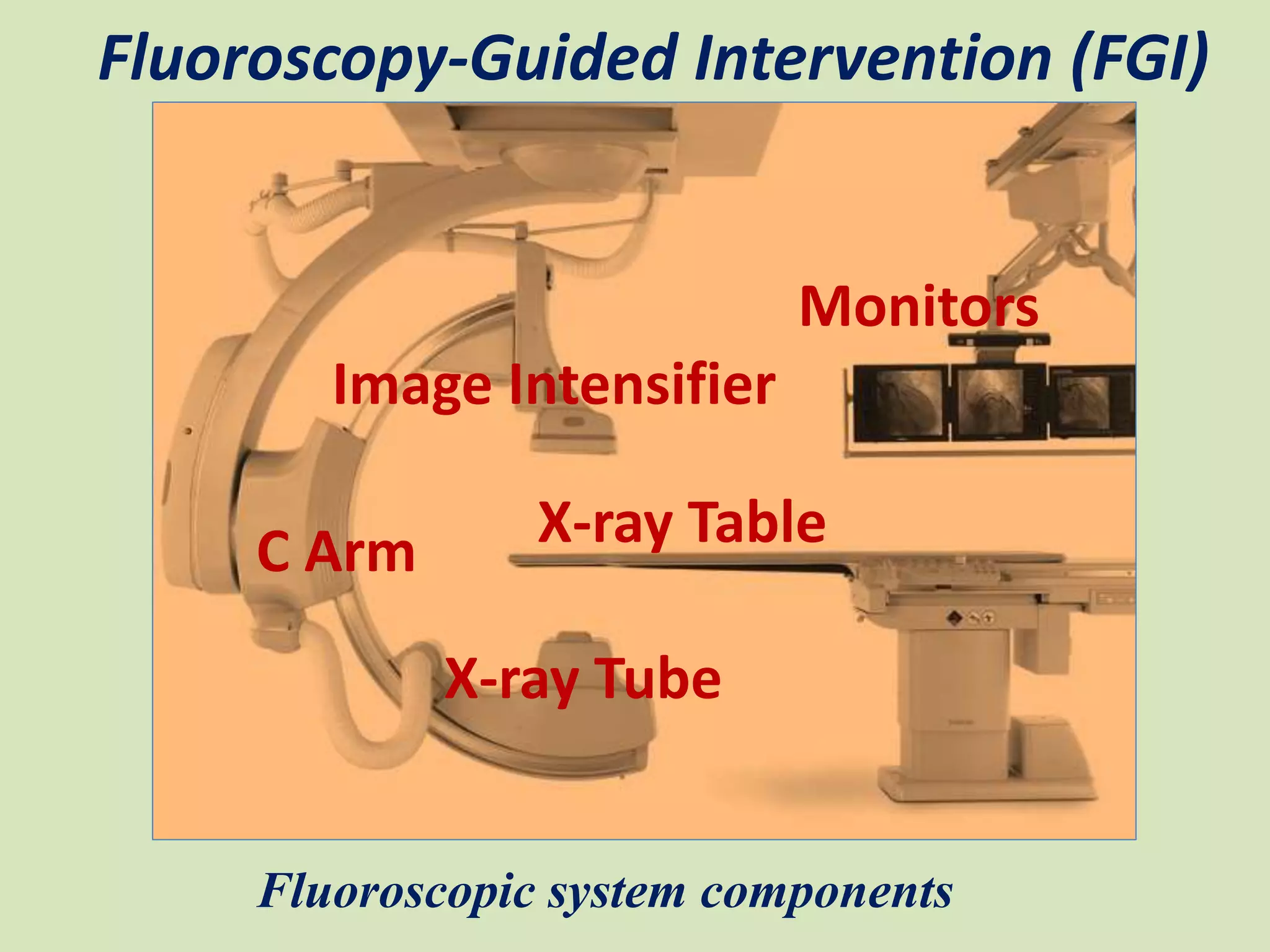
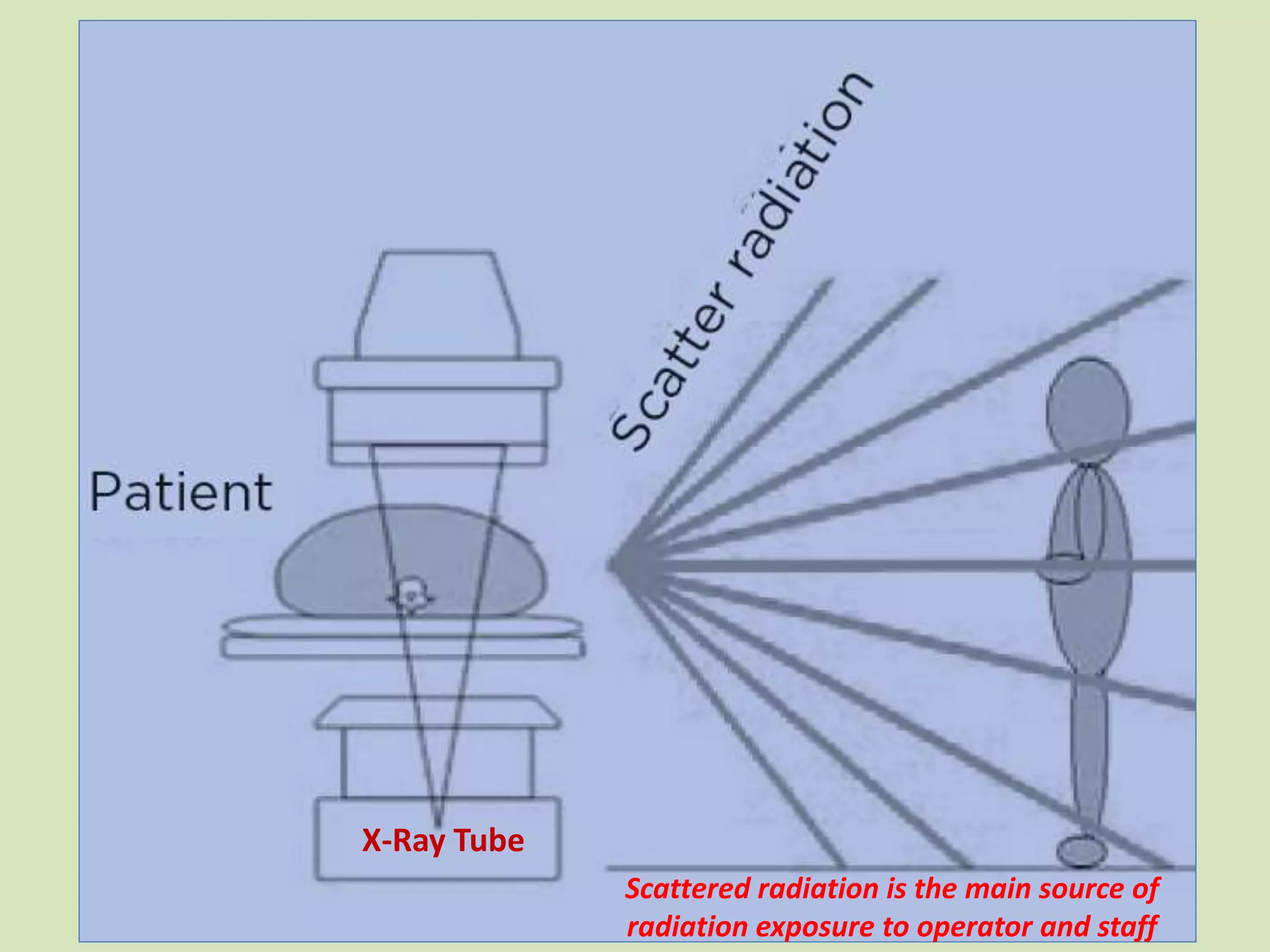
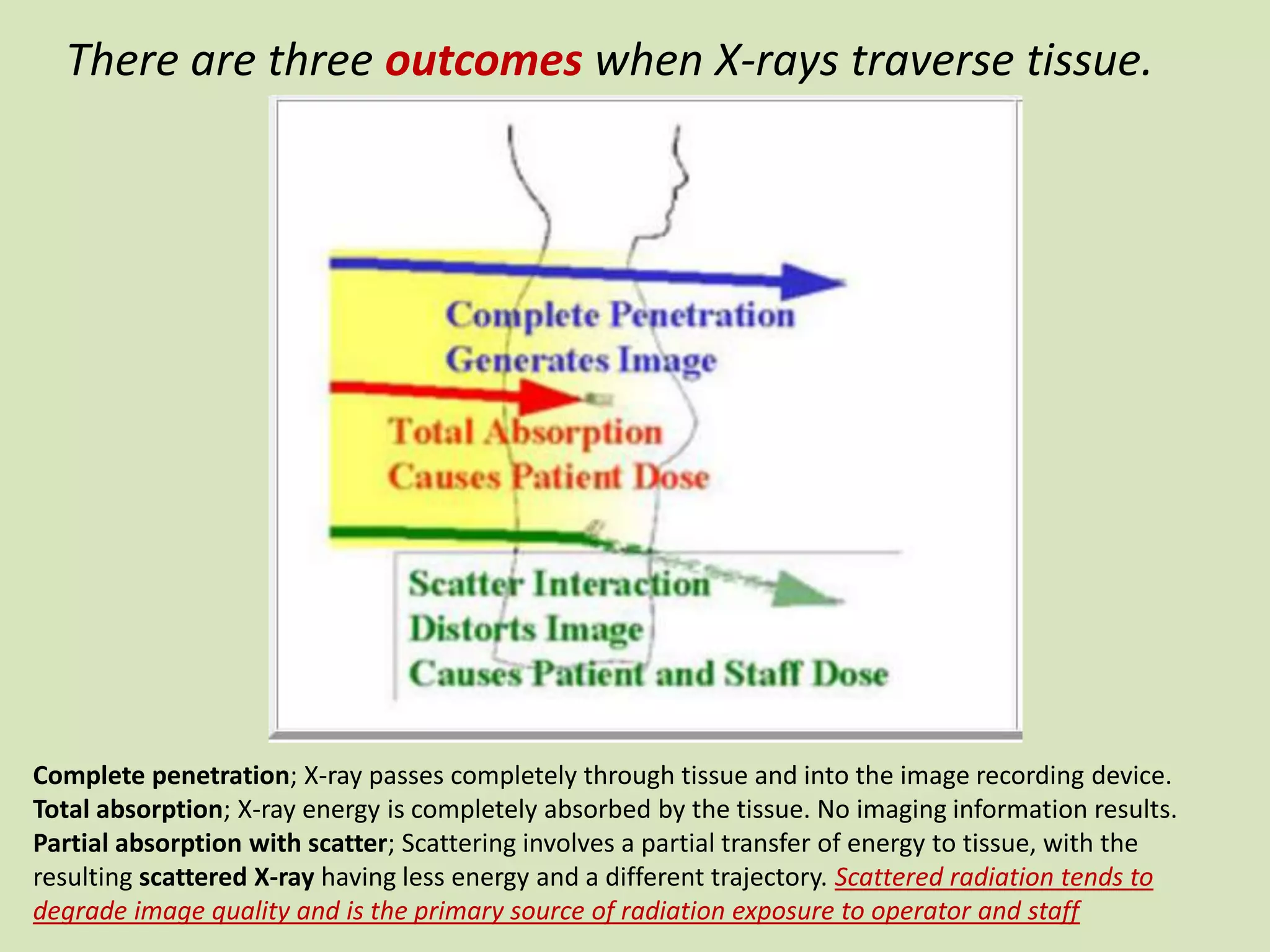
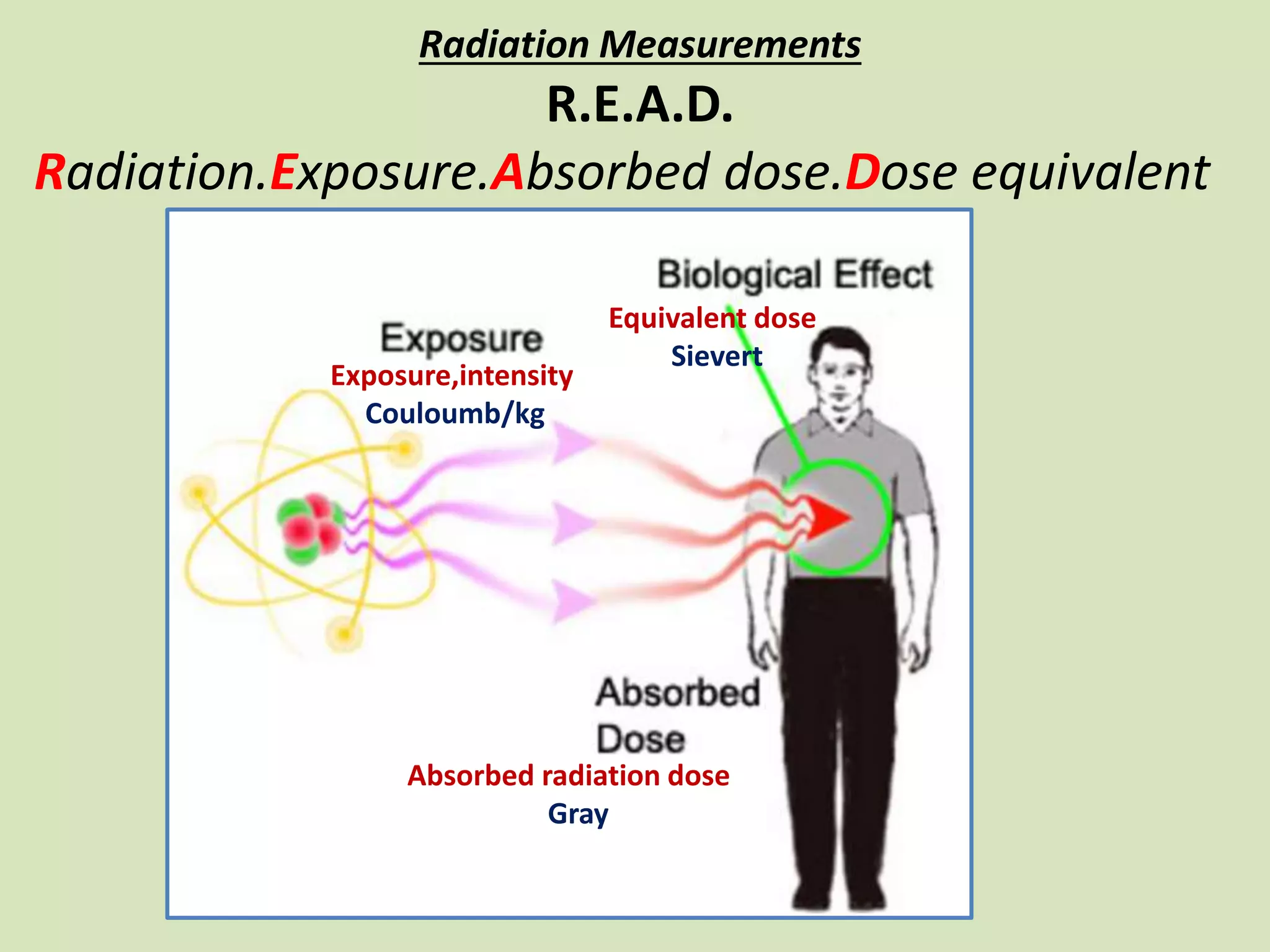
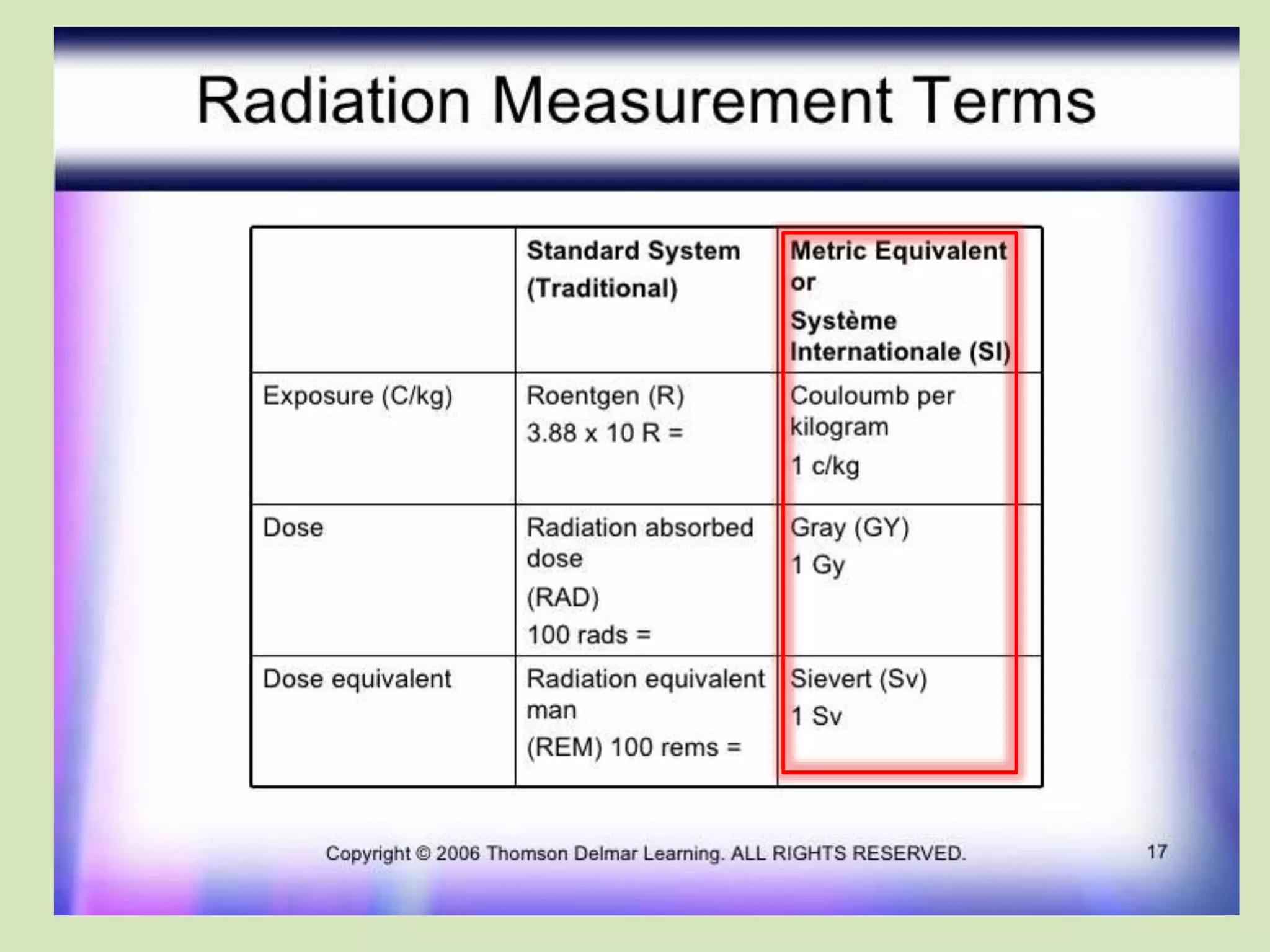
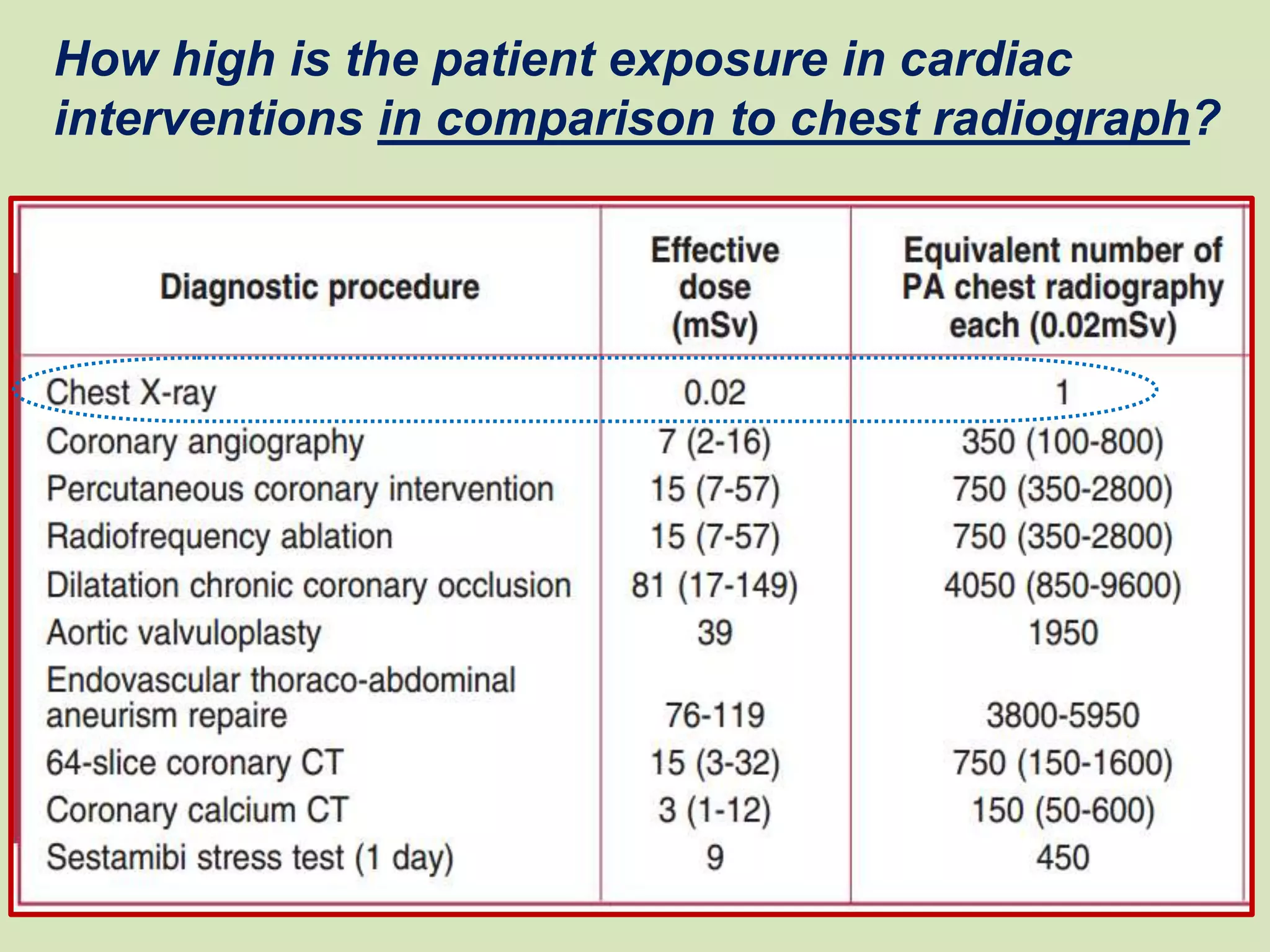
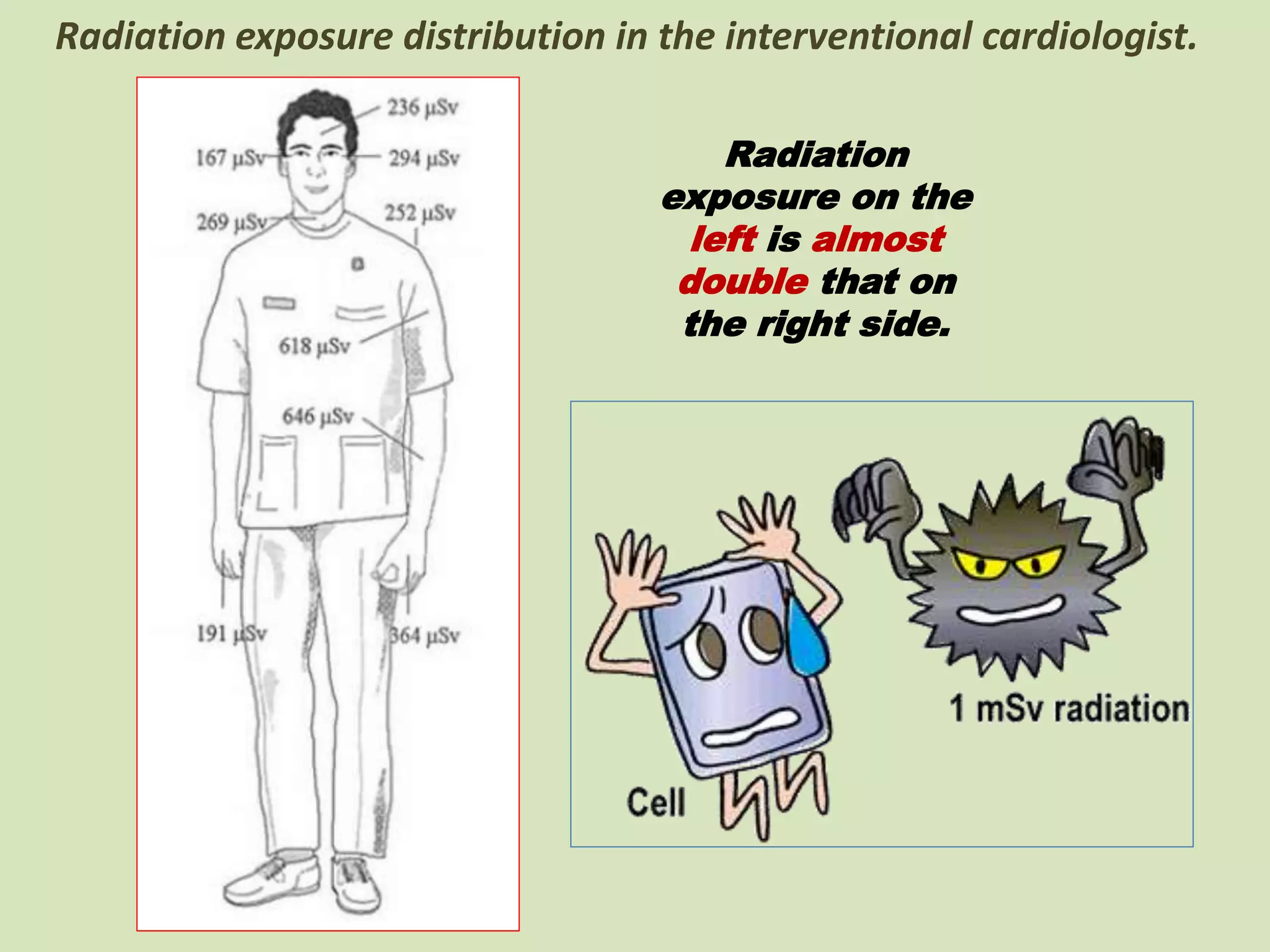
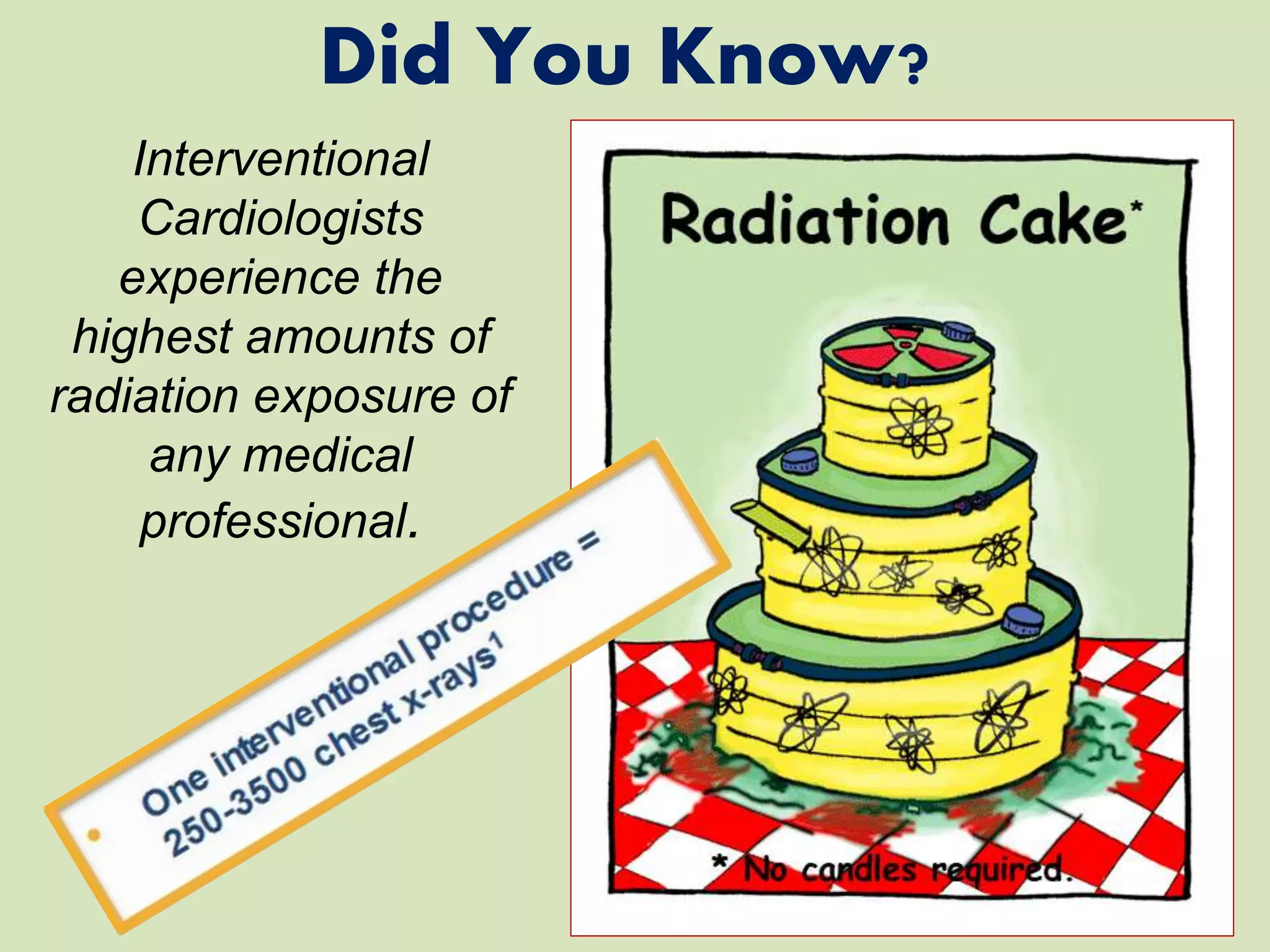
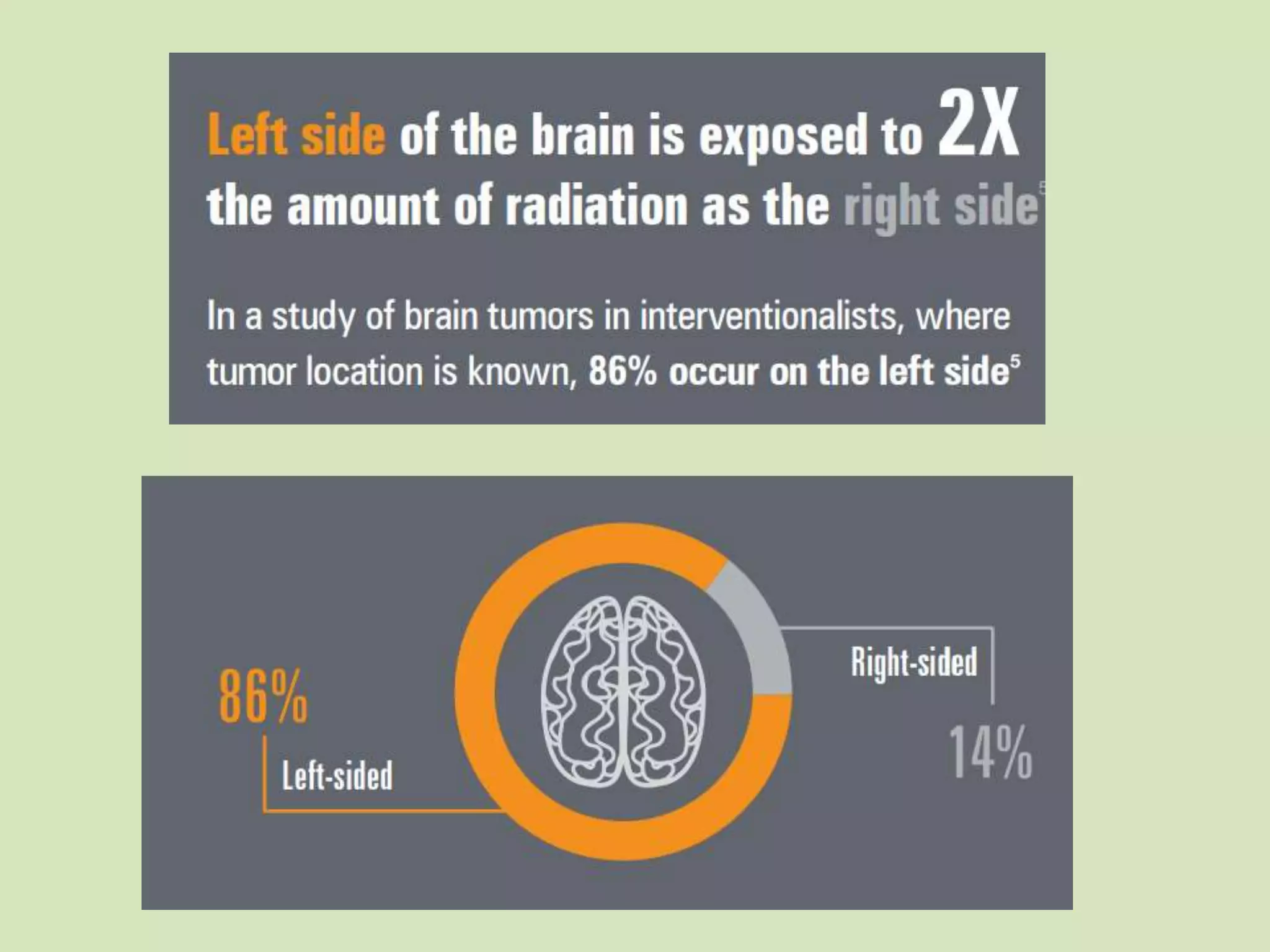
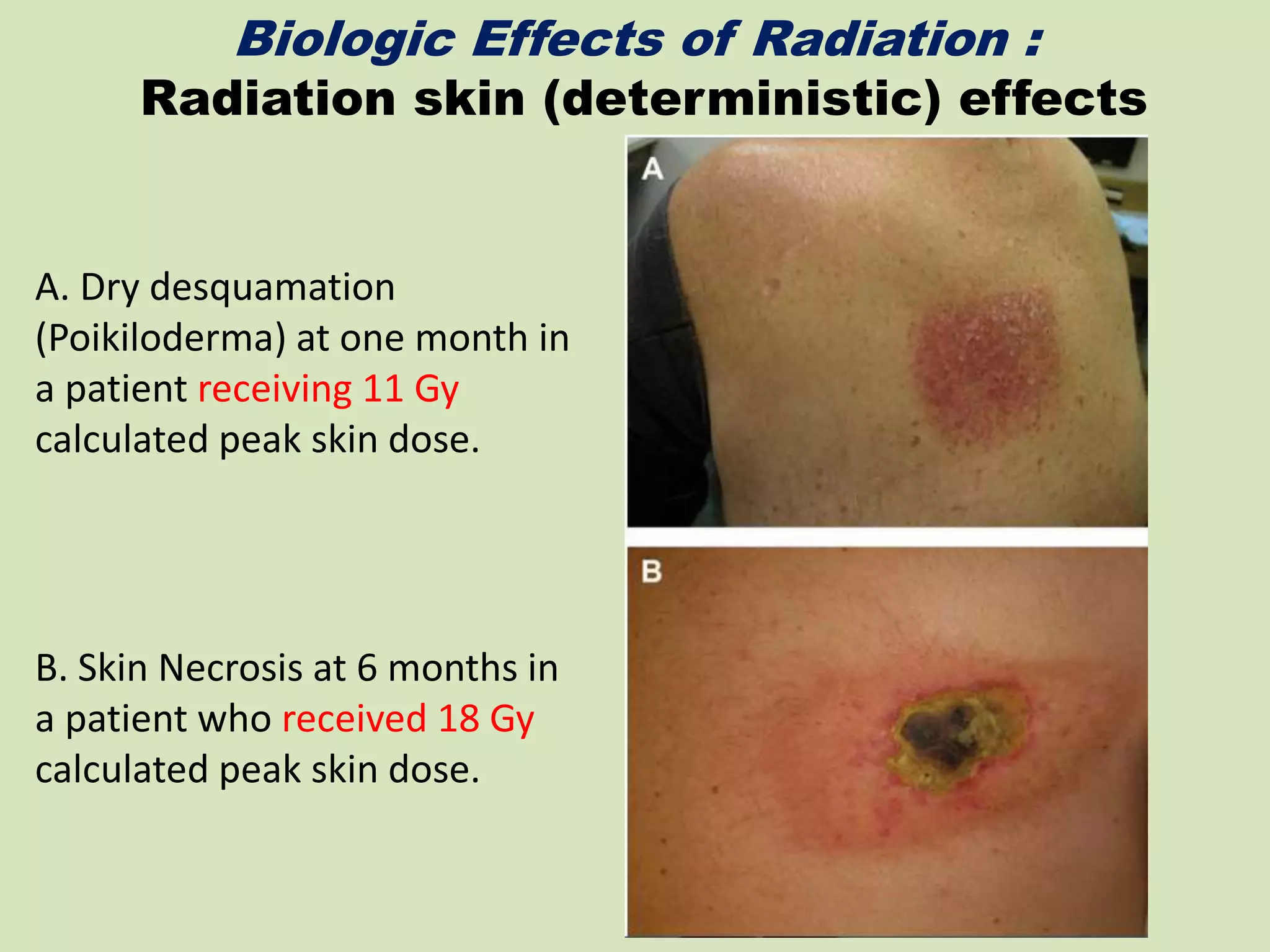
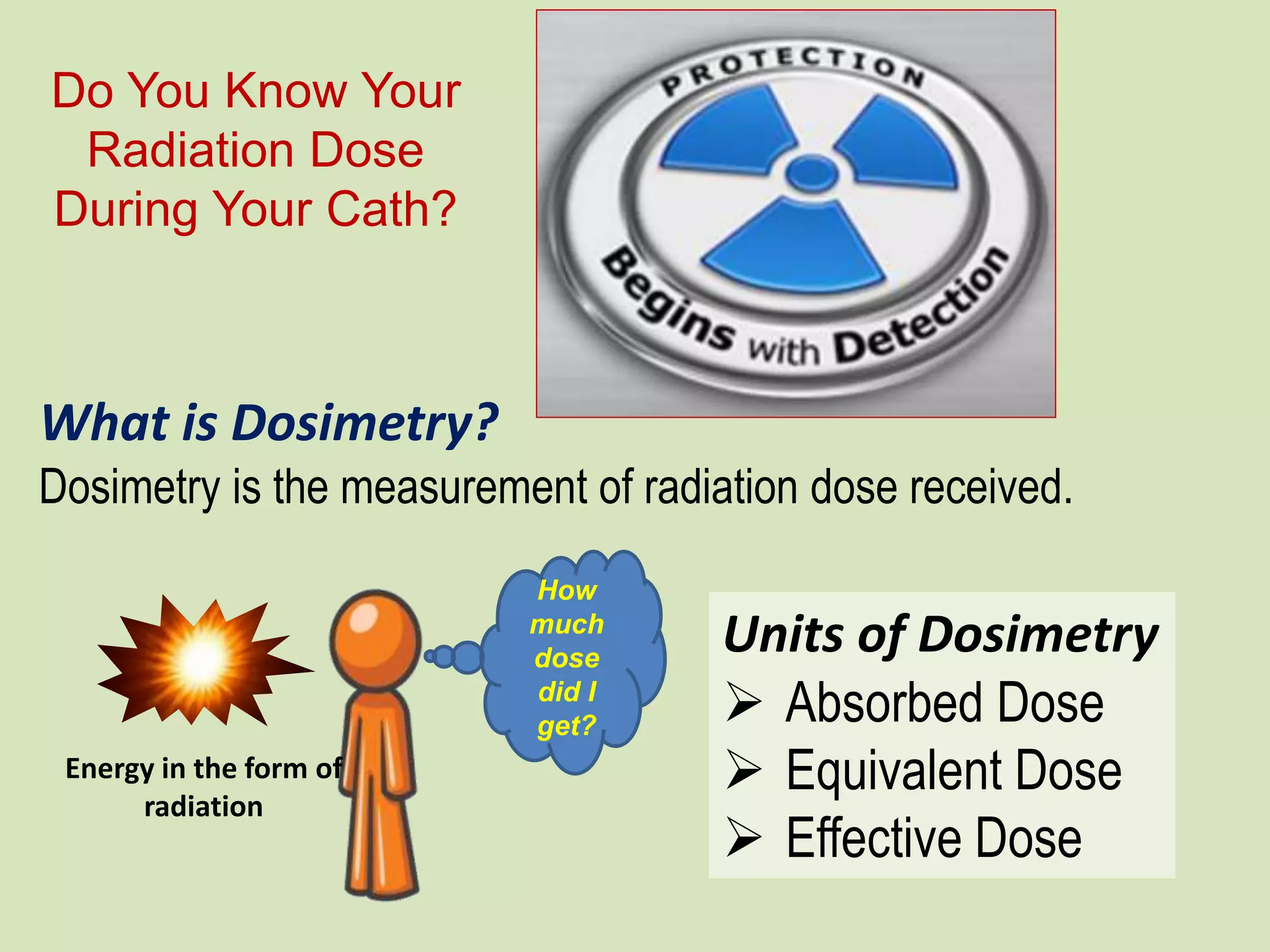
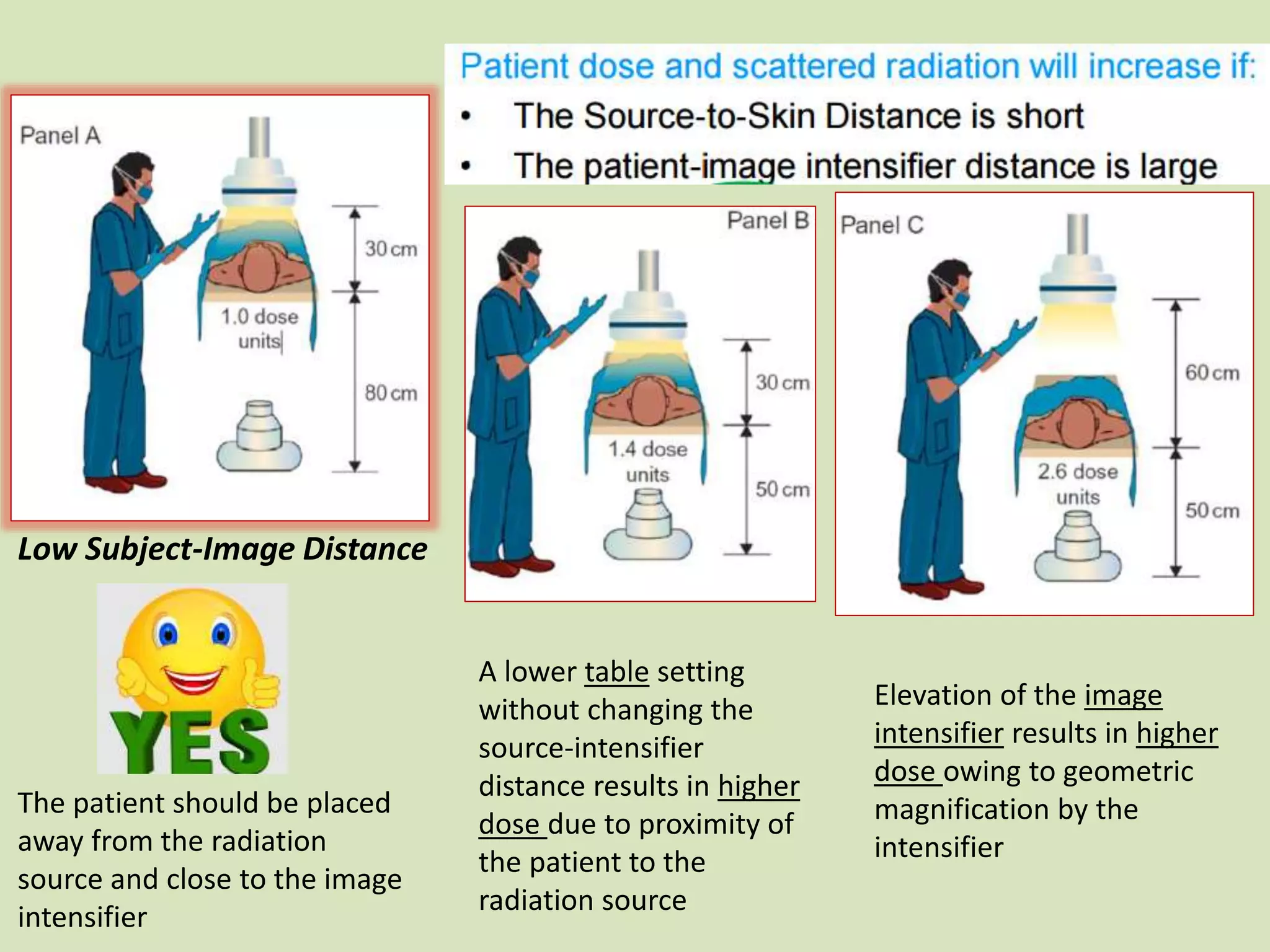
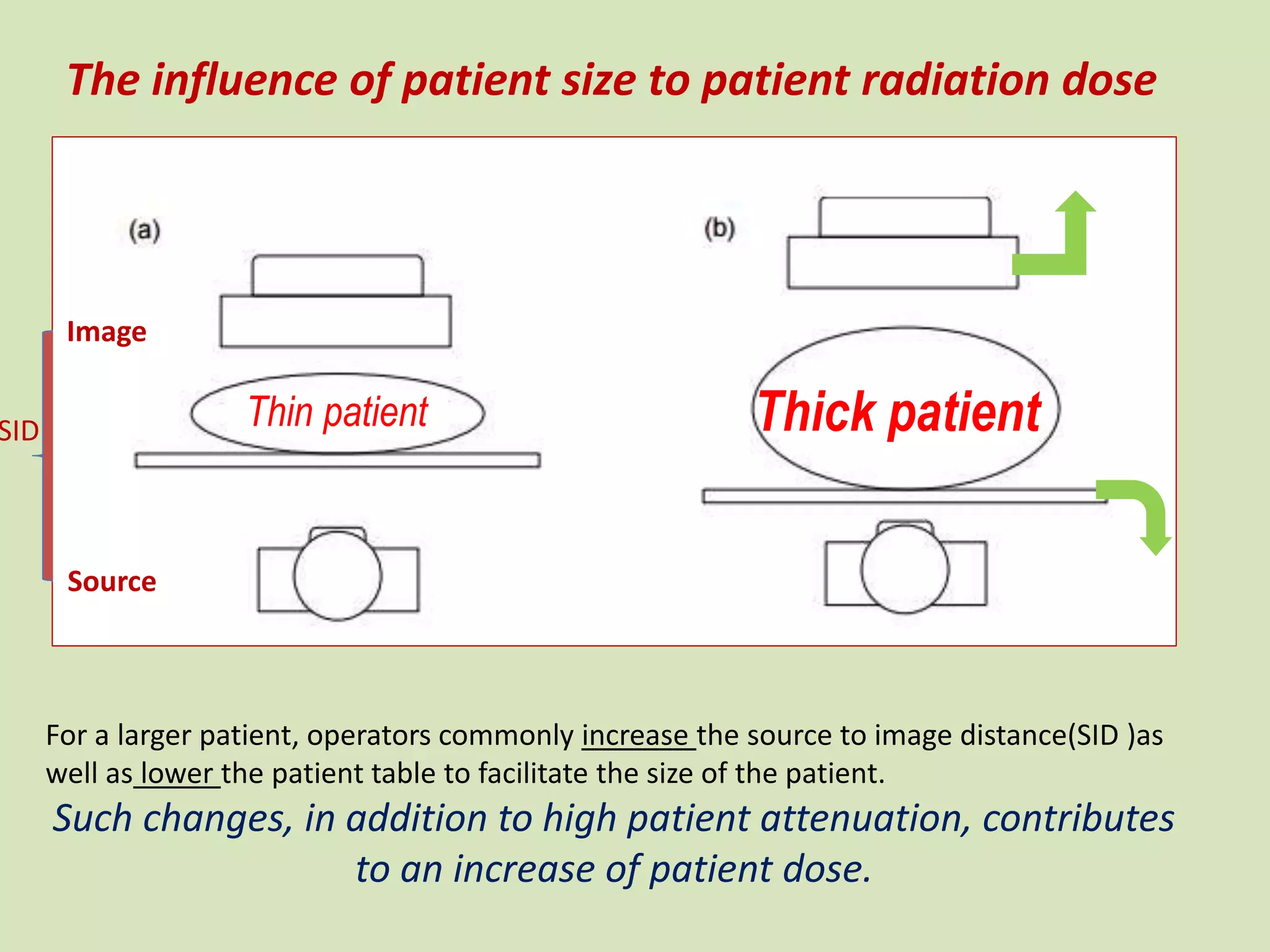
The document discusses radiation safety in the cardiac cath lab, highlighting the risks of ionizing radiation exposure to both operators and patients. It outlines radiation measurement units, occupational exposure risks, and methods for optimizing safety, such as using protective equipment, proper patient positioning, and real-time dose monitoring. Strategies to reduce exposure include minimizing use of fluoroscopy and cine imaging, utilizing collimation, and ensuring appropriate shielding and distance from radiation sources.