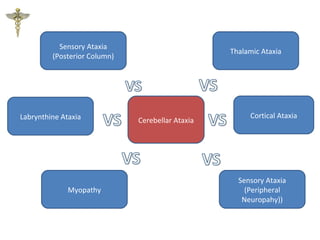
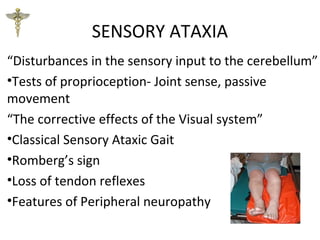
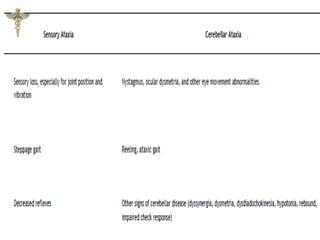
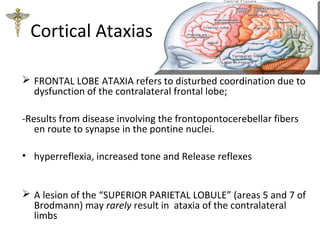
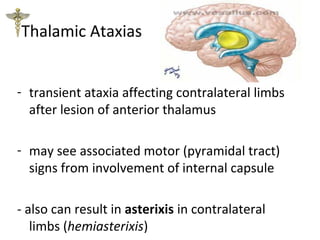
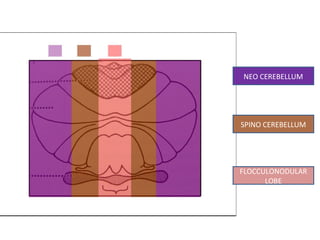
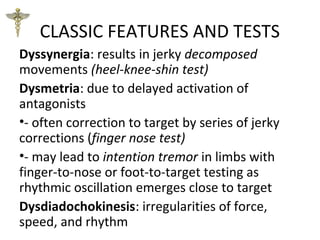
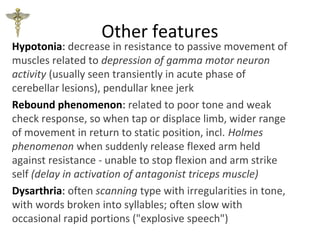
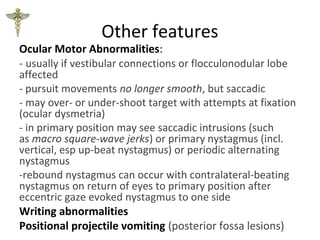
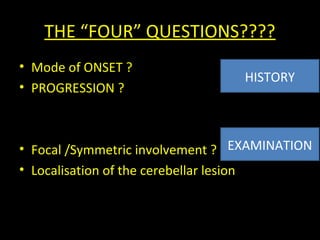
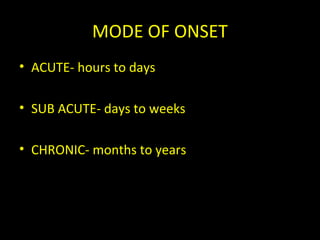
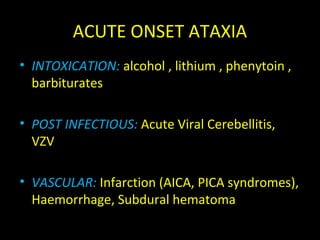
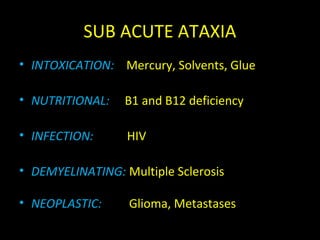
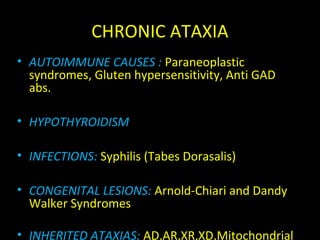
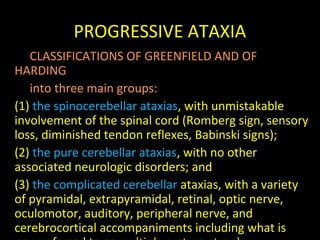
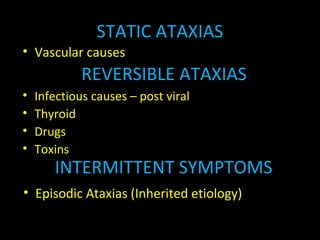
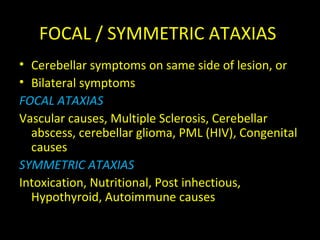
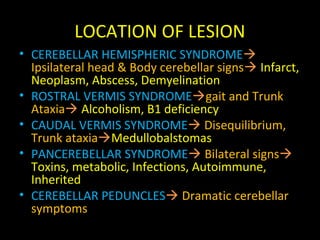
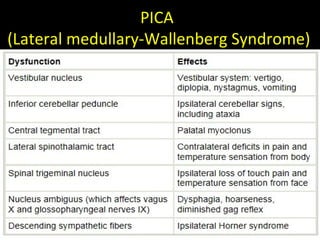
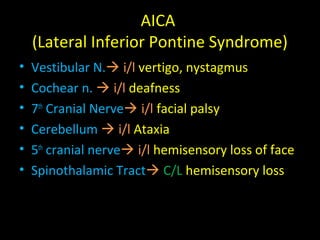
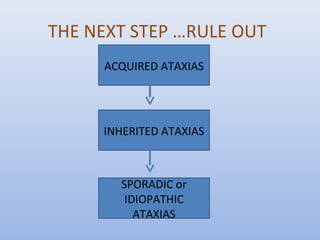
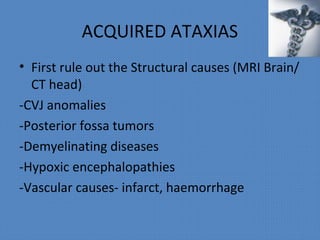
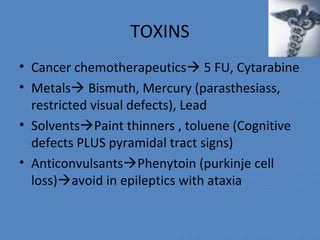
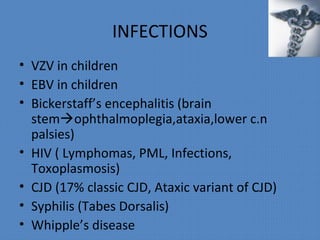
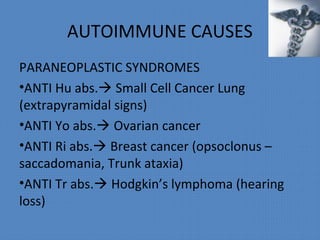
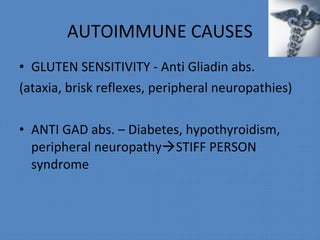
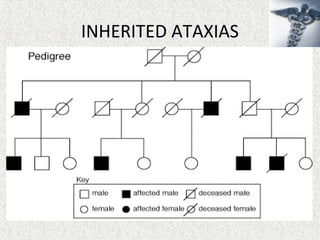
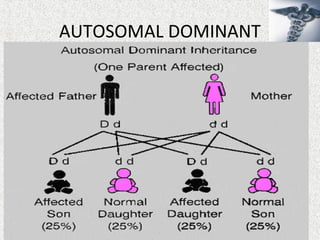
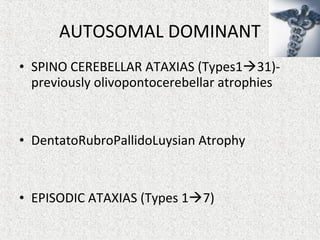
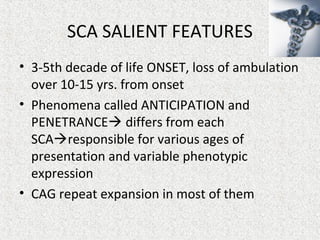
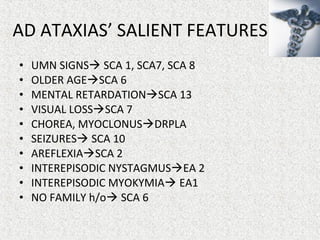
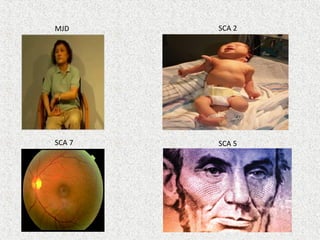
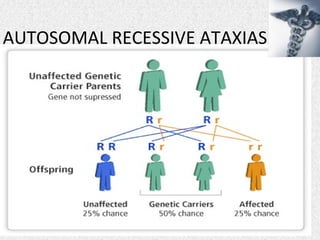
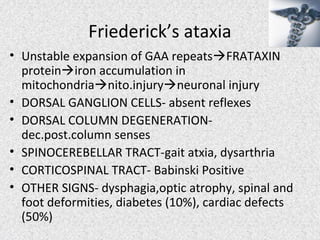
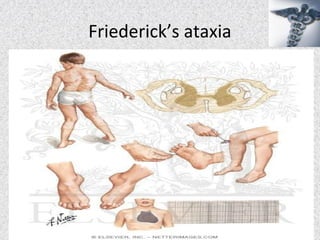
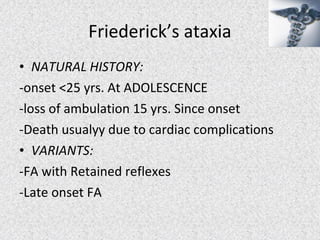
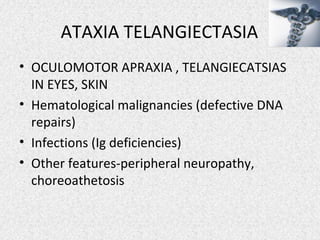
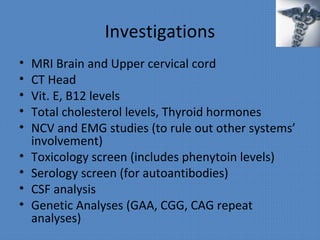
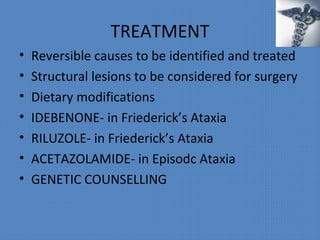
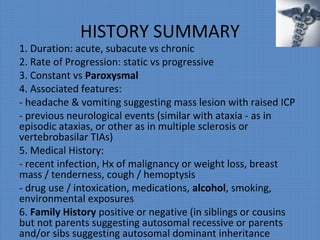
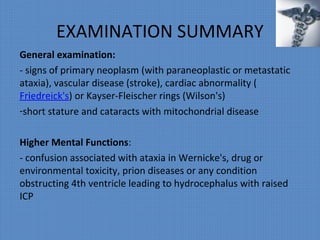
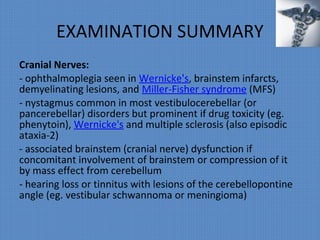
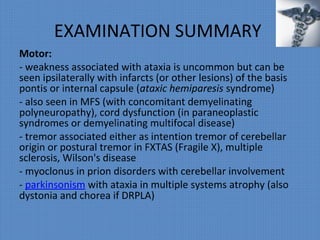
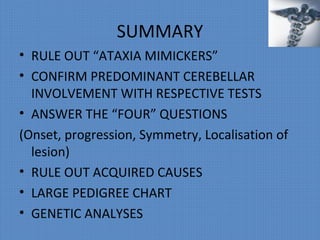
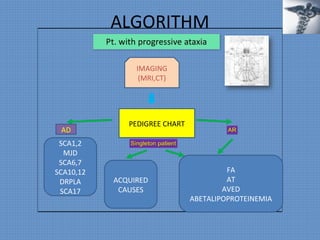
This document provides an overview of the approach to evaluating and diagnosing ataxia. It begins with definitions of ataxia and discusses tests to differentiate various systems that can cause ataxia-mimicking symptoms. It then covers approaches to evaluating cerebellar ataxia, including assessing mode of onset, progression, focal vs symmetric involvement, and localizing the lesion. Common etiologies of acquired, inherited, autosomal dominant and recessive ataxias are summarized. The document provides a step-wise algorithm for evaluating and categorizing ataxia.