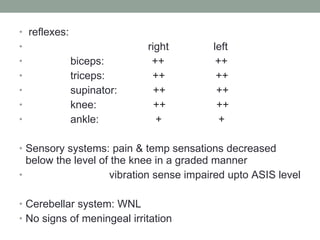
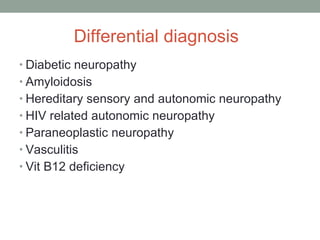
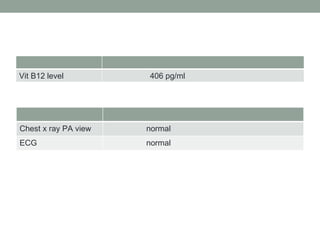
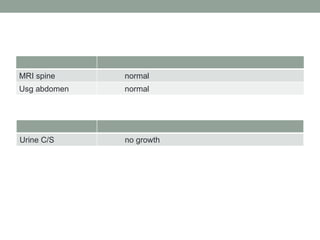
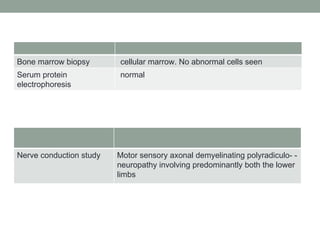
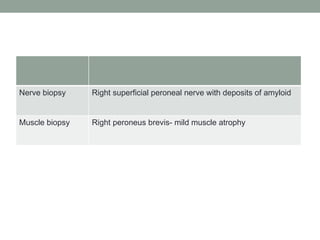
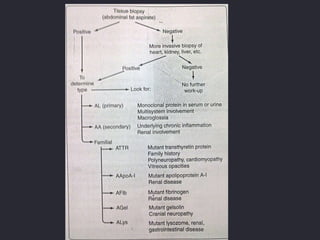
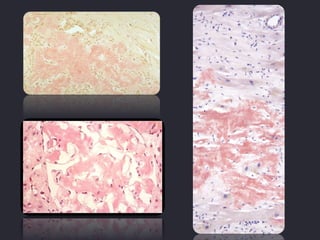
A 41-year-old male presented with numbness in both lower limbs for 1.5 years and urinary retention for 6 months. Nerve conduction studies showed axonal demyelinating polyradiculoneuropathy predominantly in the lower limbs. Biopsy of the right superficial peroneal nerve showed amyloid deposits. The diagnosis was amyloid polyradiculoneuropathy, likely familial. Liver transplantation can eliminate the variant transthyretin protein produced in the liver and halt progression of neuropathy in many cases, but outcomes depend on the specific mutation and disease severity at time of transplant.
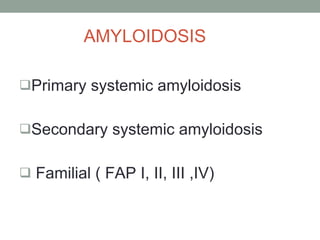

![Presse Med. 2010 Jan;39(1):17-25. Epub 2009 May 5. [Liver transplantation for familial amyloid polyneuropathy]. [Article in French] Adams D , Slama M , Samuel D . Liver transplantation has been proposed as a treatment for FAP because the liver is the main source of variant amyloidogenic TTR. Transplantation makes it possible to eliminate 98% of the variant TTR in the serum, doubles median survival for variant TTRMet30 carriers, and halts the progress of the sensorimotor neuropathy over the long term in 62% of cases. No regression or recurrence has been observed. Poor prognostic factors after liver transplantation are a mutation other than the TTRMet30 variant, severe neuropathy, and late onset. Liver transplantation must be proposed to the symptomatic patients as early as possible](https://image.slidesharecdn.com/acaseofperipheralneuropathy-110214052442-phpapp01/85/A-Case-of-Peripheral-Neuropathy-33-320.jpg)