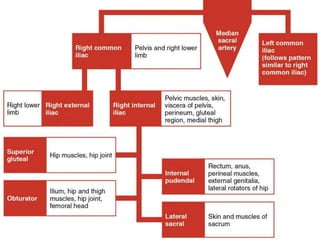
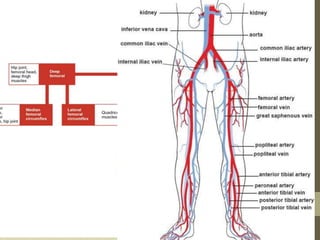
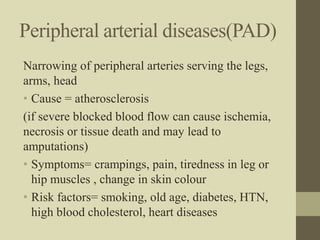
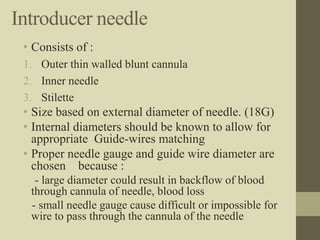
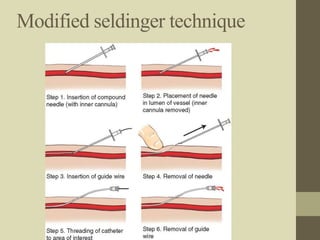
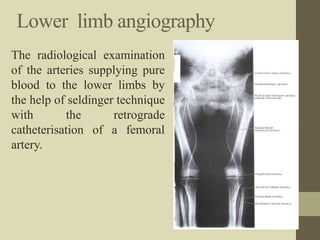
Peripheral angiography is a radiological procedure used to examine arteries and veins after injecting contrast media. It involves puncturing an artery such as the femoral artery using the Seldinger technique and threading a catheter over a guidewire to inject contrast media and obtain images. The procedure is used to diagnose and treat various vascular conditions. Precise positioning, sterile equipment and contrast injection are needed to obtain diagnostic images of the peripheral vasculature.