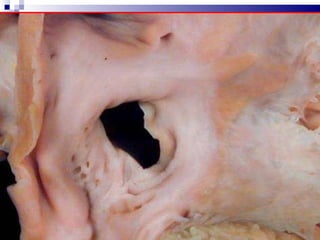
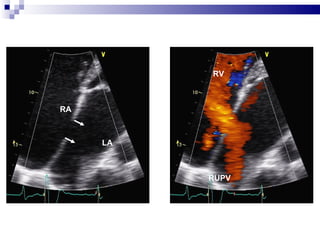
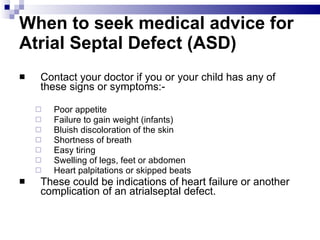
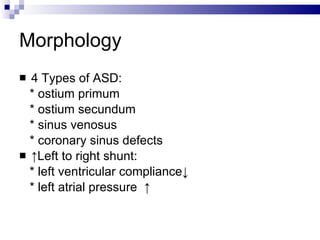
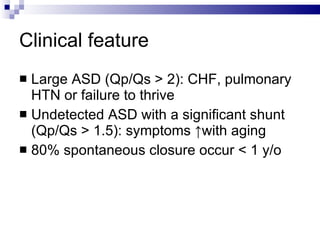
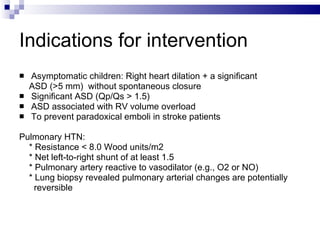
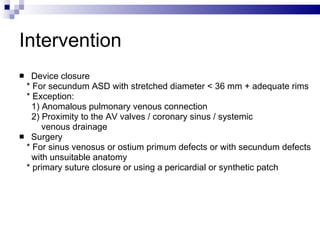
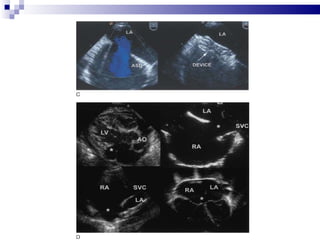
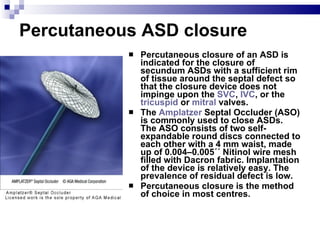
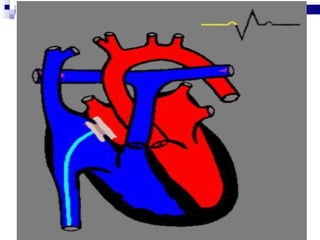
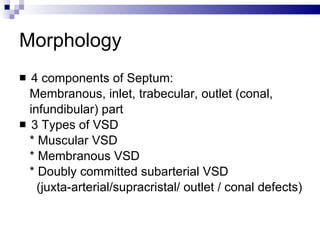
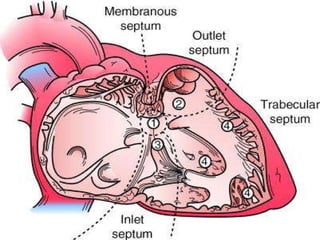
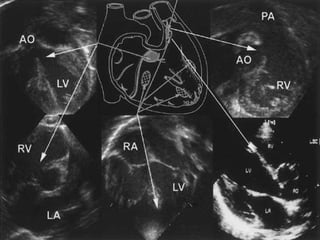
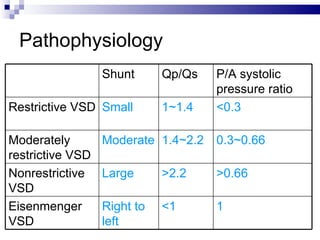
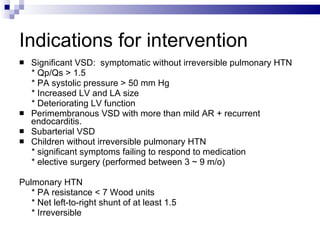
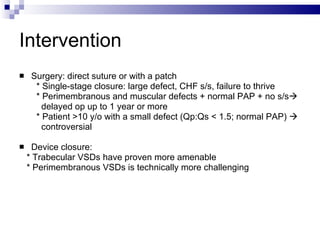
The document discusses non-surgical interventions for atrial septal defects (ASDs) and ventricular septal defects (VSDs). It describes the anatomy, causes, symptoms, and types of ASDs and VSDs. It provides indications for intervention such as large defect size, heart failure, or failure to thrive. The main non-surgical interventions discussed are percutaneous device closure of ASDs and VSDs, which are preferred to surgery when the anatomy is suitable. The future of interventions may include improved 3D imaging, contrast agents, and stents to repair more complex congenital heart defects.