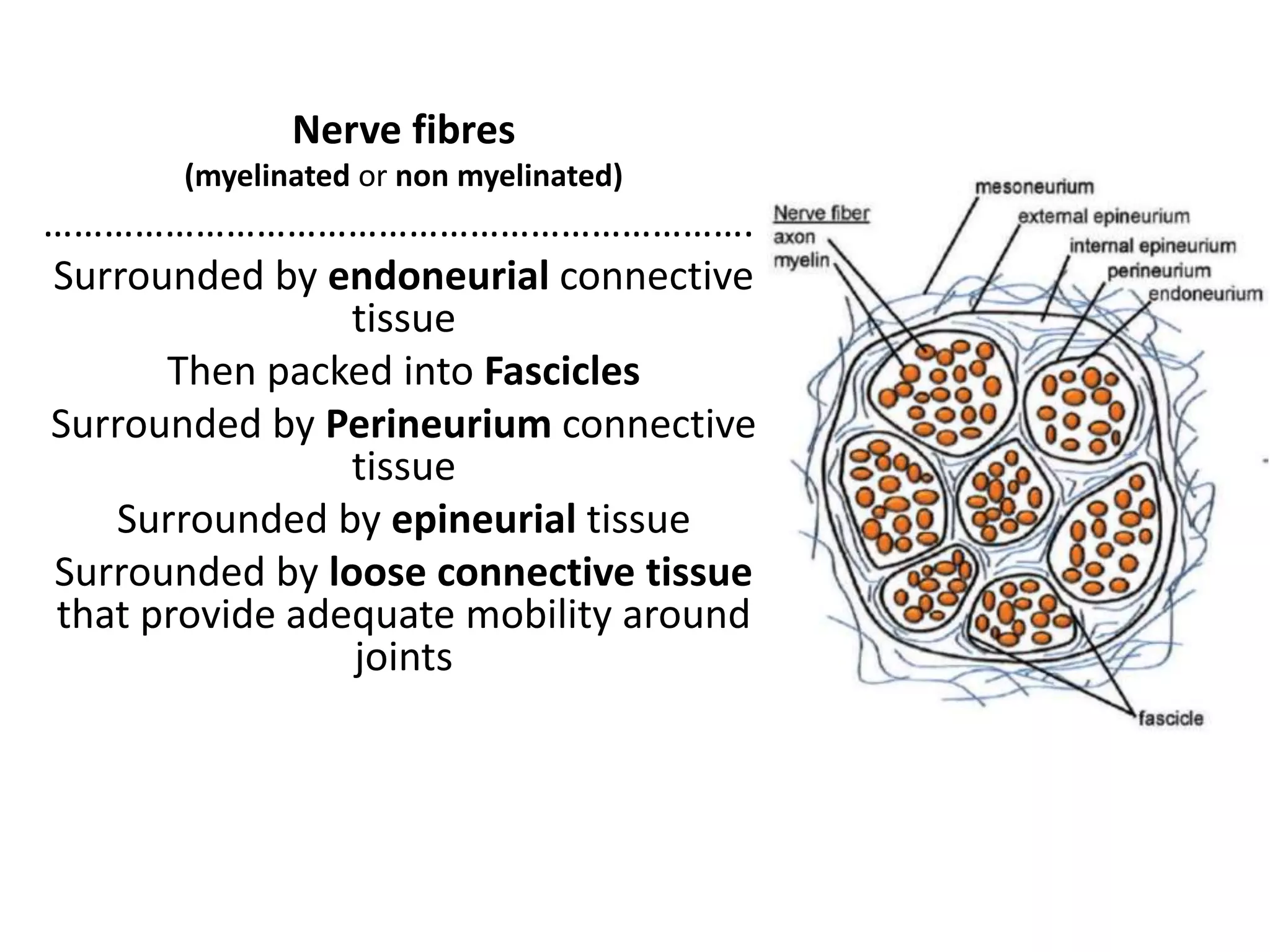
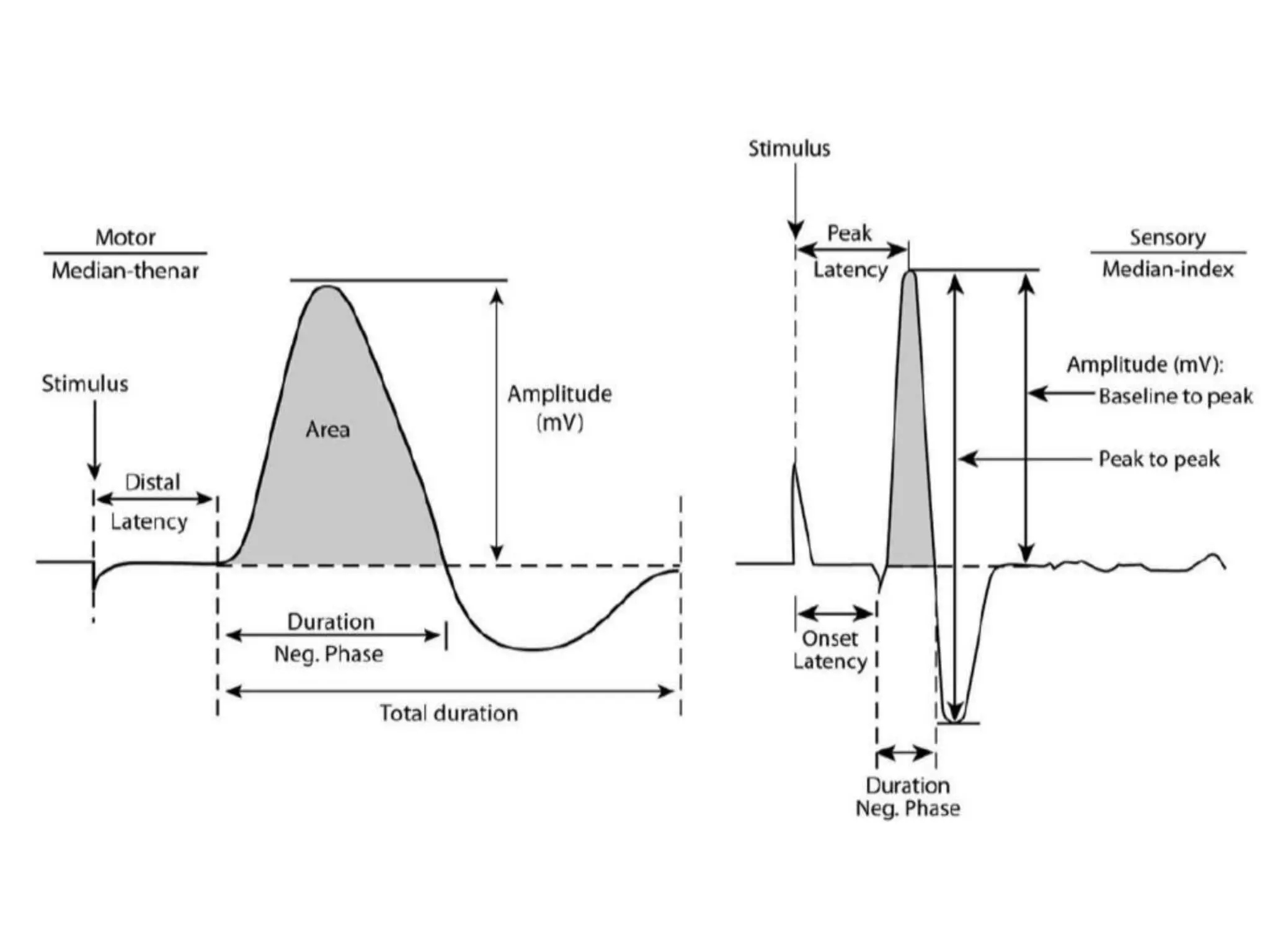
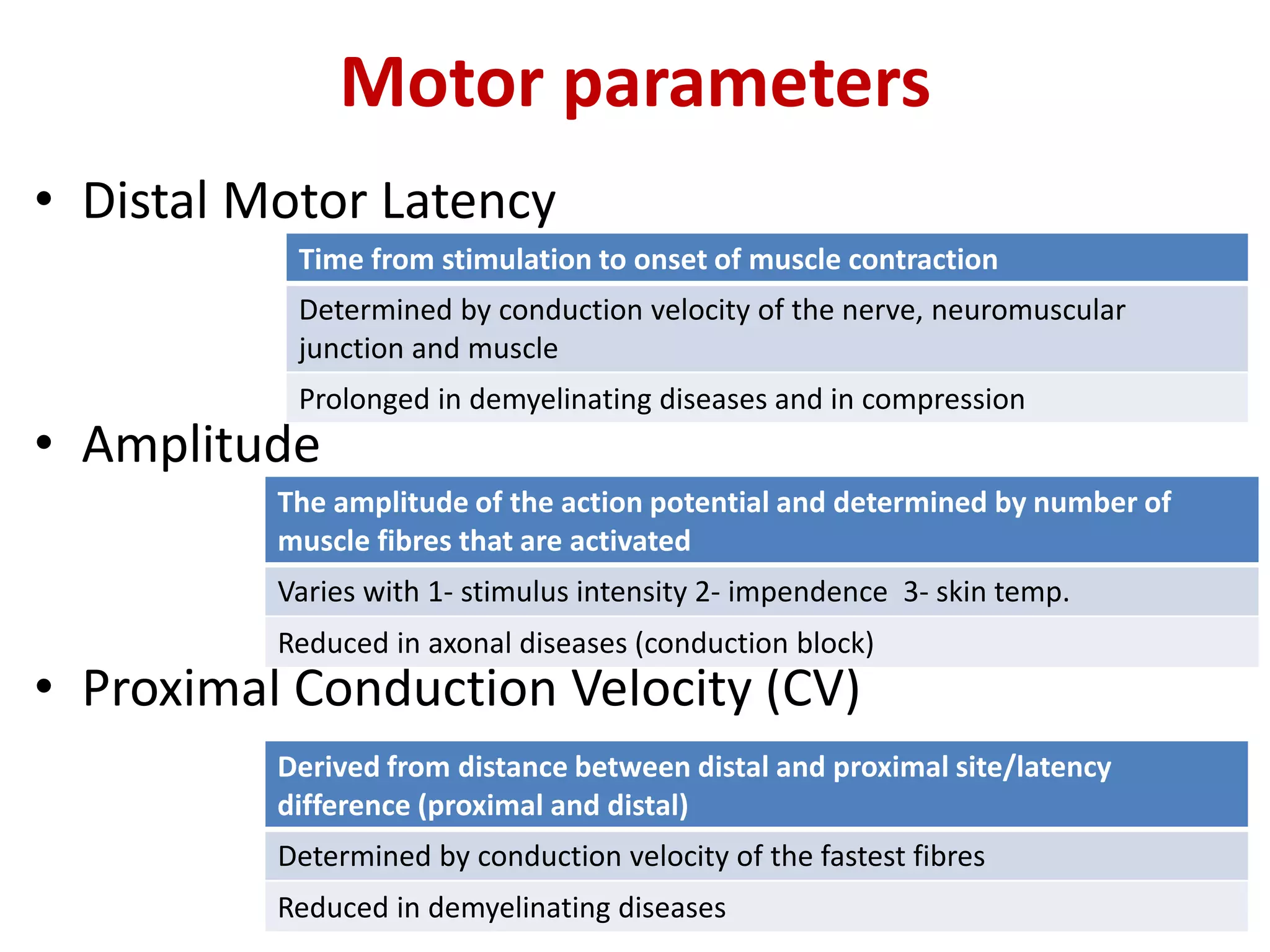
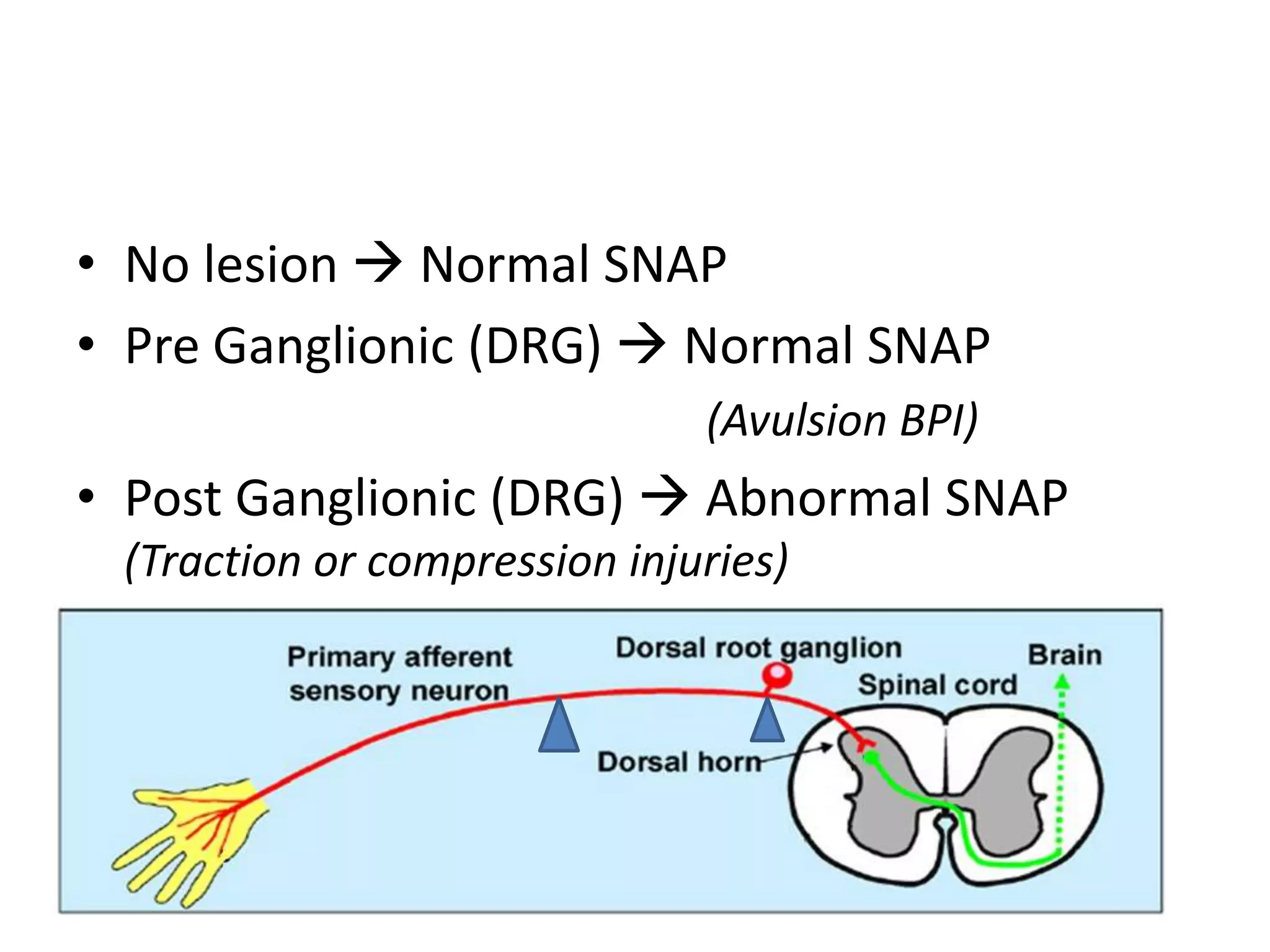
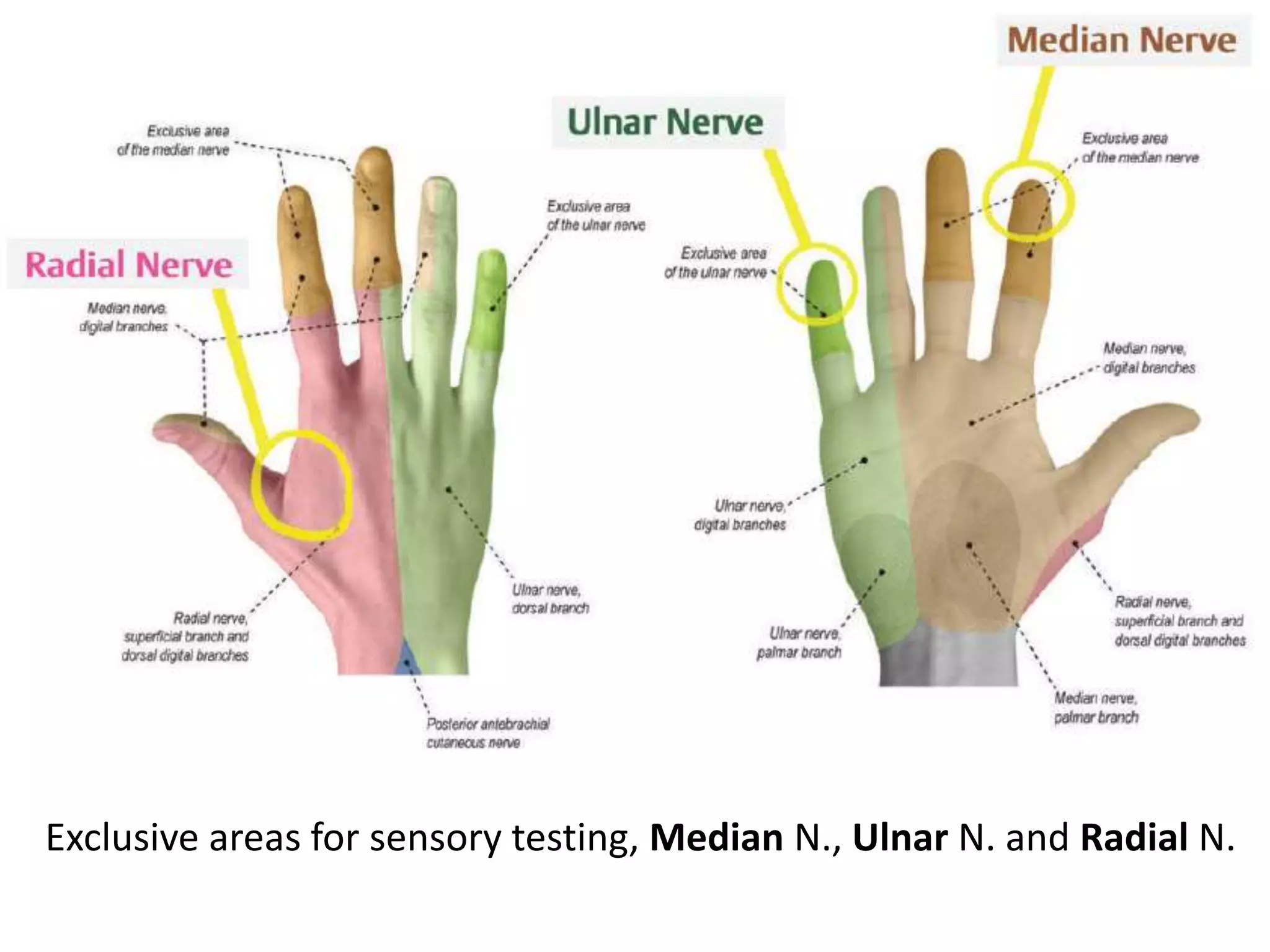
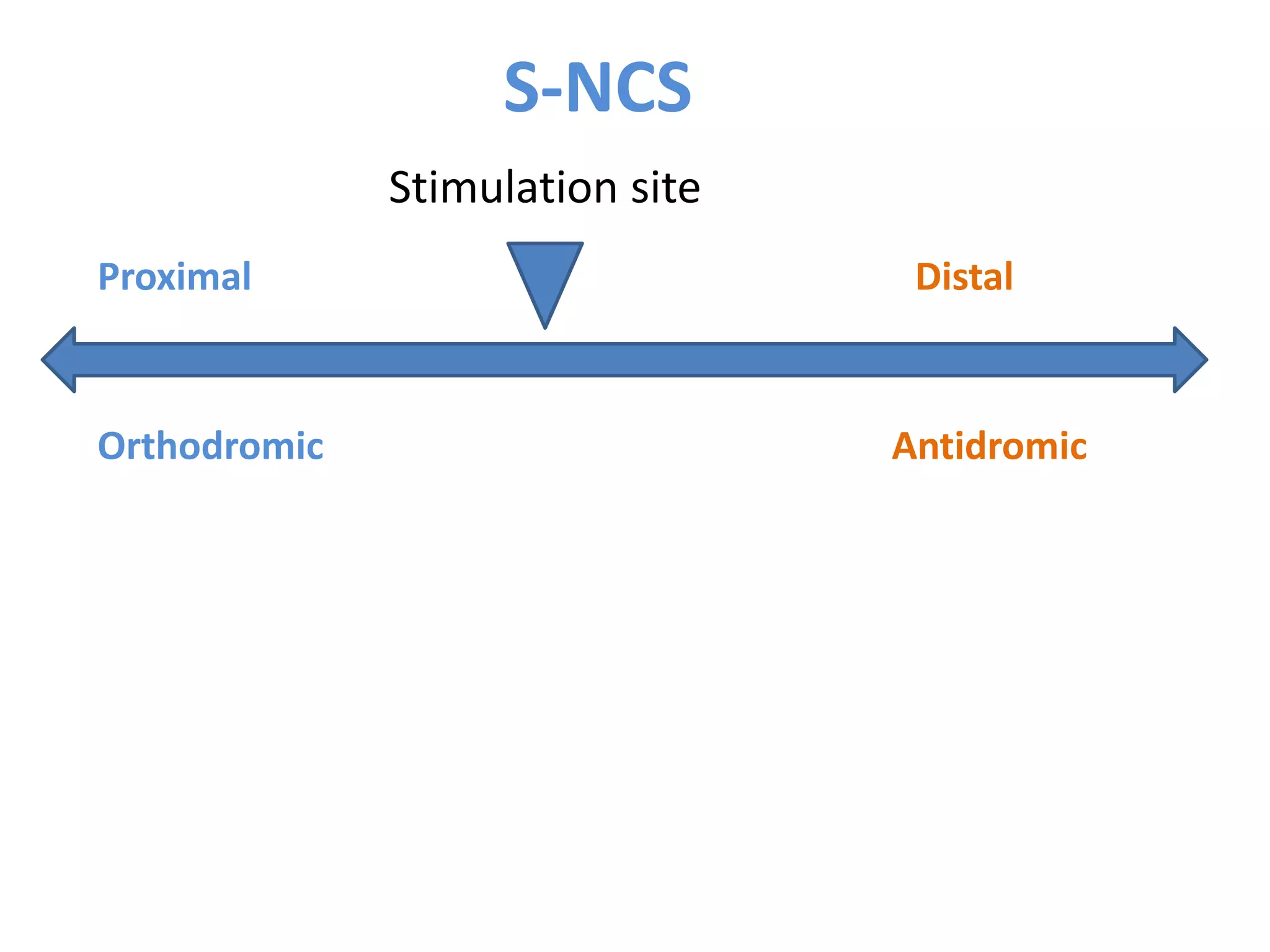
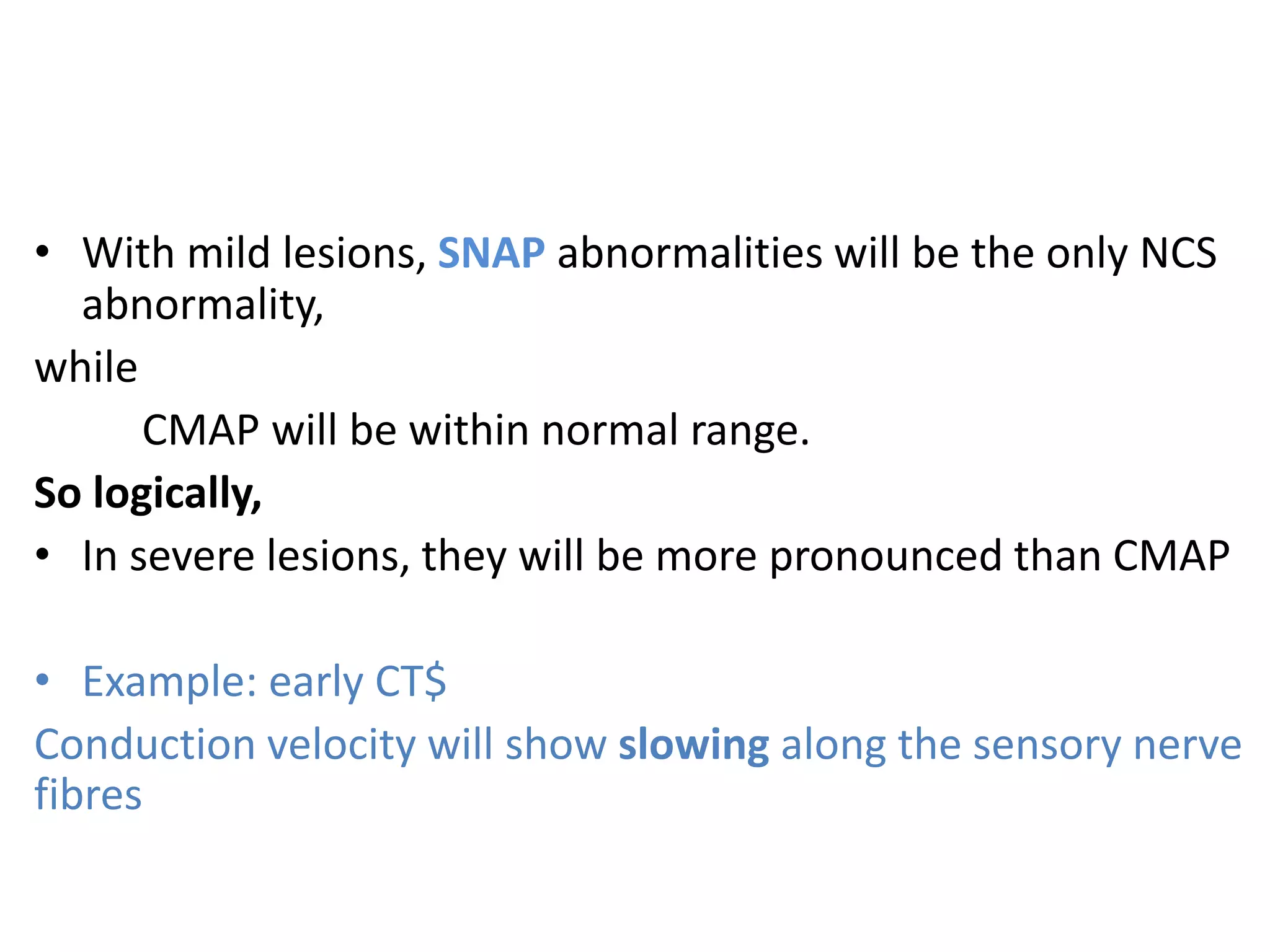
The document provides an in-depth overview of nerve conduction velocity (NCV) and electromyography (EMG) as diagnostic tools in neurosurgery, detailing their methodology, interpretations, and clinical relevance. It discusses the anatomy of the nervous system, types of nerve injuries, and the significance of various electrical responses during testing. The limitations of these techniques and their implications for diagnosing peripheral nerve disorders are also highlighted.